Combining AI Models Improves Breast Cancer Risk Assessment
Released: August 29, 2023
At A Glance
- Combining diagnostic and texture-based AI models results in improved interval and long-term breast cancer risk assessment.
- The combined AI model was tested on more than 119,000 women in a breast cancer screening program.
- The model also enabled identification of women at high risk for breast cancer.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Combining artificial intelligence (AI) systems for short- and long-term breast cancer risk results in an improved cancer risk assessment, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA).
Most breast cancer screening programs take a one-size-fits-all approach and follow the same protocols when it comes to determining a woman’s lifetime risk of developing breast cancer. Using mammography-based deep learning models may improve the accuracy of breast cancer risk assessment and can also lead to earlier diagnoses.
“About 1 in 10 women develop breast cancer throughout their lifetime,” said study author Andreas D. Lauritzen, Ph.D., from the Department of Computer Science at the University of Copenhagen in Denmark. “In recent years, AI has been studied for the purpose of diagnosing breast cancer earlier by automatically detecting breast cancers in mammograms and measuring the risk of future breast cancer.”
A variety of AI tools exist to aid in detecting cancer risk. Diagnostic AI models are trained to detect suspicious lesions on mammograms and are well suited to estimate short-term breast cancer risk.
More suitable for long-term breast cancer risk are texture AI models, capable of identifying breast density. Women with dense breast tissue are at higher risk of developing breast cancer and may benefit from supplemental MRI screening.
“It is important to enable reliable and robust assessment of breast cancer risk using information from the screening mammogram,” Dr. Lauritzen said.
For this study, Dr. Lauritzen and his research team sought to identify whether a commercially available diagnostic AI tool and an AI texture model, trained separately and then subsequently combined, may improve breast cancer risk assessment.
The researchers used the diagnostic AI tool Transpara and a texture model that was developed by the researchers. A Dutch training set of over 39,000 exams was used to train the models. The short- and long-term risk models were combined using a three-layer neural network.
The combined AI model was tested on a study group of more than 119,000 women who were included in a breast cancer screening program in the Capital Region of Denmark between November 2012 and December 2015. The average age of the women was 59 years.
Compared to the diagnostic and texture models alone, the combined AI model showed an overall improved risk assessment for both interval and long-term cancer detection. Interval cancers are those that are found between routine screenings.
The model also enabled identification of women at high risk for breast cancer. Women identified by the combined model as having the 10% highest combined risk accounted for 44.1% of interval cancers and 33.7% of long-term cancers.
Using AI to identify a women’s breast cancer risk from a single mammogram will not only result in earlier cancer detection but can also improve the strain on the health care system due to the worldwide shortage of specialized breast radiologists.
“Current state-of-the-art clinical risk models require multiple tests such as blood work, genetic testing, mammogram and filling out extensive questionnaires, all of which would substantially increase the workload in the screening clinic,” Dr. Lauritzen said. “Using our model, risk can be assessed with the same performance as the clinical risk models but within seconds from screening and without introducing overhead in the clinic.”
“Assessing Breast Cancer Risk by Combining AI for Lesion Detection and Mammographic Texture.” Collaborating with Dr. Lauritzen were My C. von Euler-Chelpin, Ph.D., Elsebeth Lynge, Ph.D., Ilse Vejborg, Ph.D., Mads Nielsen, Ph.D., Nico Karssemeijer, Ph.D., and Martin Lillholm, Ph.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology’s legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
Video (MP4):

Video 1. Andreas D. Lauritzen, Ph.D., discusses his research “Combining AI Models Improves Breast Cancer Risk Assessment”
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
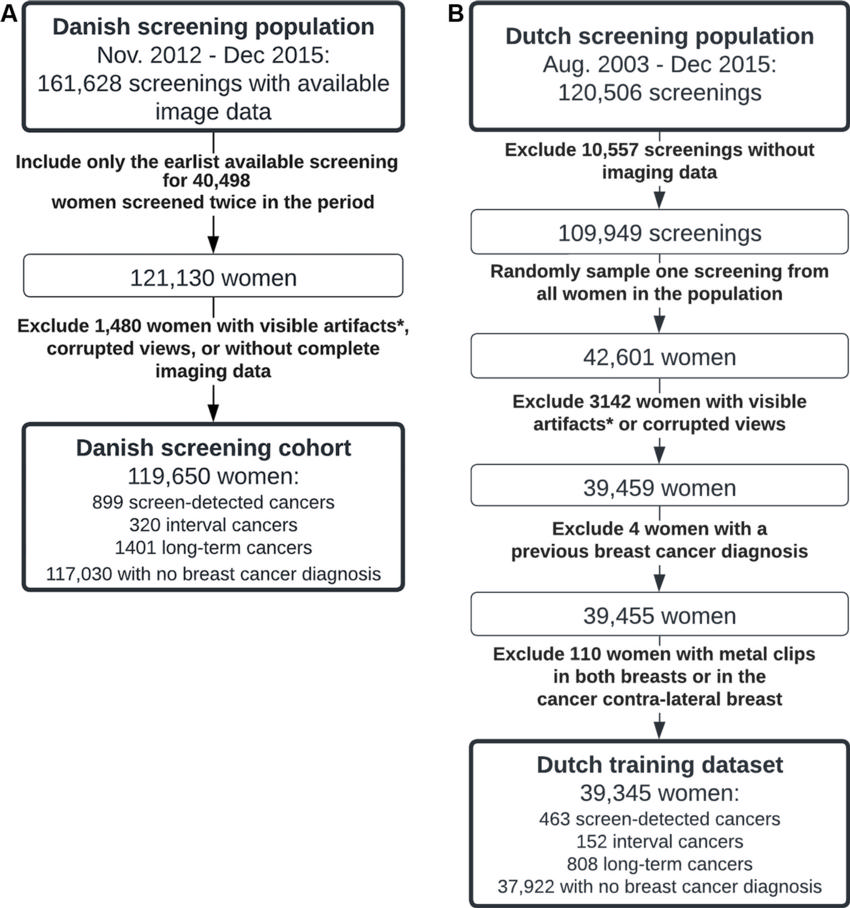
Figure 1. Flow diagrams show data collection processes for the (A) Danish screening cohort and (B) Dutch training data set. * = visible artifacts such as foreign objects, implanted medical devices, and miscellaneous disruptive image artifacts.
High-res (TIF) version
(Right-click and Save As)
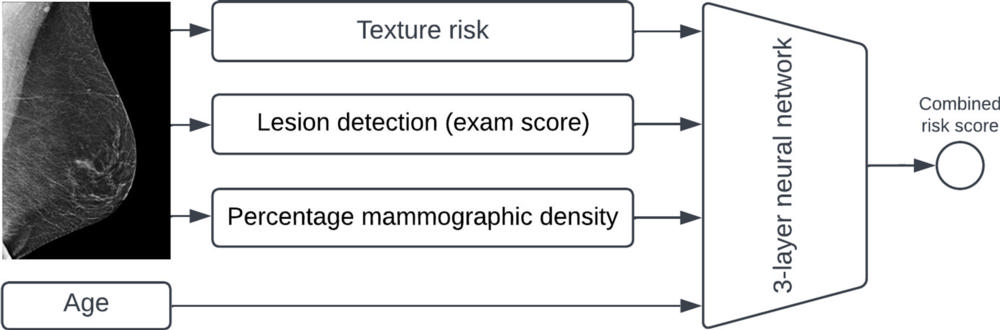
Figure 2. Schematic shows components of the combination model. A mammogram is individually evaluated by the diagnostic artificial intelligence algorithm for lesions (examination score); by the mammographic texture model for textures associated with long-term cancer risk (texture score), which is combined with the presence of clips to generate texture risk; and for percentage mammographic density. Percentage mammographic density is estimated as the amount of dense tissue of the total breast area using a deep learning segmentation tool. These three risk covariates, as well as age, are combined using a three-layer neural network into a single continuous risk estimate referred to as the combined risk.
High-res (TIF) version
(Right-click and Save As)
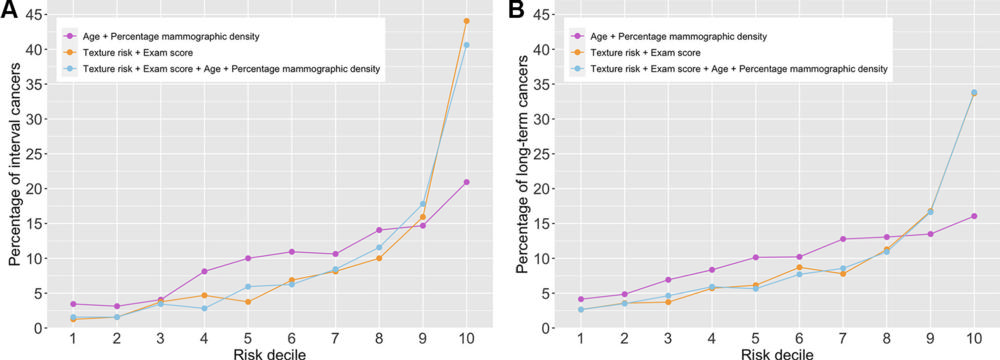
Figure 3. Line graphs show the percentage of (A) interval cancers and (B) long-term cancers in each risk decile as determined by the following three models: the baseline model aggregating age and percentage mammographic density; the combination model with texture risk and the examination score; and the combination model with texture risk, the examination score, age, and percentage mammographic density.
High-res (TIF) version
(Right-click and Save As)
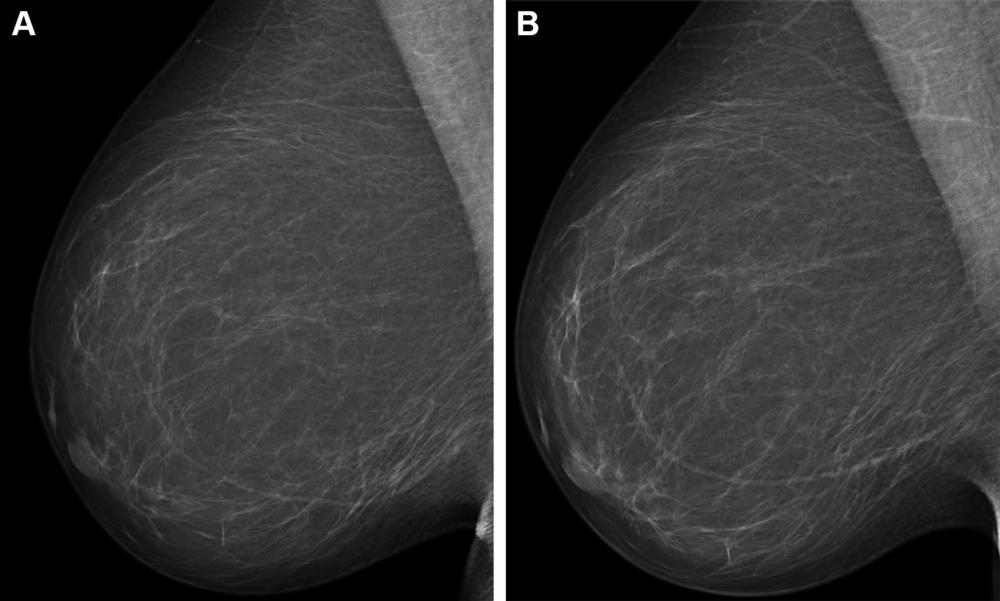
Figure 4. Full-field digital mammograms (right mediolateral oblique view) in a 59-year-old woman show (A) the screening mammogram obtained during the study period and (B) the screening mammogram obtained in the subsequent screening round. The first screening mammogram (A) had a very low combined risk score (lowest 0.1%) as determined by the combination model with texture risk and the examination score. The woman was not recalled and did not receive a breast cancer diagnosis throughout the 5-year follow-up.
High-res (TIF) version
(Right-click and Save As)
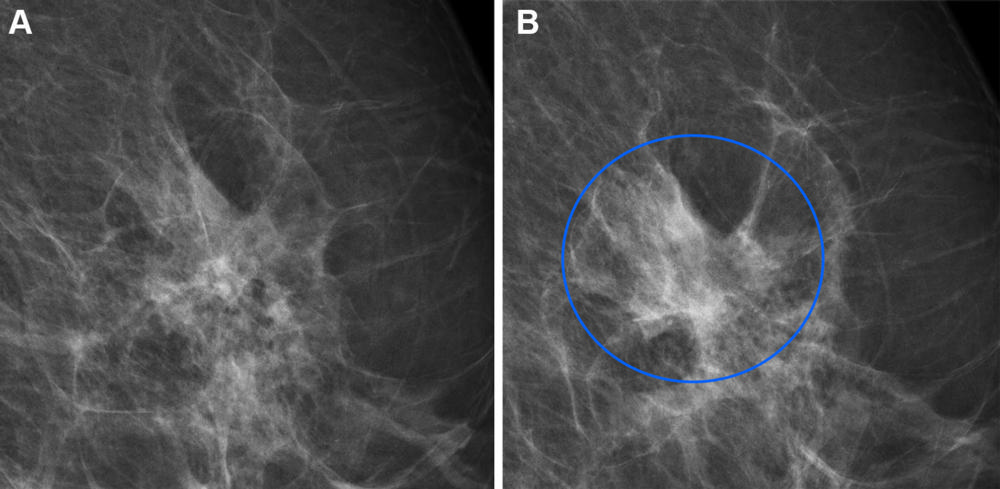
Figure 5. Full-field digital mammograms (left mediolateral oblique view) in a 60-year-old woman with an interval cancer show (A) the screening mammogram at the area of interest and (B) the same area of interest on a clinical mammogram obtained during diagnostic testing a year later, whereby the blue circle indicates the diagnosed lesion. The woman was not recalled as a result of screening. The screening mammogram (A) had a very high combined risk score (highest 99%) as determined by the combination model with texture risk and the examination score.
High-res (TIF) version
(Right-click and Save As)
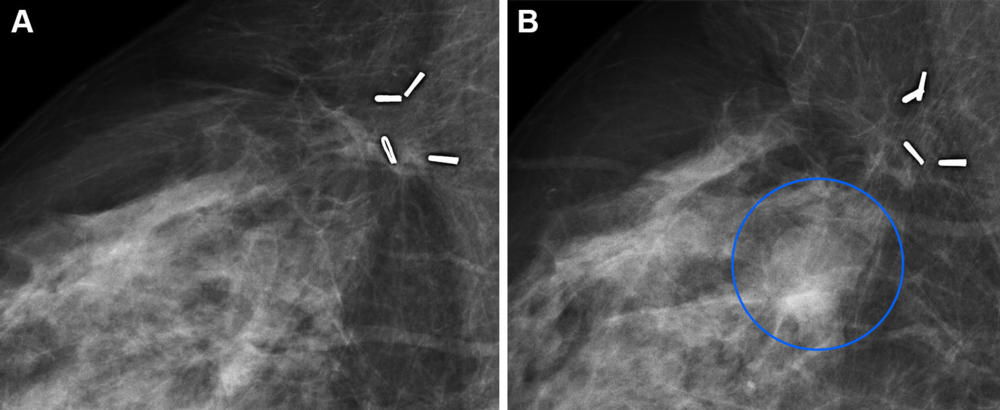
Figure 6. Full-field digital mammograms (right mediolateral oblique view) in a 59-year-old woman with a long-term cancer show (A) the screening mammogram at the area of interest and (B) the same area of interest on a clinical mammogram obtained during diagnostic testing 3 years later, whereby the blue circle indicates the diagnosed lesion. The woman was not recalled as a result of screening. The screening mammogram (A) had a very high combined risk score (highest 99.9%) as determined by the combination model with texture risk and the examination score. The four objects are surgical clips left in the breast from previous breast-conserving surgery.
High-res (TIF) version
(Right-click and Save As)
