MRI Shows Potential to Improve Breast Cancer Risk Prediction
Released: May 12, 2015
At A Glance
- Researchers reviewed screening breast MRI exams of high-risk women 18 years or older with no history of breast cancer.
- Women who displayed elevated amounts of background parenchymal enhancement (BPE) on MRI were nine times more likely to have breast cancer diagnosed during the study follow-up interval.
- The results suggest that BPE could potentially help physicians better tailor screening and management strategies to each individual’s breast cancer risk.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Emma Day
1-630-590-7791
eday@rsna.org
OAK BROOK, Ill. – Magnetic resonance imaging (MRI) provides important information about a woman's future risk of developing breast cancer, according to a new study published in Radiology. Researchers said the findings support an expanded role for MRI in more personalized approaches to breast cancer screening and prevention.
The new study focused on the relationship between imaging features and cancer risk in women who already face a high risk of breast cancer because of family history, genetic mutations associated with the disease, or other factors. In prior studies, dense breast tissue, or tissue that contains more fibroglandular tissue than fatty tissue, has been linked to an increased likelihood of breast cancer development.
"To date, it's been difficult to assess the future risk of breast cancer for women, so there is a strong desire in the oncology community to identify ways to better determine this risk," said study co-author Habib Rahbar, M.D., a breast imaging expert at Seattle Cancer Care Alliance and assistant professor at the University of Washington. "While breast density is loosely associated with the risk of developing breast cancer, it is unclear whether it or other imaging features can improve upon current risk assessment methods."
Contrast-enhanced MRI is one potential tool that is already used as an imaging option to supplement mammography in high-risk women. Current American Cancer Society guidelines recommend that women with a 20 percent or greater lifetime risk of developing breast cancer undergo annual screening breast MRIs in addition to routine annual screening mammography.
In the new study, Dr. Rahbar and colleagues reviewed screening breast MR images from high-risk women 18 years or older with no history of breast cancer who were screened at their institution from January 2006 to December 2011.
The researchers looked for any associations between cancer risk and imaging features, including breast density and background parenchymal enhancement (BPE). BPE is a phenomenon in which areas of normal background breast tissue appear white, or enhanced, on the MR images. The precise reasons for this enhancement are not clear, but previous research has suggested a possible link to cancer risk.
The results showed that women who displayed elevated amounts of BPE on MRI were nine times more likely to have a breast cancer diagnosis during the study follow-up interval than those who exhibited no or minimal BPE. In contrast, mammographic density appeared to have no significant relationship to cancer risk in the study group.
The findings suggest that BPE could potentially help physicians better tailor screening and management strategies to each individual's breast cancer risk. Currently, women at high risk for breast cancer have various options, including supplementing screening mammography with MRI, prevention therapy with tamoxifen—a drug that blocks estrogen activity in the breast—and preventive mastectomies. If validated in larger studies, BPE could provide more information to help guide these important decisions.
"MRI could be used in a broader group of women to determine who most needs supplemental screening based on their BPE levels," Dr. Rahbar said. "This is important as we move into an era of more personalized medicine."
The researchers are working to validate the findings in a larger group of patients and are planning additional research to understand more about why BPE may serve as a biomarker of breast cancer risk. One theory is that BPE is related to areas of inflammation associated with early stages of the disease.
"Breast cancer needs a supportive environment to grow, and recent research suggests that areas of inflammation are particularly conducive for such growth," Dr. Rahbar said.
"Are Qualitative Assessments of Background Parenchymal Enhancement, Amount of Fibroglandular Tissue on MR Images, and Mammographic Density Associated with Breast Cancer Risk?" The study was led by Dr. Rahbar and Brian N. Dontchos, M.D., a recent Roger E. Moe Fellow in Multidisciplinary Breast Cancer Care at the University of Washington School of Medicine, and was funded by grants from the International Society for Magnetic Resonance in Medicine and the National Institutes of Health (R01CA151326).
Collaborating with Drs. Rahbar and Dontchos were Savannah C. Partridge, Ph.D., Larissa A. Korde, M.D, Ph.D., Diana L. Lam, M.D., John R. Scheel, M.D., Ph.D., Sue Peacock, M.Sc., and Constance D. Lehman, M.D., Ph.D.
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org)
RSNA is an association of more than 54,000 radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on breast MRI, visit RadiologyInfo.org.
Images (.JPG and .TIF format)

Figure 1. Examples of varying amounts of background parenchymal enhancement (BPE), as prospectively assessed qualitatively. Axial postcontrast maximum intensity projection MR images show (a) minimal, (b) mild, (c) moderate, and (d) marked BPE
High-res (TIF) version
(Right-click and Save As)

Figure 2. Examples of background parenchymal enhancement (BPE) patterns, as assessed retrospectively, with observers blinded to clinical outcomes. Axial T1-weighted postcontrast fat-saturated images show (a) BPE with a predominantly central pattern and (b) BPE with a predominantly peripheral pattern.
High-res (TIF) version
(Right-click and Save As)

Figure 3. Examples of varying amounts of fibroglandular tissue (FGT) on breast MR images, as assessed retrospectively, with observers blinded to known mammographic densities. Axial T1-weighted images show examples of breast composition described as (a) almost entirely fat, (b) scattered fibroglandular, (c) heterogeneous, and (d) extreme amount of FGT.
High-res (TIF) version
(Right-click and Save As)
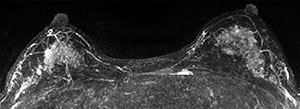
Figure 4. Contrast-enhanced maximum intensity projection in a 41-year-old woman with a family history of breast cancer shows marked background parenchymal enhancement . This patient was found to have invasive ductal carcinoma 183 days after index MR imaging.
High-res (TIF) version
(Right-click and Save As)
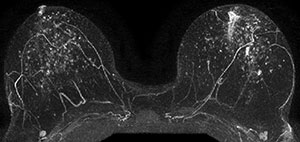
Figure 5. Postcontrast maximum intensity projection in a 48-year-old woman with a genetic history of breast cancer and prior excisional biopsy in the left breast shows moderate background parenchymal enhancement. A diagnosis of invasive ductal carcinoma was made 1044 days after index MR imaging.
High-res (TIF) version
(Right-click and Save As)
