Shorter MRI Exam Effectively Detects Cancer in Dense Breasts
Released: May 20, 2025
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — Abbreviated breast MRI shortens exam time while retaining a high level of diagnostic accuracy of breast cancer in women with extremely dense breasts, according to an article published today in Radiology, a journal of the Radiological Society of North America (RSNA).
Women with extremely dense breasts have a high proportion of dense glandular and fibrous tissue and very little fatty tissue. This can be a risk factor for breast cancer due to the similar appearance of tumors and dense breast tissue on mammograms.
Supplemental MRI screening is generally recommended for women with extremely dense breasts.
"Compared to mammography, breast MRI, whether abbreviated or full protocol, has a higher diagnostic accuracy for women with extremely dense breasts," said study author Wouter B. Veldhuis, M.D., Ph.D., an associate professor in the Department of Radiology at the University Medical Center at Utrecht University in the Netherlands.
Although breast MRI has a high cancer detection rate, the additional costs and time associated with the procedure have impacted the widespread implementation of breast MRI in women with extremely dense breasts.
A conventional full-protocol breast MRI can take an average of 30 to 35 minutes to complete, while an abbreviated breast MRI can take as little as 10 minutes. Reducing the scan time of full protocol breast MRI through abbreviated breast MRI may lower the cost of the procedure.
Dr. Veldhuis and colleagues conducted a secondary analysis on a subset of MRI exams from the Netherlands-based Dense Tissue and Early Breast Neoplasm Screening (DENSE) Trial to assess the minimal protocol necessary to maintain high accuracy in detecting breast cancer.
Seven radiologists, each with a minimum of 16 years of experience, read the same set of screening breast MRI exams with 4 different sequences added incrementally, resulting in a total of 2,072 reads.
After each MRI sequence, the radiologists provided a Breast Imaging Reporting and Data System (BI-RADS) score to determine the necessity for recall for further testing.
The researchers found that the abbreviated MRI protocol had comparable sensitivity and specificity to the full protocol MRI. Furthermore, the results of the study showed that the addition of more sequences did not provide any additional diagnostic information for making a recall or no-recall decision.
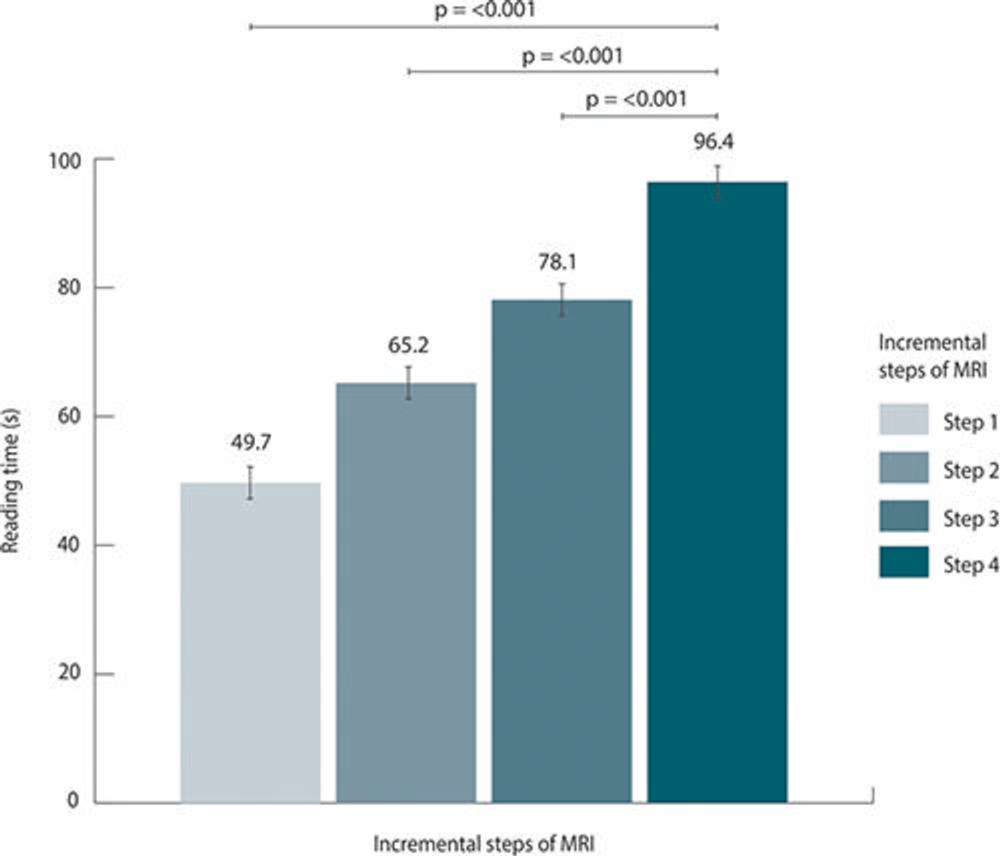
Both scan and reading times of the abbreviated MRIs were dramatically reduced, resulting in up to 80% shorter scan times and 50% shorter pooled reading times. The shortest scan time was under five minutes.
"The shortest abbreviated protocol demonstrated good performance, comparable to that of the full multiparametric protocol, while being up to four times faster to acquire and up to two times faster to read," Dr. Veldhuis noted.
The researchers note that the shorter reading and scan times of abbreviated breast MRI could enable more women to be screened within a shorter timeframe while also making it a more accessible and comfortable experience for patients.
"Reducing the examination time and noise levels potentially improves patient experience," Dr. Veldhuis said. "Moreover, shorter reading and scan times may allow implementation of MRI in national screening programs making it available for all women with extremely dense breasts."
"Multireader Diagnostic Accuracy of Abbreviated Breast MRI for Screening Women with Extremely Dense Breasts." Collaborating with Dr. Veldhuis were Sophie E. L. van Grinsven, Ritse M. Mann, M.D., Ph.D., Evelyn M. Monninkhof, Ph.D., Katya Duvivier, M.D., Mathijn D. F. de Jong, M.D., Petra K. de Koekkoek-Doll, M.D., Claudette E. Loo, M.D., Ph.D., Ruud M. Pijnappel, M.D., Ph.D., Rogier van der Sluijs, Jeroen Veltman, M.D., Ph.D., and Carla H. van Gils, Ph.D., for the DENSE Trial Study Group.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast MRI, visit RadiologyInfo.org.
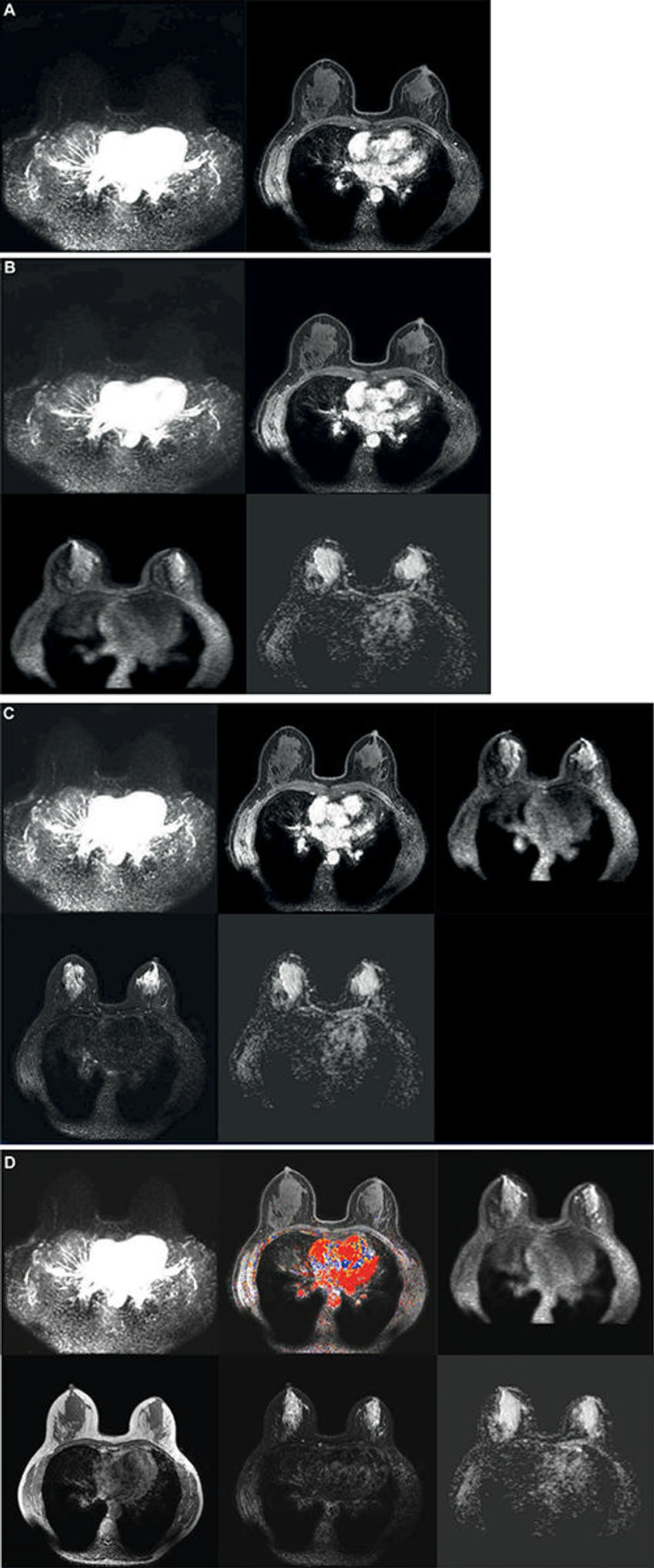
Figure 1. Axial images show the incremental steps 1–4. (A) Step 1: The first step consisted of the dual high-temporal low-spatial and low-temporal high-spatial dynamic T1 series, from before contrast material injection to 120 seconds after contrast injection only. (B) Step 2: The second step added diffusion-weighted images to the series available from step 1. (C) Step 3: The third step added T2-weighted images to the series available from steps 1 and 2. (D) Step 4: The fourth and final step added non–fat-saturated T1-weighted precontrast images, all remaining dynamic phases acquired after the first 120 seconds after contrast administration, and enhancement curve kinetics to the series available from steps 1, 2, and 3. This final step is the full multiparametric breast MRI protocol that was used in the Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial. The curve kinetics overlay is a colormap showing the standard three types of delayed curve kinetics: type-I kinetics, persistent increase (blue); type-II kinetics, plateau (yellow); and type-III kinetics, washout (red).
High-res (TIF) version
(Right-click and Save As)
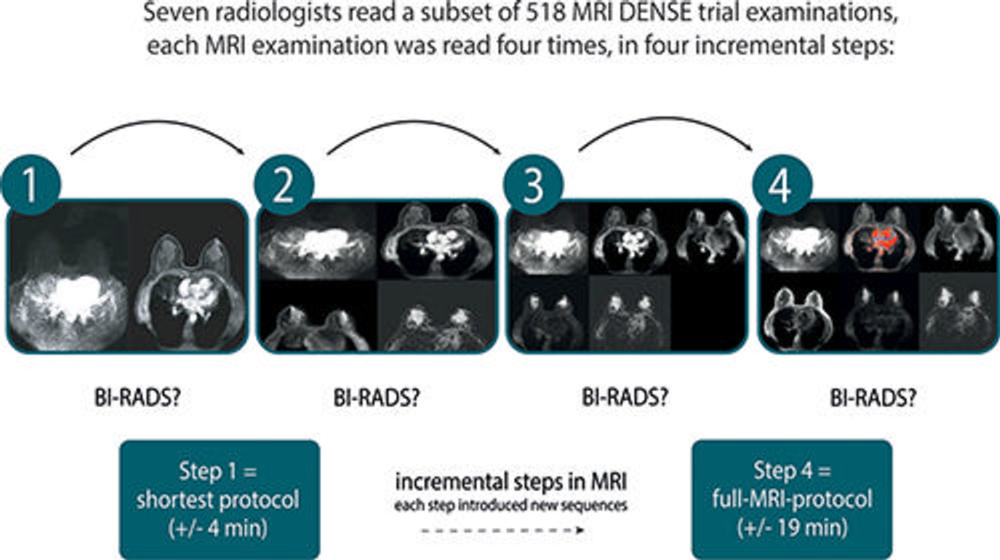
Figure 2. Schematic shows the reading procedure of this multireader, multicase study. Each radiologist assessed the same 518 MRI examinations in four incremental steps (steps 1–4), each step adding additional sequences to those from the preceding step. BI-RADS = Breast Imaging Reporting and Data System, DENSE = Dense Tissue and Early Breast Neoplasm Screening.
High-res (TIF) version
(Right-click and Save As)
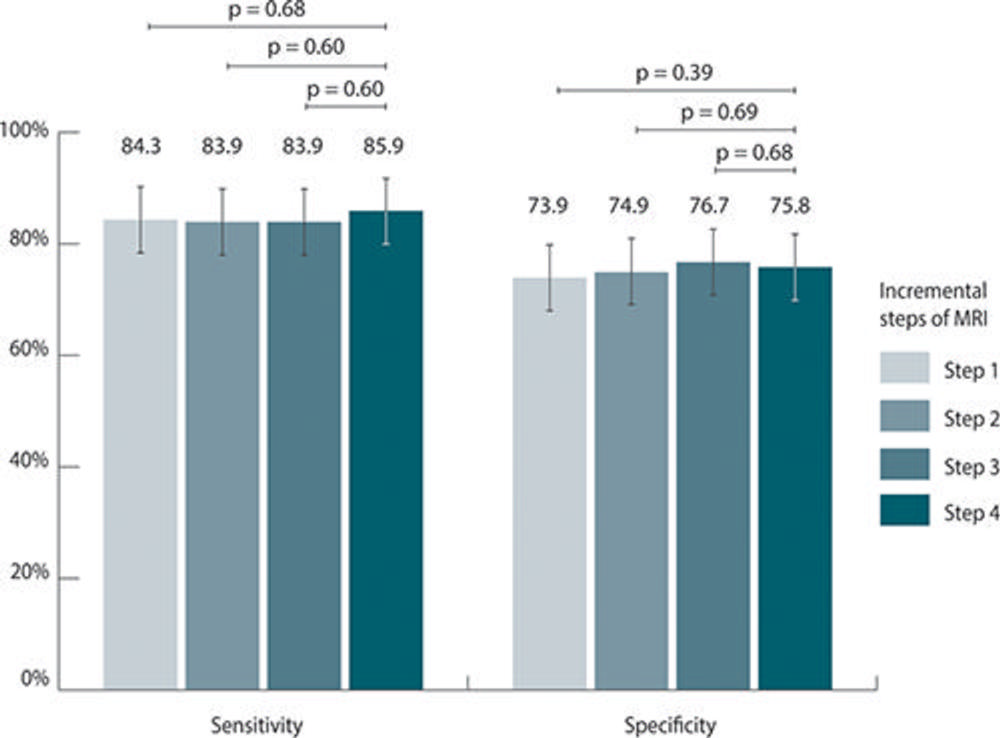
Figure 3. Bar graphs show pooled sensitivity and specificity per incremental steps of MRI. There was no evidence of a difference in both sensitivity and specificity between the abbreviated protocols and full MRI protocol.
High-res (TIF) version
(Right-click and Save As)
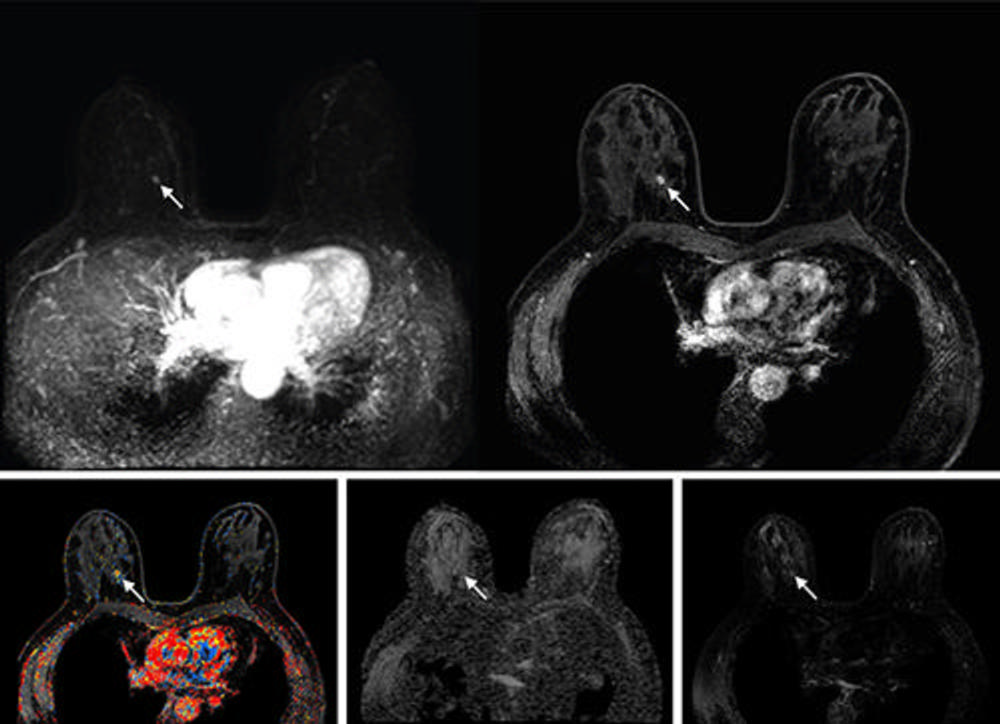
Figure 4. Abbreviated axial MRI images show a 6-mm irregular mass with an irregular margin (arrows) in the right upper inner quadrant with early rapid enhancement. The lesion was assessed as Breast Imaging Reporting and Data System (or BI-RADS) category 4 (suspicious for cancer). The participant was recalled and underwent US-guided core-needle biopsy that showed invasive carcinoma of no special type. On the full-protocol sequences (not shown), the lesion was T2-weighted hypointense and showed diffusion restriction and washout kinetics in the delayed phase, characteristics that, although are all confirmative of the malignant nature of the lesion, offered no additional value for making the recall decision.
High-res (TIF) version
(Right-click and Save As)
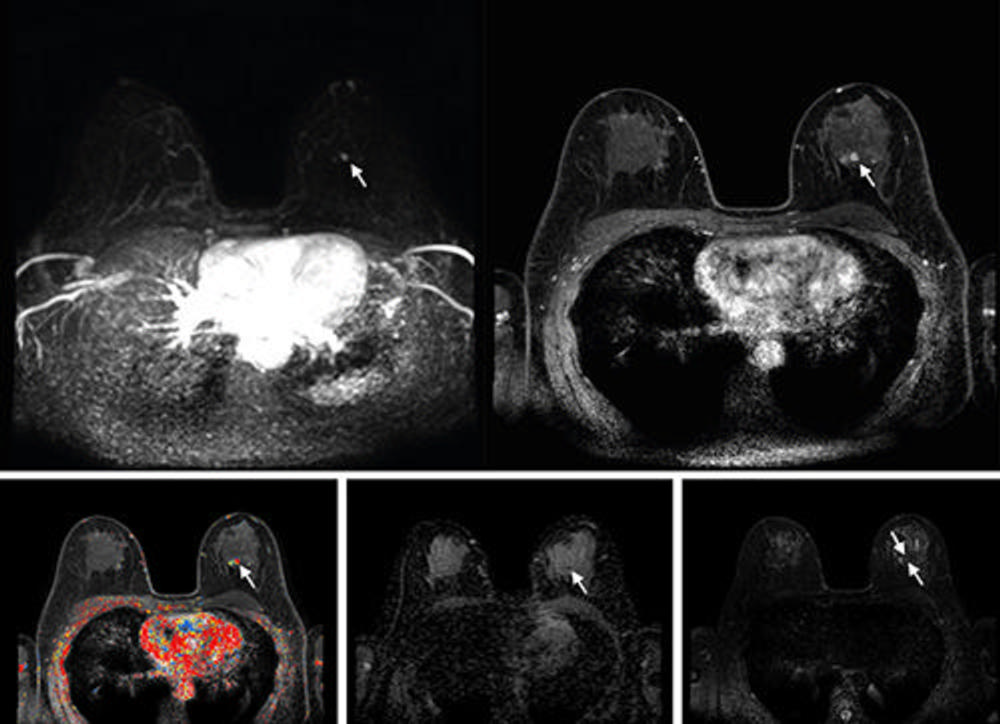
Figure 5. Abbreviated axial MRI images show a 7-mm irregular mass with irregular margin (arrows) in the right upper inner quadrant with early rapid enhancement (Breast Imaging Reporting and Data System category 4 [suspicious for cancer]). The participant was recalled and underwent an MRI-guided vacuum-assisted biopsy that showed sclerosing adenosis with microcalcifications and usual ductal hyperplasia and focal apocrine metaplasia. On the full-protocol images (not shown), the lesion was T2-weighted hypointense and showed diffusion restriction and washout kinetics in the delayed phase, characteristics that would not have reversed the decision to recall the participant.
High-res (TIF) version
(Right-click and Save As)