Virus That Causes COVID-19 Increases Risk of Cardiac Events
Released: February 04, 2025
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — A new study found severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was associated with the rapid growth of plaque in the coronary arteries and an increased risk of cardiovascular events. The results were published today in Radiology, a journal of the Radiological Society of North America (RSNA).
“COVID-19, caused by SARS-CoV-2, is initially characterized by acute lung injury and respiratory failure,” said the study’s senior author, Junbo Ge, M.D., professor and director of the Cardiology Department at Zhongshan Hospital, Fudan University in Shanghai, China. “However, emerging evidence indicates COVID-19 also involves an extreme inflammatory response that can affect the cardiovascular system.”
According to Dr. Ge, this systemic inflammation produces consequences for the heart beyond the first month of infection, leading to high mortality and unfavorable outcomes.
The researchers investigated the impact of SARS-CoV-2 infection using coronary CT angiography (CCTA) to assess coronary inflammation, determined by analyzing changes in tissue surrounding the coronary arteries, as well as plaque burden and type.
The retrospective study included patients who underwent CCTA between September 2018 and October 2023. The final study group of 803 patients (mean age, 63.9 years, 543 men) included 329 patients (41%) imaged before the COVID-19 pandemic and 474 patients imaged during the pandemic. Of those, 25 patients were infected with SARS-CoV-2 before imaging.
The research team analyzed a total of 2,588 coronary artery lesions, including 2,108 lesions among SARS-CoV-2 patients and 480 lesions among uninfected patients.
For all patients, researchers compared baseline and follow-up measurements of plaque volume changes, the presence of high-risk plaque and inflammation. They also analyzed the relationship between SARS-CoV-2 and cardiovascular events, such as a heart attack or revascularization procedure.
At baseline, the mean stenosis, or narrowing of the artery, per lesion was 31.3%. Only 8.1% of lesions had diameter stenosis of 50% or more.
Compared to the uninfected patients, the plaque volumes grew faster in SARS-CoV-2 patients. Lesions in patients with SARS-CoV-2 infection had a higher incidence of developing into high-risk plaques (20.1% versus 15.8%) and coronary inflammation (27% versus 19.9%). Patients with COVID-19 also had a higher risk of target lesion failure (10.4% versus 3.1%), an indicator of increased heart attack or stroke risk.
“Inflammation following COVID-19 can lead to ongoing plaque growth, particularly in high-risk, noncalcified plaques.” Dr. Ge said. “Patients with SARS-CoV-2 infection are at increased risk for myocardial infarction, acute coronary syndrome and stroke for up to a year.”
He added that these effects persist during the aftermath of COVID-19, regardless of comorbidities such as age, hypertension, and diabetes.
“Effective management strategies for these patients are imperative,” Dr. Ge said.
The findings suggest that SARS-CoV-2 infection may exacerbate cardiovascular risk by accelerating the progression of susceptible plaques and coronary inflammation. However, a more comprehensive understanding of the biological mechanisms is required to formulate preventative and therapeutic approaches.
“It’s crucial to anticipate a heavier cardiovascular patient burden in the future as most infected individuals recover from acute SARS-CoV-2 infection,” Dr. Ge said.
“SARS-CoV-2 Infection Association with Atherosclerotic Plaque Progression at Coronary CT Angiography and Adverse Cardiovascular Events.” Collaborating with Dr. Ge were Neng Dai, M.D., Xianglin Tang, M.D., Yiqing Hu, M.D., Hao Lu, M.D., Zhangwei Chen, M.D., Shaofeng Duan, Ph.D., Weifeng Guo, M.D., Pranav Prakash Edavi, M.D., Yongfu Yu, Ph.D., Dong Huang, M.D., and Juying Qian, M.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on CT angiography, visit RadiologyInfo.org.
Images (JPG, TIF):
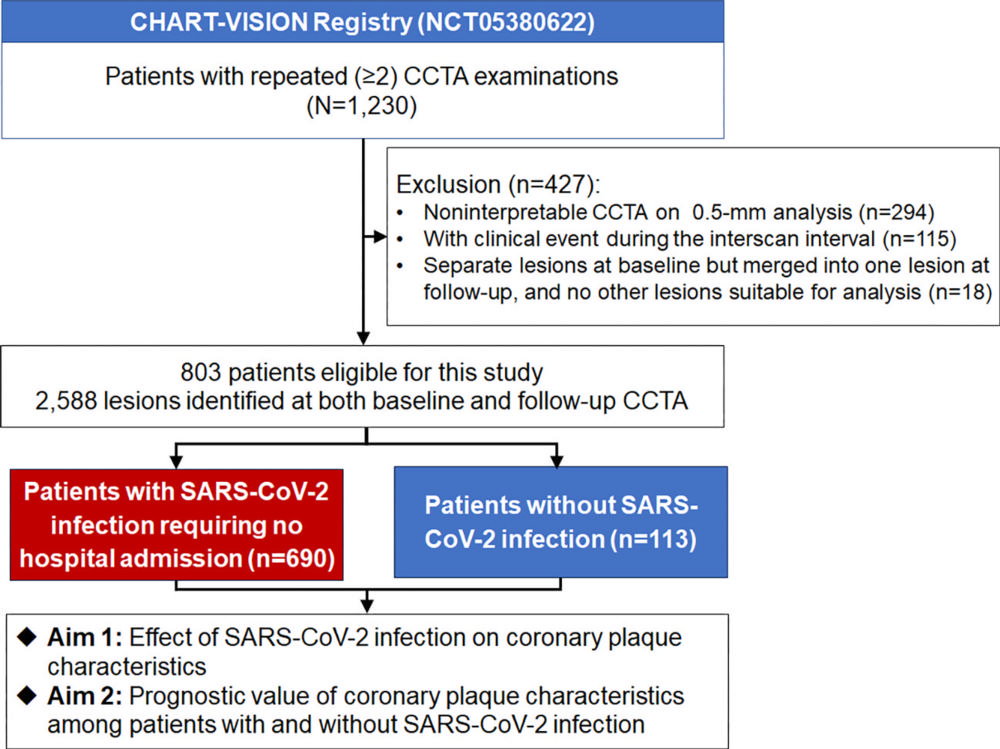
Figure 1. Study inclusion and exclusion flowchart. The CHART-VISION registry (CHART Study of Coronary CT Angiography in Coronary Artery Disease, ClinicalTrials.gov registration no. NCT05380622) describes the natural history of coronary atherosclerotic plaque development and progression or regression and plaque characterization and phenotypes over time at coronary CT angiography (CCTA) among deferred coronary lesions.
High-res (TIF) version
(Right-click and Save As)
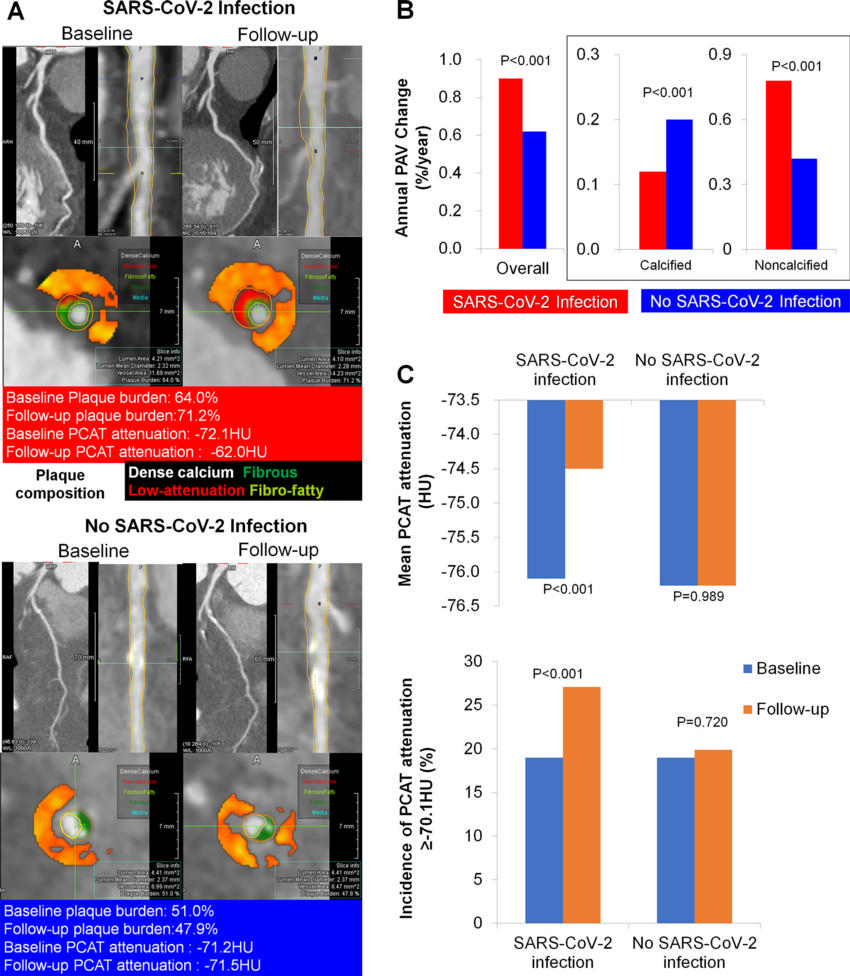
Figure 2. Temporal changes in the composition of plaque volumes and fat attenuation index according to SARS-CoV-2 infection status. (A) Representative coronary CT angiography images of lesions at baseline and follow-up, (B) annualized change in overall and percent atheroma volume (PAV) by composition according to SARS-CoV-2 infection status, and (C) mean pericoronary adipose tissue (PCAT) and presence of PCAT of −70.1 HU or more at baseline and follow-up according to SARS-CoV-2 infection status.
High-res (TIF) version
(Right-click and Save As)
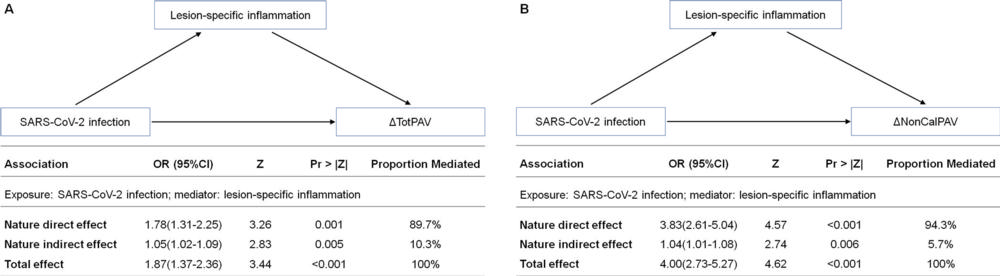
Figure 3. Effect of SARS-CoV-2 infection on plaque progression mediated by inflammation. Causal mediation analysis was used to examine whether the impact of SARSCoV- 2 infection on the (A) annual change in total percent atheroma volume (ΔTotPAV) and (B) annual change in noncalcified percent atheroma volume (ΔNonCalPAV) was mediated by lesion-specific inflammation. Under a counterfactual framework, the total effect of SARS-CoV-2 infection on the annual change in total percent atheroma volume or annual change in noncalcified percent atheroma volume can be decomposed into direct effects and indirect effects through lesion-specific inflammation. OR = odds ratio, Pr = probability, Z = regression coefficient test statistic.
High-res (TIF) version
(Right-click and Save As)
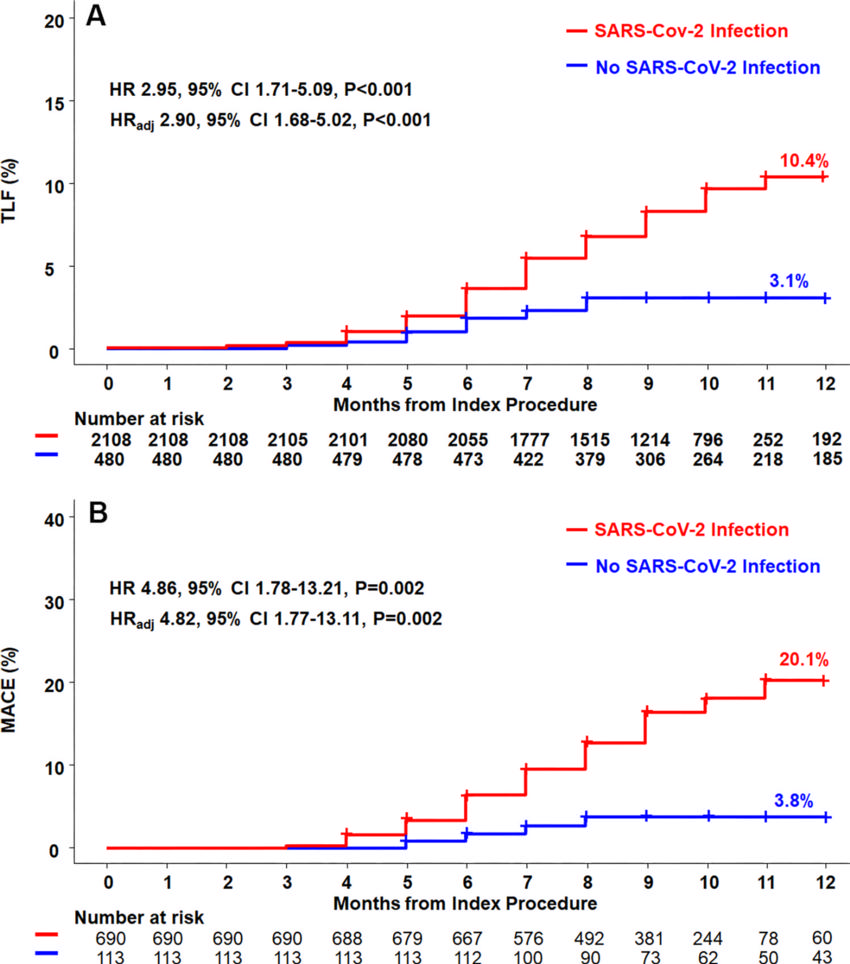
Figure 4. Graphs show the cumulative incidence of adverse events according to SARS-CoV-2 infection status Kaplan-Meier curves and cumulative incidence of clinical outcomes at the (A) per-lesion and (B) per-patient levels. Target lesion failure (TLF) is a composite of cardiac death, target lesion myocardial infarction, and clinically driven target lesion revascularizations. Major adverse cardiovascular events (MACEs) were a composite of death from any cause, myocardial infarction, and hospitalization for unstable angina. Multivariable adjustment was performed for age, sex, hypertension, dyslipidemia, diabetes mellitus, history of smoking, total percent atheroma volume (PAV), low-density lipoprotein level at baseline, and use of antiplatelet and lipid-lowering therapy. HR = hazard ratio, HRadj = adjusted hazard ratio.
High-res (TIF) version
(Right-click and Save As)
