Climate Change Exposure Associated with Increased Emergency Imaging
Released: November 19, 2024
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — Using data collected over a 10-year period from four emergency departments, researchers at the University of Toronto found that short-term exposure to ambient heat and air pollution levels was associated with increased utilization of X-rays and computed tomography (CT). Results of the study were published today in Radiology, a journal of the Radiological Society of North America (RSNA).
"Extreme climate exposures are associated with higher demand for health care including emergency department visits," said Kate Hanneman, M.D., M.P.H., vice chair and associate professor at the University of Toronto, Department of Medical Imaging, and deputy lead of sustainability at the Joint Department of Medical Imaging at Toronto General Hospital. "However, the impact of climate-related environmental exposure on medical imaging utilization is currently unknown."
In the retrospective study, the research team analyzed the association between daily imaging utilization counts at four emergency departments in academic hospitals in Toronto, Canada, and local daily ambient environmental data between 2013 and 2022. A time-stratified, case-crossover design was used to control for seasonality, time trends, influence by day of the week, and covariates including age, sex, race and behavioral risk factors.
For the purposes of the study, high heat was defined as a mean ambient temperature greater than 68 degrees Fahrenheit. A high level of air pollution was defined as the presence of fine particulate matter (PM2.5) at levels greater than 12 μg/m3.
Over the study period, 1,666,420 medical imaging exams were performed in the four emergency departments with a mean of 428 exams daily. The mean for daily emergency department visits was 659. The average mean daily ambient temperature was 48.2 degrees (range, -7°F to 85°F), and the mean daily ambient particulate matter was 7.9 μg/m3.
The researchers found that short-term (fewer than seven days) exposures to higher ambient (outdoor) heat and higher PM2.5 air pollution were associated with overall increases in imaging utilization (5.1% and 4.0%, respectively). High heat exposure days and high air pollution exposure days were associated with excess absolute risk of 5.5 and 6.4 imaging studies per 1 million people at risk per day, respectively.
"While the individual daily effects we observed are modest, the cumulative increase in total imaging volumes is substantial," Dr. Hanneman said.
Over the study period, there were 602 high-heat exposure days and 552 unhealthy high air pollution days. High heat exposure increased by 0.6% (2.2 days) per year while high PM2.5 days decreased by 0.4% (1.3 days) per year over the study period.
"This is consistent with overall improved air quality in Canada and the U.S. over the last two decades attributed to policies aimed at regulating air pollution and the phasing out of coal plants in Ontario," Dr. Hanneman said. "Despite the decrease in high air pollution days, PM2.5 remains a health threat."
Heat and air pollution were associated with increased utilization of X-rays and CT, but not ultrasound or MR. High temperatures had a greater effect on X-ray utilization, while high PM2.5 levels were associated with higher CT utilization. Both environmental exposures were associated with increased utilization of chest, neuro and musculoskeletal imaging.
Increased imaging utilization associated with ambient heat was a function of higher emergency department visits, whereas increased utilization related to high PM2.5 levels was a function of both increased patient volumes and increased per-patient imaging.
Dr. Hanneman said data from the study may help radiology departments prepare for and build resiliency to the current and future impacts of climate change.
"As global temperatures continue to rise, the frequency and severity of heat waves and extreme weather events are expected to increase," she said. "Knowing the impact on our departments will allow us to plan proactively."
The research was supported by an RSNA Research & Education Foundation Emerging Issues Grant.
"Increased Emergency Department Medical Imaging: Association with Short-Term Exposures to Ambient Heat and Particulate Air Pollution." Collaborating with Dr. Hanneman were Omar Taboun, B.Sc., M.Sc., Anish Kirpalani, M.D., Birgit Ertl-Wagner, M.D., Ph.D., Julien Aguet, M.D., Scott Delaney, Sc.D., J.D., M.P.H., Rachel C. Nethery, Ph.D., Joseph Choi, M.D., M.P.H., Hayley Panet, M.H.Sc., C.H.E., M.R.T. (MR), Maura J. Brown, M.D., Heidi Schmidt, M.D., Ania Kielar, M.D., and Michael Patlas, M.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on emergency imaging, visit RadiologyInfo.org.
Images (JPG, TIF):

Figure 1. Diagram summarizes study purpose, design, setting, outcome, short-term environmental exposures (up to lag of 7 days), results, and conclusion. PM2.5 = fine particulate matter with 2.5 μm or smaller aerodynamic diameter.
High-res (TIF) version
(Right-click and Save As)
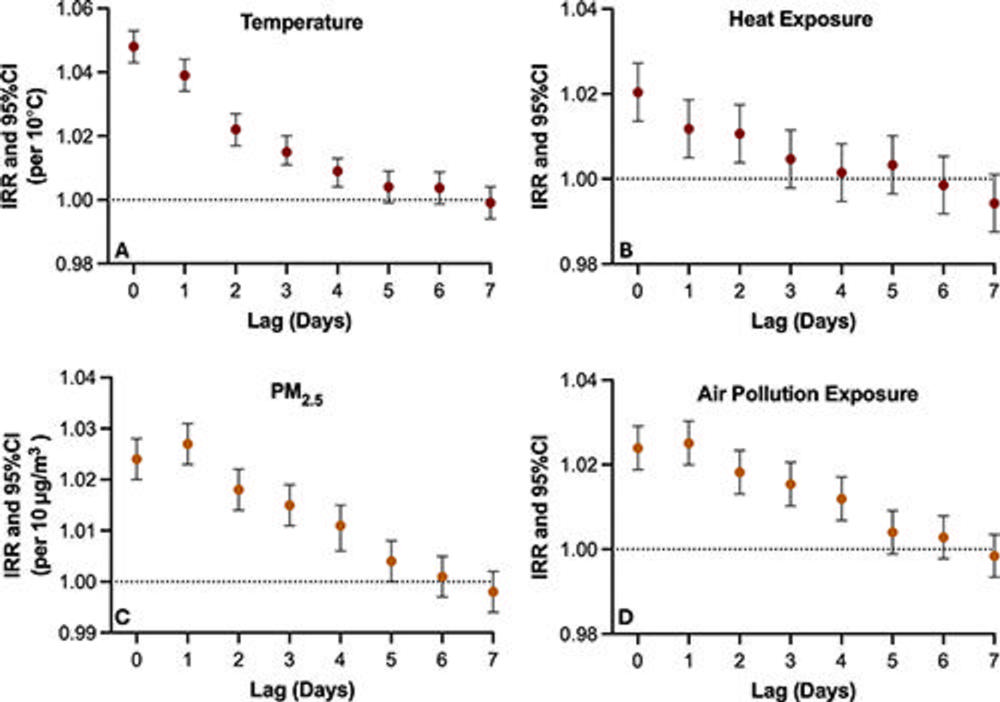
Figure 2. Dot plots show lagged (delayed) associations (up to lag of 7 days) between short-term environmental exposures and total daily emergency department medical imaging utilization, including (A) mean daily ambient temperature (per 10 °C rise), (B) heat exposure days (defined as ambient mean daily temperature >20 °C), (C) mean daily ambient fine particulate matter with 2.5-μm or smaller aerodynamic diameter (PM2.5) (per 10-μg/m3 rise), and (D) air pollution exposure days (defined as mean daily PM2.5 >12 μg/m3). Dots indicate incidence rate ratios (IRRs) for environmental exposures at each lag day, with whiskers representing the 95% CI. The dotted line indicates an IRR of 1 (no effect).
High-res (TIF) version
(Right-click and Save As)

Figure 3. Dot plots show the association between short-term environmental exposures and daily emergency department medical imaging utilization stratified by modality (radiography, CT, US, and MRI), including (A) 2-day moving average of mean ambient temperature (per 10 °C rise), (B) heat exposure days (defined as ambient mean daily temperature >20 °C), (C) 3-day moving average of mean daily ambient fine particulate matter with 2.5-μm or smaller aerodynamic diameter (PM2.5) (per 10-μg/m3 rise), and (D) air pollution exposure days (defined as mean daily PM2.5 >12 μg/m3). Dots indicate incidence rate ratios (IRRs) for environmental exposures for each imaging modality, with whiskers representing the 95% CI. The dotted line indicates an IRR of 1 (no effect).
High-res (TIF) version
(Right-click and Save As)
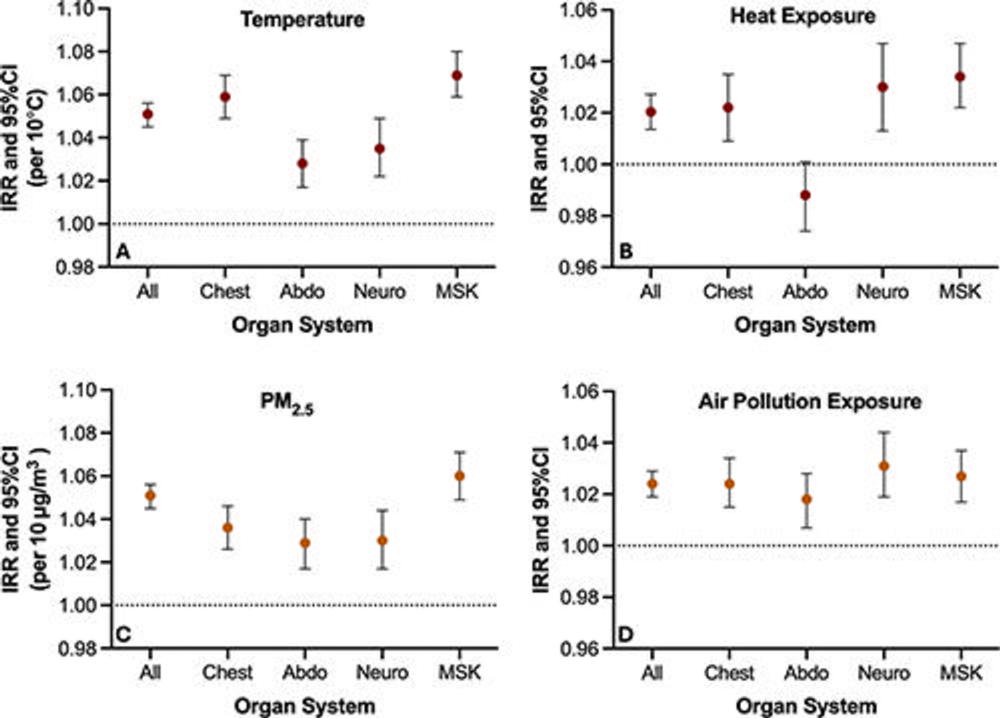
Figure 4. Dot plots show the association between short-term environmental exposures and daily emergency department medical imaging utilization stratified by organ system, including (A) 2-day moving average of mean ambient temperature (per 10 °C rise), (B) heat exposure days (defined as ambient mean daily temperature >20 °C), (C) 3-day moving average of mean daily ambient fine particulate matter with 2.5-μm or smaller aerodynamic diameter (PM2.5) (per 10-μg/m3 rise), and (D) air pollution exposure days (defined as mean daily PM2.5 >12 μg/m3). Dots indicate incidence rate ratios (IRRs) for environmental exposures for imaging of each organ system, with whiskers representing the 95% CI. The dotted line indicates an IRR of 1 (no effect). Abdo = abdominal, MSK = musculoskeletal, neuro = neuroimaging.
High-res (TIF) version
(Right-click and Save As)
