Access to Patient Questionnaire Improves Spine MRI Diagnosis
Released: October 29, 2024
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — Knowing a patient’s symptoms helps radiologists in lumbar spine MRI interpretation and diagnosis, according to a study published today in Radiology, a journal of the Radiological Society of North America (RSNA).
MRI is the most important imaging exam in patients with back pain or sciatica because it shows nearly all degenerative and structural abnormalities of the spine.
However, MRI often shows spinal abnormalities in individuals who do not have symptoms. Because the same abnormalities can occur in both symptomatic and asymptomatic individuals, it is impossible to distinguish an incidental MRI finding from the true cause of pain by only looking at the MRI.
To diagnose the true cause of pain, it is critical to match the MRI abnormalities with patients’ symptoms. Since radiologists may not have access to detailed, high-quality symptom information at the time of MRI interpretation, their reports usually list all the spinal abnormalities without specifying the one most likely causing symptoms.
“MRI exams of the lumbar spine often show many degenerative abnormalities. Most of these are incidental findings that do not cause pain,” said study author William E. Palmer, M.D., division chief of Musculoskeletal Radiology at Massachusetts General Hospital (Mass General) in Boston. “To diagnose the true pain generators and make the best treatment decisions, symptoms must be matched with MRI abnormalities.”
Patients at Mass General complete a short symptom questionnaire prior to their lumbar spine MRI. They answer questions about the severity of their pain, where it is located, what makes it worse, and what makes it better.
“The questionnaire is important because it obtains symptom information directly from patients and communicates it to radiologists at the time of lumbar spine MRI interpretation,” Dr. Palmer said.
Dr. Palmer and colleagues sought to determine exactly how beneficial patient-reported symptom information is at the time of MRI interpretation.
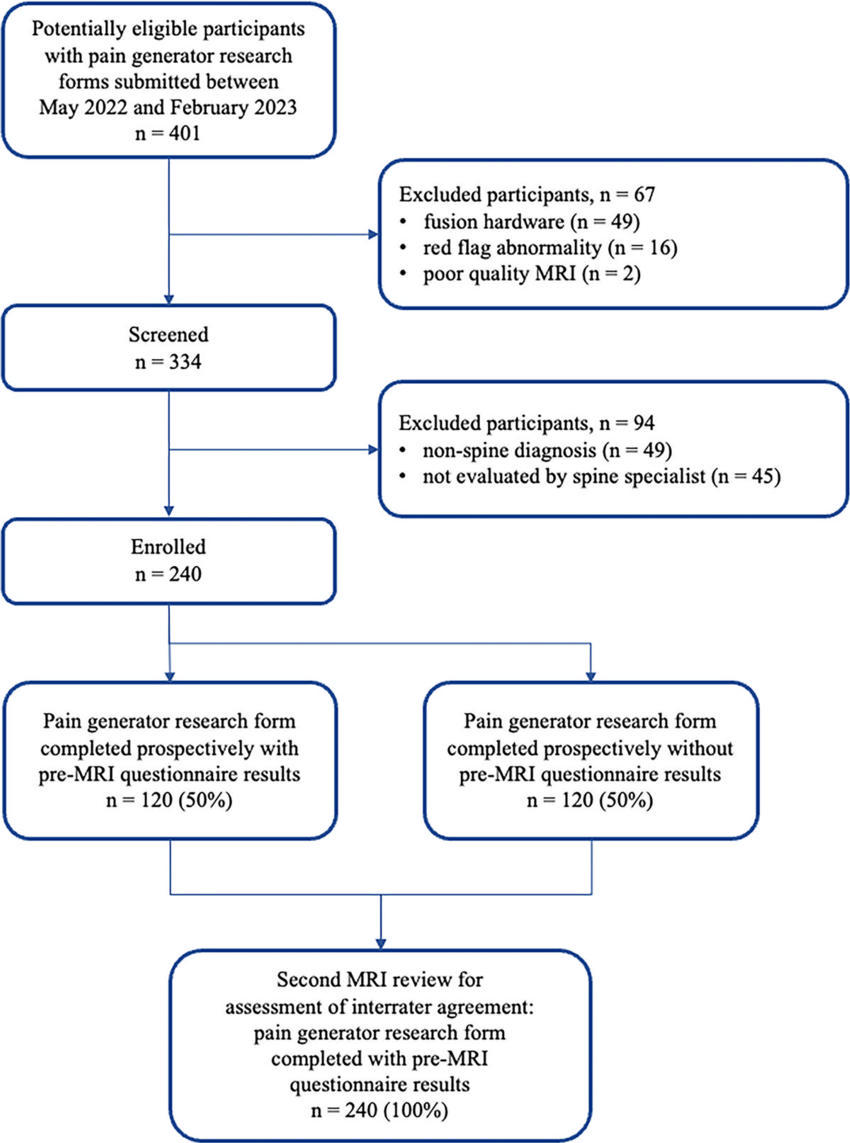
For this prospective, multi-reader study, the investigators included a total of 240 Mass General patients who completed a symptom questionnaire prior to their lumbar spine MRI.
Musculoskeletal radiologists ranging from 2 to 24 years of experience alternated the reading of MRIs with or without symptom information from the questionnaire. Their diagnoses were then compared to the diagnoses of spine specialists, who conducted face-to-face interviews with patients to make their assessments and decide on treatments.
Radiologists who had access to questionnaire information during MRI interpretation achieved a near statistically perfect agreement with spine specialists.
MRI interpretations without patient-reported symptom information resulted in a significant decrease in diagnostic accuracy and confidence. The questionnaire helped to avoid diagnostic discrepancies between radiologists and spine specialists.
“By distinguishing actionable pain generators from incidental findings, radiologists can best help primary care physicians who depend on MRI reports to guide their treatments and referrals,” Dr. Palmer said.
“Impact of Patient-reported Symptom Information on the Interpretation of MRI of the Lumbar Spine.” Collaborating with Dr. Palmer were Rene Balza, M.D., Sarah F. Mercaldo, Ph.D., Ambrose J. Huang, M.D., Jad S. Husseini, M.D., Mohamed Jarraya, M.D., F. Joseph Simeone, M.D., and Joao R. T. Vicentini, M.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on spine MRI, visit RadiologyInfo.org.
Video (MP4):

Video William E. Palmer, M.D., discusses his research on the impact of patient-reported symptom information on the interpretation of MRI of the lumbar spine.
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
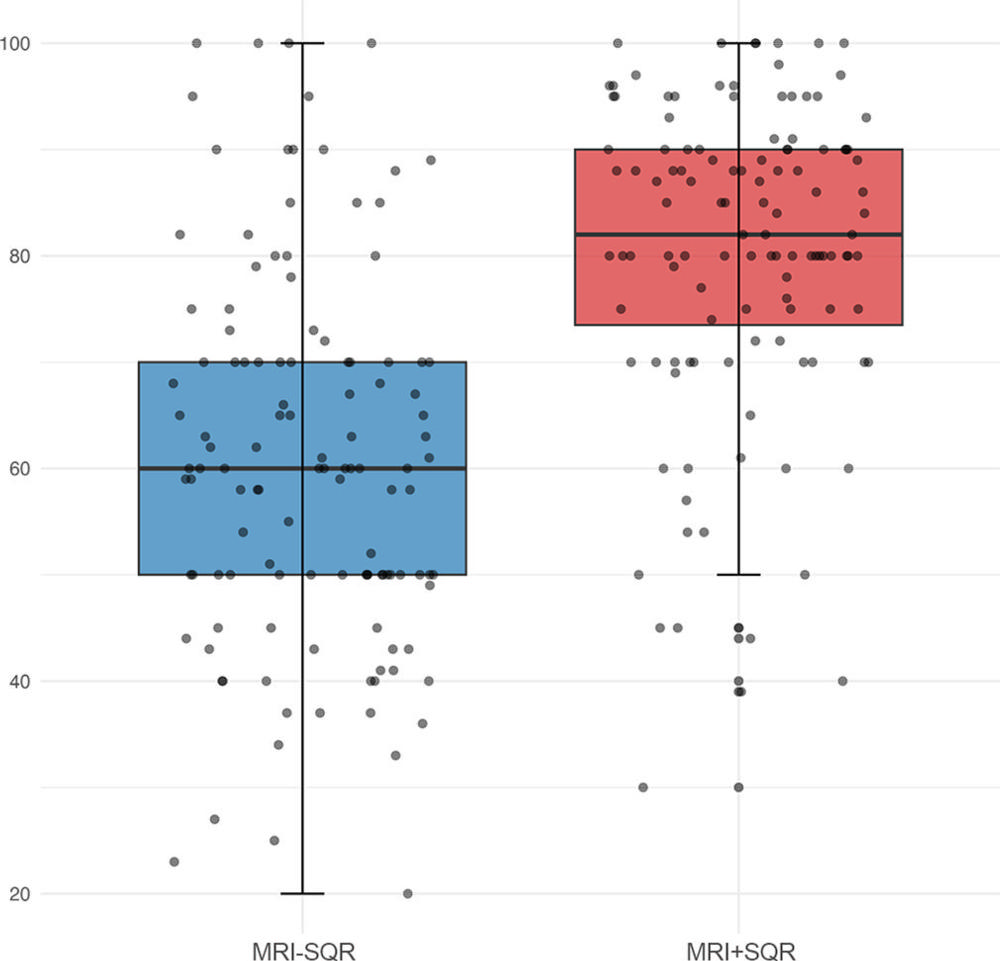
Figure 2. Box plot of diagnostic certainty levels (0–100, where 0 indicates no certainty and 100 denotes absolute certainty). Boxes show median value (horizontal line within boxes) and IQR. Whiskers depict the range of values within 1.5 times the IQR. The points represent actual certainty values in each group. SQR = symptom questionnaire results, MRI-SQR = MRI diagnoses without symptom questionnaire results, MRI+SQR = MRI diagnoses with symptom questionnaire results.
High-res (TIF) version
(Right-click and Save As)
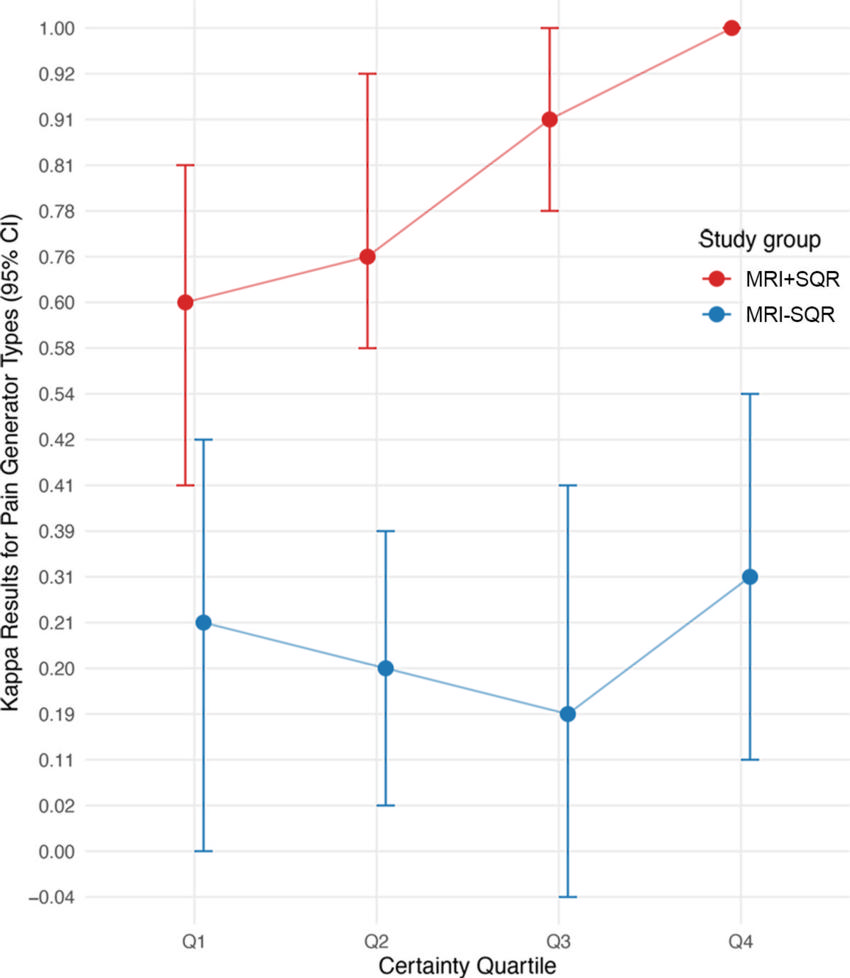
Figure 3. Graphs shows mean κ values for the pain-generator types according to certainty quartiles. Quartile 1 (Q1) to quartile 4 (Q4) represent four subgroups sorted by certainty level, where Q1 denotes the lowest 25% of certainty levels and Q4 denotes the highest 25% of certainty levels. In MRI with symptom questionnaire results (MRI+SQR), certainty level quartiles are less than 74, 74–82, 83–90, and greater than 90. In MRI without SQR (MRI-SQR), certainty level quartiles are less than 50, 50–60, 61–70, and greater than 70. The error bars depict 95% CIs. For MRI with SQR, mean κ values are higher in Q4 than Q1. For MRI without SQR, κ values show no evidence of a significant difference (P = .53).
High-res (TIF) version
(Right-click and Save As)
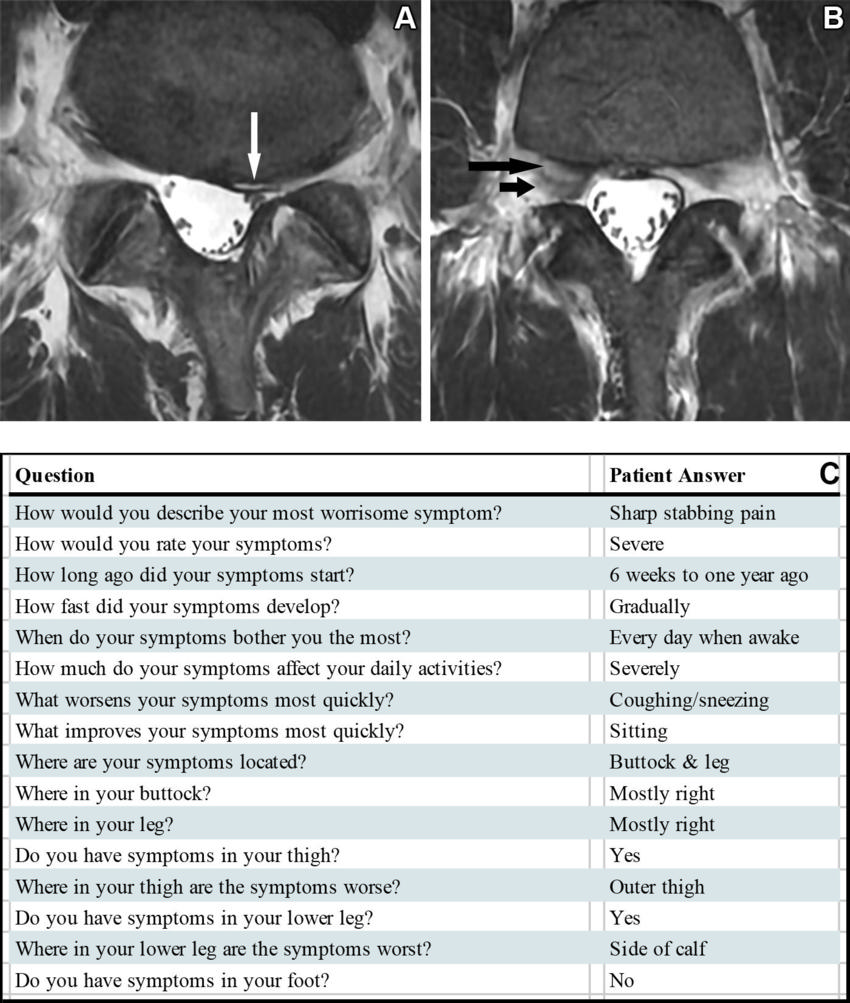
Figure 4. (A, B) Axial T2-weighted fast spin-echo MRI scans in a 42-year-old male participant with lumbar spine symptoms. (A) On MRI scan without knowledge of symptom questionnaire results (SQR), the pain generator was misdiagnosed as subarticular zone stenosis (arrow) at L5-S1 level on the left. (B) On MRI scan with SQR, the pain generator was diagnosed as foraminal stenosis at L4-5 level on the right, agreeing with diagnosis made by spine specialist. Intraforaminal disk extrusion (long arrow) compresses right L4 dorsal root ganglion (short arrow). (C) Pre-MRI symptom questionnaire indicates the character and location of right-sided buttock and leg pain.
High-res (TIF) version
(Right-click and Save As)
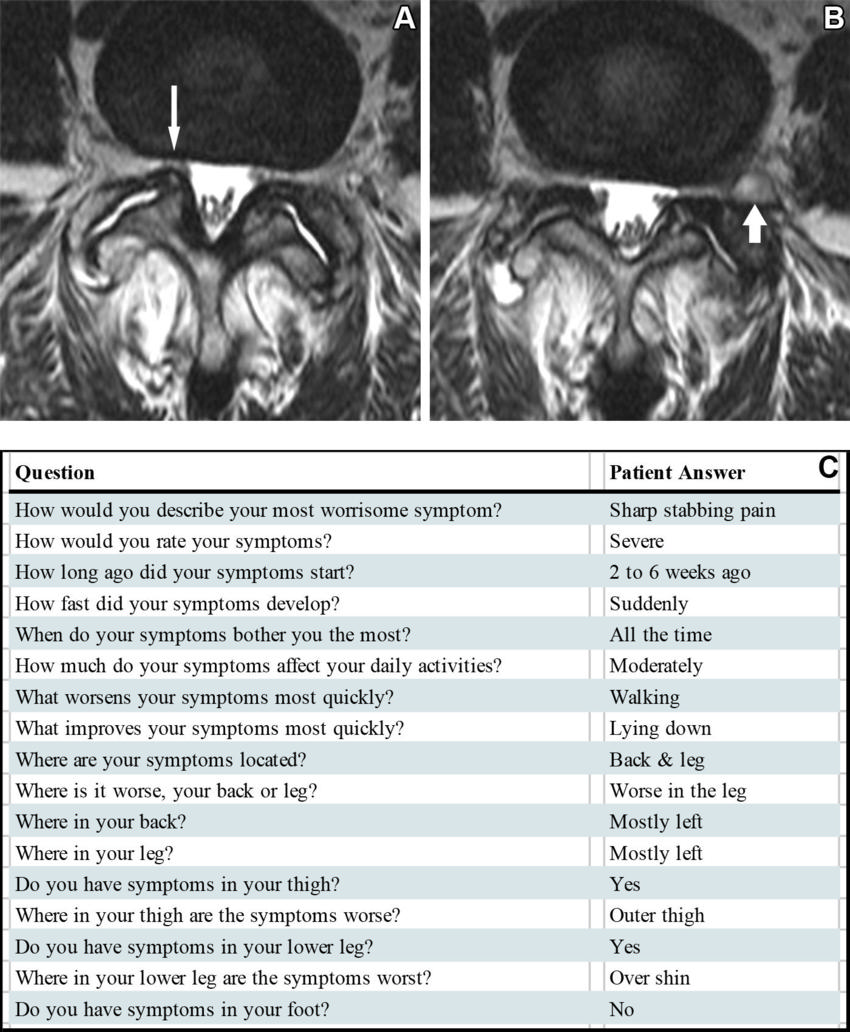
Figure 5. (A, B) Axial T2-weighted fast spin-echo MRI scans in a 53-year-old female participant with lumbar spine symptoms. (A) On MRI scan without knowledge of symptom questionnaire results (SQR), the pain generator was misdiagnosed as facet arthropathy at L4–5 level bilaterally. MRI showed multiple other possible pain generators, including subarticular zone stenosis (arrow). (B) On MRI scan with SQR, the pain generator was diagnosed as foraminal stenosis at L4-5 level on the left, agreeing with diagnosis made by spine specialist. Facet cyst (arrow) compresses left L4 dorsal root ganglion. (C) Pre-MRI symptom questionnaire indicates the character and location of left-sided back and leg pain.
High-res (TIF) version
(Right-click and Save As)