Ten-Year Study Shows Tomosynthesis Improves Breast Cancer Detection
Released: September 17, 2024
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — According to a new 10-year study, screening for breast cancer with digital breast tomosynthesis (DBT) increases cancer detection rates and significantly reduces the rate of advanced cancers compared to conventional 2D digital mammography. The findings were published today in Radiology, a journal of the Radiological Society of North America (RSNA).
Mammography is considered the gold standard in breast cancer screening for the general population. However, conventional 2D mammography, in which a low-dose X-ray system produces pictures of the inside of the breast from two angles, fails to detect approximately 20% of breast cancers. It is also associated with false-positive results, where an abnormality seen on a screening mammogram turns out not to be cancer after a woman has been recalled for and undergone additional tests.
DBT is an advanced form of mammography that reconstructs pictures of the breast taken from different angles into 3D images. Studies have found that DBT has a higher cancer detection rate compared to digital mammography.
"This study is the first to compare 10 years of data on breast cancers detected by DBT to digital mammography-detected cancers," said co-author Jaskirandeep Kaur Grewal, PA-C., previous student at Yale School of Medicine Physician Associate Program.
In the retrospective study, Dr. Philpotts and a team of researchers analyzed consecutive cancer cases detected by screening mammography over 13 years at Yale University/Yale-New Haven Health. The data included 10 years of mammograms performed with DBT, which became the standard at Yale facilities beginning in 2011, and the preceding three years of mammograms performed with digital mammography.
The study cohort included 272,938 screening mammograms, of which 35,544 were performed with digital mammography, and 237,394 were performed with DBT. A total of 1,407 cancers were detected, 142 by mammography and 1,265 by DBT.
"Overdiagnosis has been a hot topic in mammography screening. Skeptics of mammography screening believe that the use of DBT results in overdiagnosis," said first co-author Liane Elizabeth Philpotts, M.D., professor of radiology and biomedical imaging at Yale School of Medicine in New Haven, Connecticut.
Overdiagnosis means the cancers found are not clinically relevant and may not cause a health concern for the patient if left undetected.
According to Dr. Philpotts, digital mammography and DBT detected various subtypes and grades of tumors at similar rates. The ratio of invasive cancers to ductal carcinoma in situ (DCIS) did not differ significantly between the two modalities.
"We found that digital mammography and DBT screening mammography found the same types of cancers, but at different stages," she said. "DBT found more aggressive cancers at an earlier stage compared to digital mammography."
DBT had a higher cancer detection rate than mammography (5.3% versus 4.0%) and a lower rate of advanced cancers (32.7% versus 43.6%), indicating that cancers are likely being detected earlier. Cancer detection was improved when women had repeat mammograms with DBT.
Most true-positive cancer cases detected by DBT presented as masses, while fewer presented as calcifications and asymmetries.
The recall rate for DBT (7.2%) was significantly lower than for digital mammography (10.6%).
"DBT's lower recall rate, higher cancer detection rate and lower rate of advanced cancers is a win, win, win," Dr. Philpotts said. "I think this data will contribute to the debate of overdiagnosis by demonstrating that DBT is not over-diagnosing cancers. It's finding the bad actors earlier."
Dr. Philpotts said additional studies using long-term data are needed to better understand the role of DBT in screening outcomes.
"These findings add to the growing literature regarding cancer detection with DBT and support its use in screening mammography in the United States and globally," Dr. Philpotts said. "Our results may provide healthcare institutions that have not yet switched from digital mammography to DBT with the data they need to adopt the newer technology."
"Breast Cancers Detected during a Decade of Screening with Digital Breast Tomosynthesis: Comparison with Digital Mammography." Collaborating with Dr. Philpotts and Grewal were Laura Jean Horvath, M.D., Michelle Young Giwerc, PA-C, Lawrence Staib, Ph.D., and Maryam Etesam, M.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast tomosynthesis, visit RadiologyInfo.org.
Video (MP4):

Video 1. Jaskirandeep Kaur Grewal, PA-C., discusses her research which shows that screening for breast cancer with digital breast tomosynthesis increases cancer detection rates and significantly reduces the rate of advanced cancers compared to conventional 2D digital mammography.
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
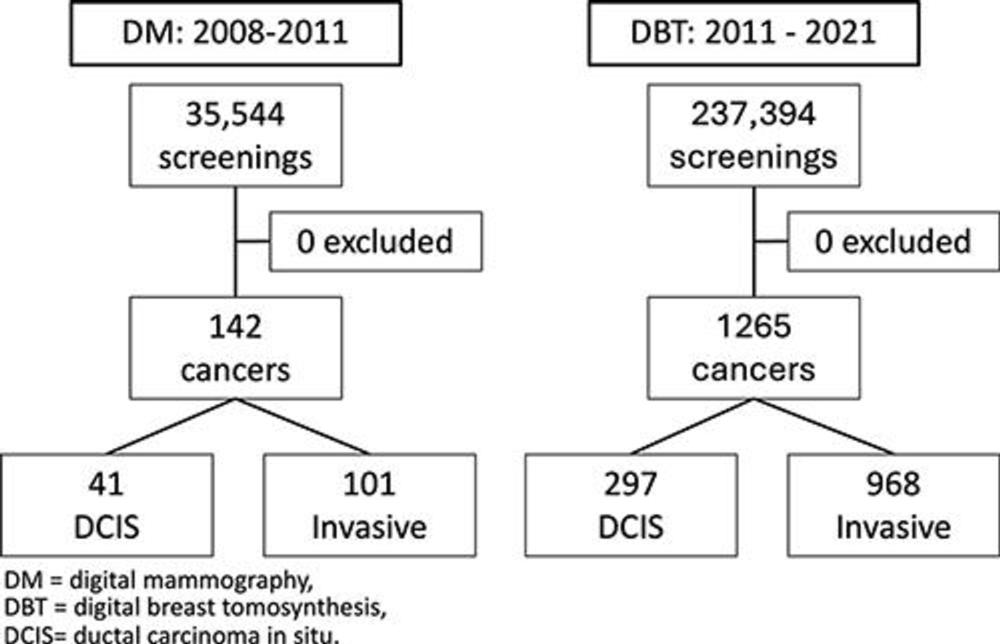
Figure 1. Flow charts for digital mammography and digital breast tomosynthesis cohorts.
High-res (TIF) version
(Right-click and Save As)
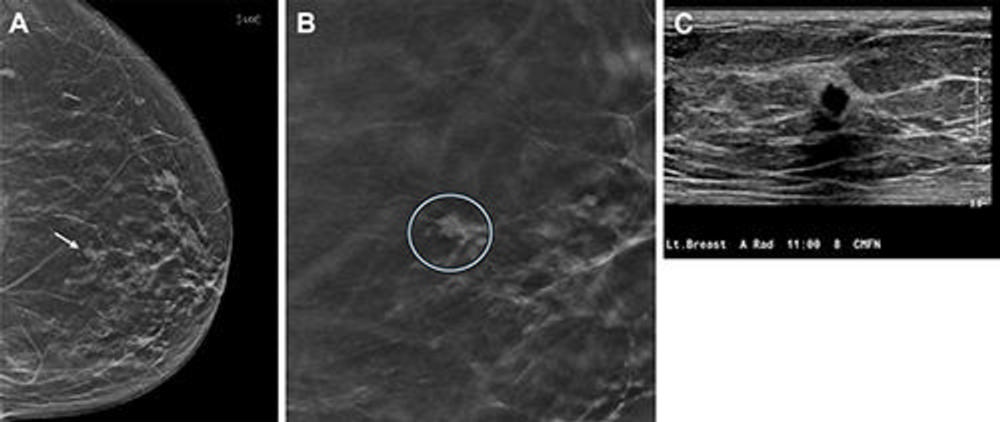
Figure 2. Images in a 67-year-old female patient who was recalled from screening for a small focal asymmetry in the left breast. (A) Two-dimensional mammographic image shows the lesion (arrow), which is difficult to see. (B) Digital breast tomosynthesis section image shows spiculated margins (circle). (C) US image shows a corresponding irregular hypoechoic mass with angular margins. Pathologic evaluation revealed a 0.7-cm triple-negative invasive carcinoma.
High-res (TIF) version
(Right-click and Save As)
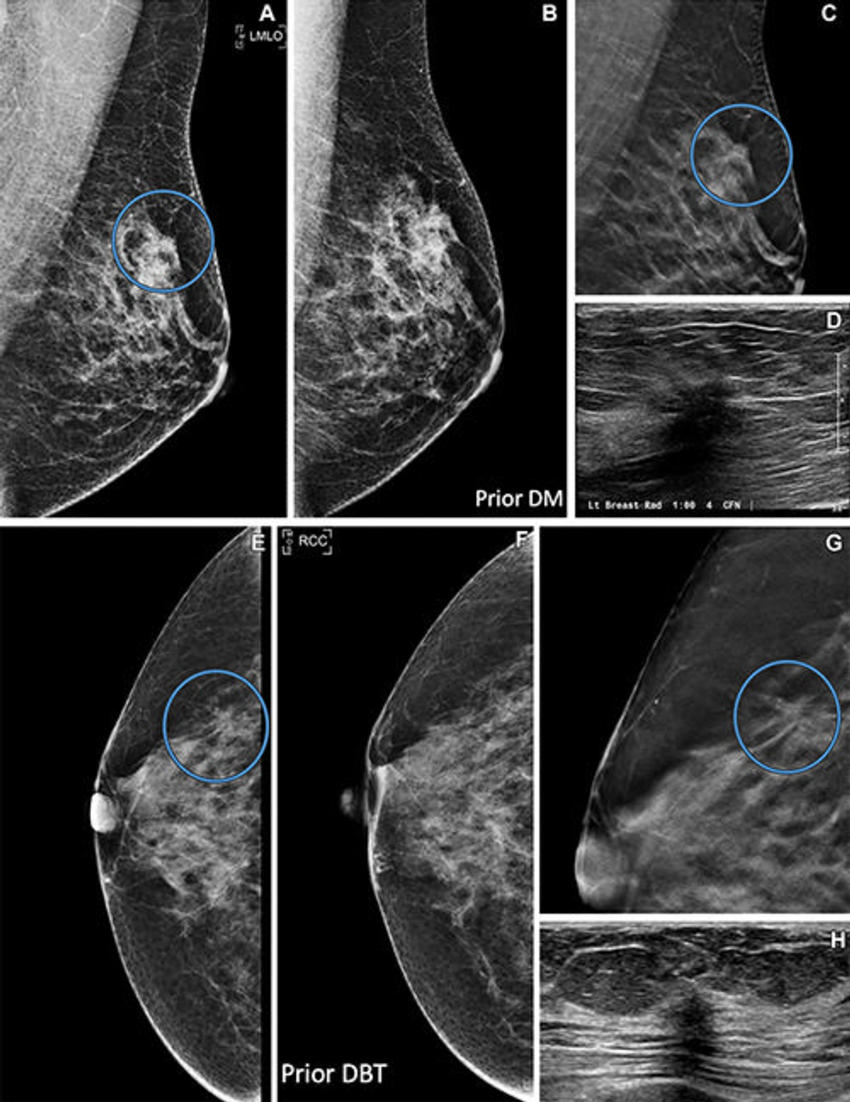
Figure 3. Images in (A–D) a 48-year-old female patient and (E–H) a 65-year-old female patient. (A) Left mediolateral oblique (LMLO) prevalent digital breast tomosynthesis (DBT) screening image shows an irregular mass (circle). (B) Prior screening digital mammogram (DM) suggests the mass may have been present but was not depicted. (C) DBT section image shows spiculated margins (circle). (D) US image shows a corresponding irregular hypoechoic mass. A 2.4-cm estrogen receptor– and progesterone receptor–positive, human epidermal growth factor receptor–negative invasive ductal carcinoma was found at pathologic evaluation. (E) Incident DBT screening image shows a new mass in the right breast (circle). (F) Previous DBT scan shows no finding. (G) DBT section image shows spiculated margins (circle). (H) US image shows a small irregular hypoechoic mass. A 0.6-cm estrogen receptor– and progesterone receptor–positive, human epidermal growth factor receptor–negative invasive ductal carcinoma was found at pathologic evaluation. RCC = right craniocaudal.
High-res (TIF) version
(Right-click and Save As)

