Expert Panel Endorses New Ultrasound Terminology for Early Pregnancy
Released: August 27, 2024
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. (Aug. 27, 2024) — For the first time, a multi-medical society panel has developed and endorsed a uniform lexicon for describing the observations seen on ultrasound during the first trimester of pregnancy. The lexicon, based on scientific evidence, societal guidelines and expert consensus, was published today in Radiology, a journal of the Radiological Society of North America (RSNA) and simultaneously in the American Journal of Obstetrics & Gynecology. The lexicon addresses terms frequently used in first trimester ultrasound reports, such as ‘ectopic pregnancy,’ ‘heartbeat,’ ‘living’ and ‘viable.’
“While there is a multi-society agreement for first-trimester imaging guidelines for reliable sonographic findings to predict which pregnancies will not progress, there has been a lack of consensus on the terms used in the imaging report and in communicating with patients,” said first author Shuchi K. Rodgers, M.D., professor of radiology at the Sidney Kimmel Medical School of Thomas Jefferson University in Philadelphia, Pennsylvania. “Many terms currently used are outdated or confusing, are used inconsistently, or may be interpreted differently by radiologists, clinicians and patients.”
The panel was convened by the Society of Radiologists in Ultrasound (SRU). Other societies participating in the development of the lexicon included the Society of Abdominal Radiology, the American College of Radiology, the American College of Obstetricians and Gynecologists, the American Institute of Ultrasound in Medicine, the Society for Maternal-Fetal Medicine, the American Society of Reproductive Medicine, the Society of Family Planning and the American College of Emergency Physicians.
Under the leadership team of Dr. Rodgers, senior author Lori M. Strachowski, M.D., and Mindy M. Horrow, M.D., (SRU past-president), the expert panel worked for a year and a half to reach a consensus on the uniform language. Panelists agreed unanimously or reached at least 80% agreement on preferred terms and synonyms, as well as terms to avoid, for the first-trimester ultrasound report.
Given that cardiac development is gradual and incomplete during the first trimester of pregnancy, the panel recommended the use of the term ‘cardiac activity’ instead of ‘heart motion’ or ‘heartbeat.’ The panel also recommended against terms, such as ‘live,’ ‘living,’ and ‘viable,’ that could raise unrealistic expectations for patients facing a potential pregnancy loss or an ectopic pregnancy.
“We recognize that specific language in the medical record could be used by third parties to negatively affect the physician-patient relationship,” said Dr. Strachowski, clinical professor of radiology and biomedical imaging and obstetrics, gynecology and reproductive sciences from the University of California, San Francisco. “Our goal was to recommend clear, specific, scientifically based and medically appropriate terminology that communicates clearly across disciplines, minimizes bias and harm, and respects patient preferences.”
While the terms ‘miscarriage’ and ‘spontaneous abortion’ remain part of the agreed lexicon, the historically used ‘pregnancy failure’ has been replaced with ‘early pregnancy loss.’
“Because patients have rapid access to their medical records, we considered patient preferences for and against certain terminology,” Dr. Strachowski said. “The term ‘pregnancy failure’ was never meant to convey blame or guilt, but it didn’t sit well with patients.”
According to the recommendations, an intrauterine pregnancy is defined as a pregnancy implanted in a normal location, while an embryo implanted in any abnormal location, whether inside (such as within a cesarean scar) or outside the uterus, is an ectopic pregnancy.
“We make it very clear that all ectopic pregnancies carry an increased risk of maternal morbidity and mortality,” she said.
Dr. Strachowski said all the participating societies have fully endorsed the new first-trimester ultrasound lexicon, and the panel expects it will be widely adopted.
“A Lexicon for First-Trimester US: Society of Radiologists in Ultrasound Consensus Conference Recommendations.” Collaborating with Drs. Rodgers, Strachowski and Horrow were Peter M. Doubilet, M.D., Ph.D., Mary C. Frates, M.D., Anne Kennedy, M.B., B.Ch., Rochelle Andreotti, M.D., Kristyn Brandi, M.D., M.P.H., Laura Detti, M.D., Sarah K. Horvath, M.D., M.S.H.P, Aya Kamaya, M.D., Atsuko Koyama, M.D., M.P.H., Penelope Chun Lema, M.D., Katherine E. Maturen, M.D., M.S., Tara Morgan, M.D., Sarah G. Običan, M.D., Kristen Olinger, M.D., Roya Sohaey, M.D., and Suneeta Senapati, M.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on ultrasound, visit RadiologyInfo.org.
Images (JPG, TIF):
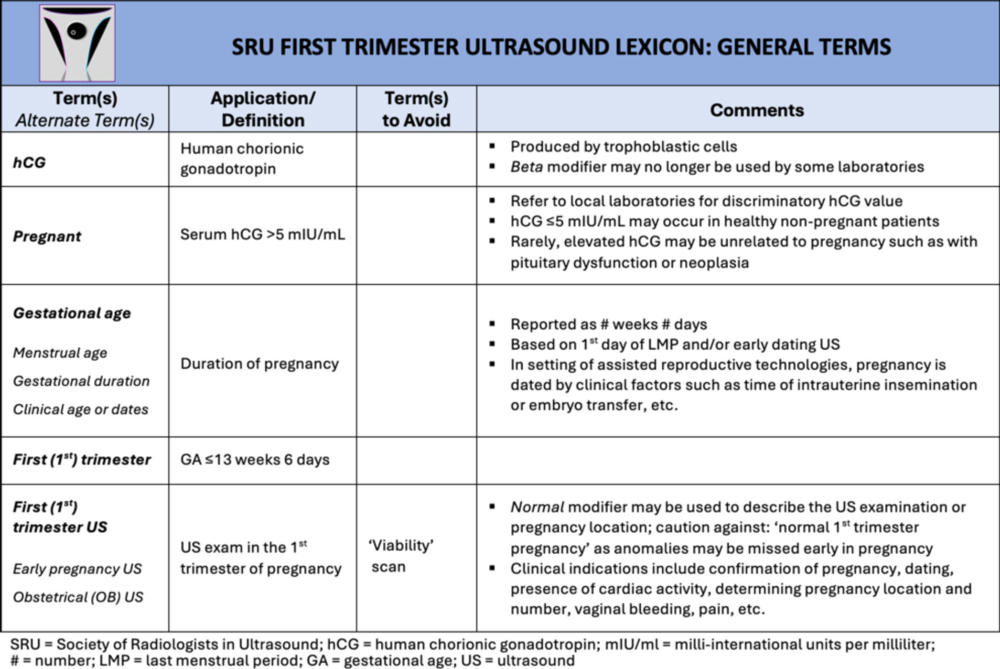
Figure 1. General terms. Lexicon terms (bolded and/or italicized) applicable to pregnancy but not specific to imaging are listed in this table.
High-res (TIF) version
(Right-click and Save As)
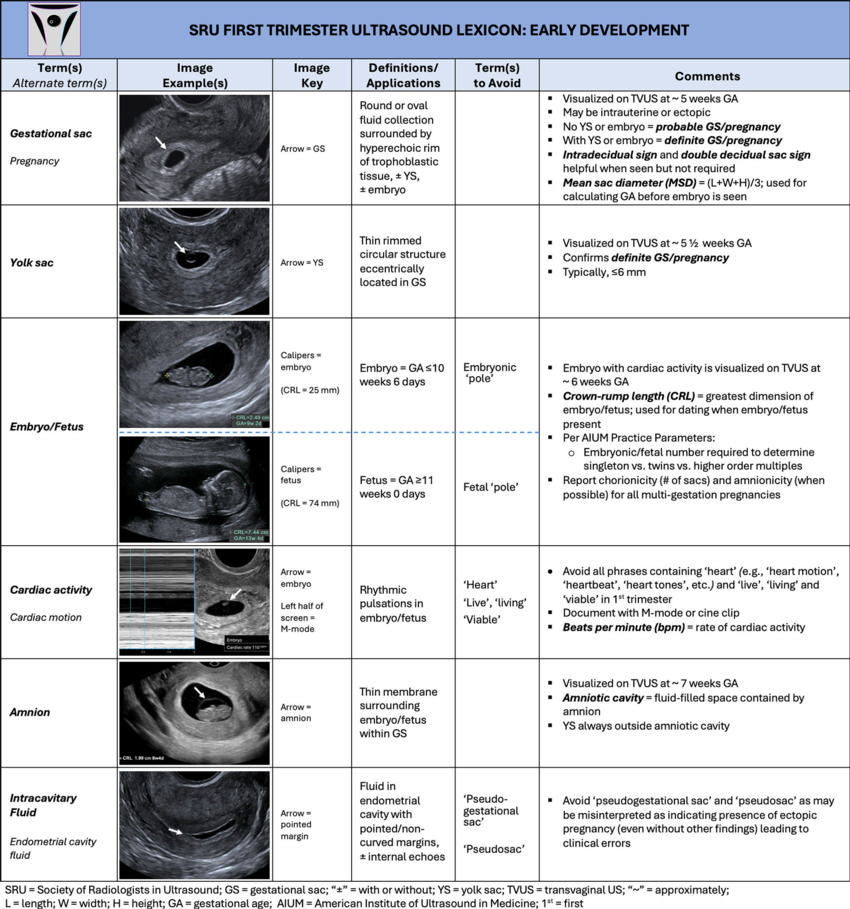
Figure 2. Early development. Lexicon terms (bolded and/or italicized) in this table relate to structures visualized at US in early pregnancy development. Terms to avoid are in single quotation marks. Terms specific to multigestation pregnancies, such as chorionicity and amnionicity, are beyond the scope of this lexicon.
High-res (TIF) version
(Right-click and Save As)
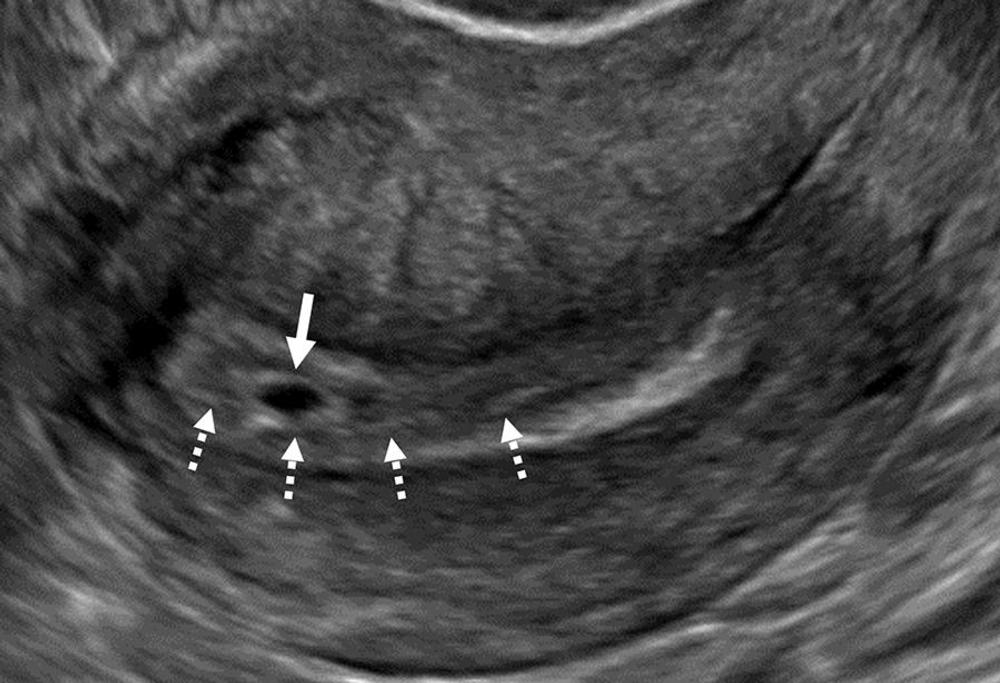
Figure 3. Intradecidual sign. Transvaginal sagittal grayscale US image in a 34-year-old pregnant patient shows a 4-mm empty gestational sac (GS) (solid arrow) in the anterior endometrium. The location of the GS to one side of the central hyperechoic line (dotted arrows) representing the opposed innermost layers of decidualized endometrium confirms it is within endometrium and not the endometrial cavity, hence the name intradecidual sign. This sign is helpful when seen to diagnose a probable intrauterine pregnancy (IUP) before visualization of the yolk sac. Three days later, the yolk sac was visualized (not shown), allowing for the diagnosis of a definite IUP.
High-res (TIF) version
(Right-click and Save As)
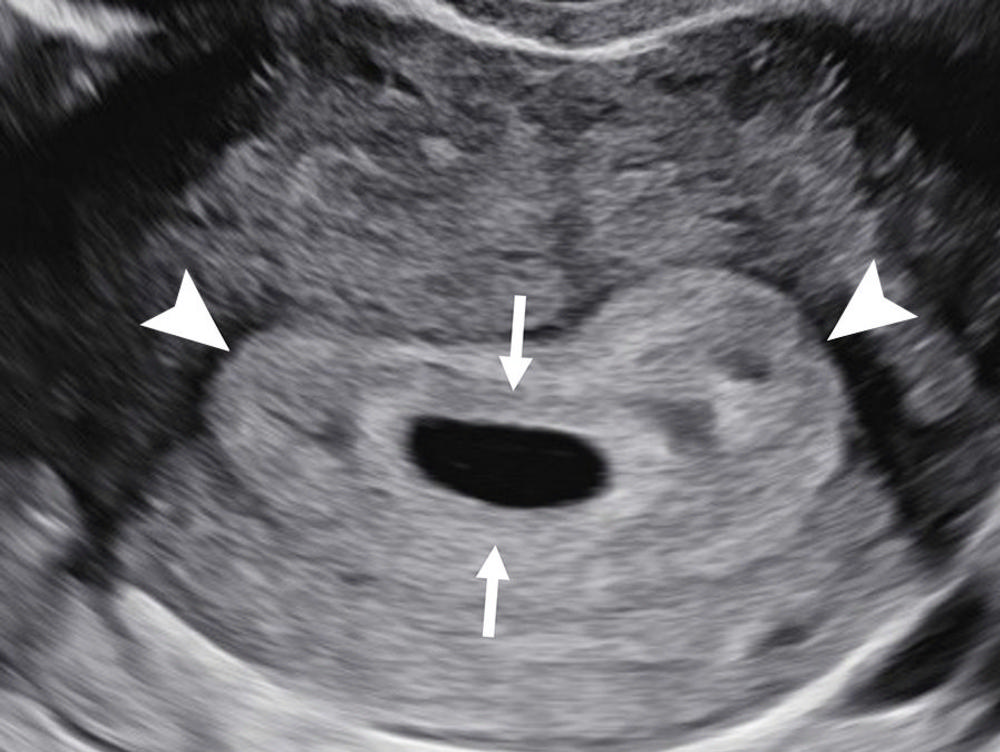
Figure 4. Double decidual sac sign. Transvaginal transverse grayscale US image in a 27-year-old pregnant patient at 5 weeks 3 days shows two concentric echogenic rings around an oval fluid collection representing the double decidual sac sign. The inner echogenic ring (arrows) corresponds to trophoblastic chorion and decidua capsularis. The outer echogenic ring (arrowheads) represents decidua vera and endometrial lining. The double decidual sac sign is more specific for an intrauterine pregnancy than the intradecidual sign when the gestational sac is empty.
High-res (TIF) version
(Right-click and Save As)
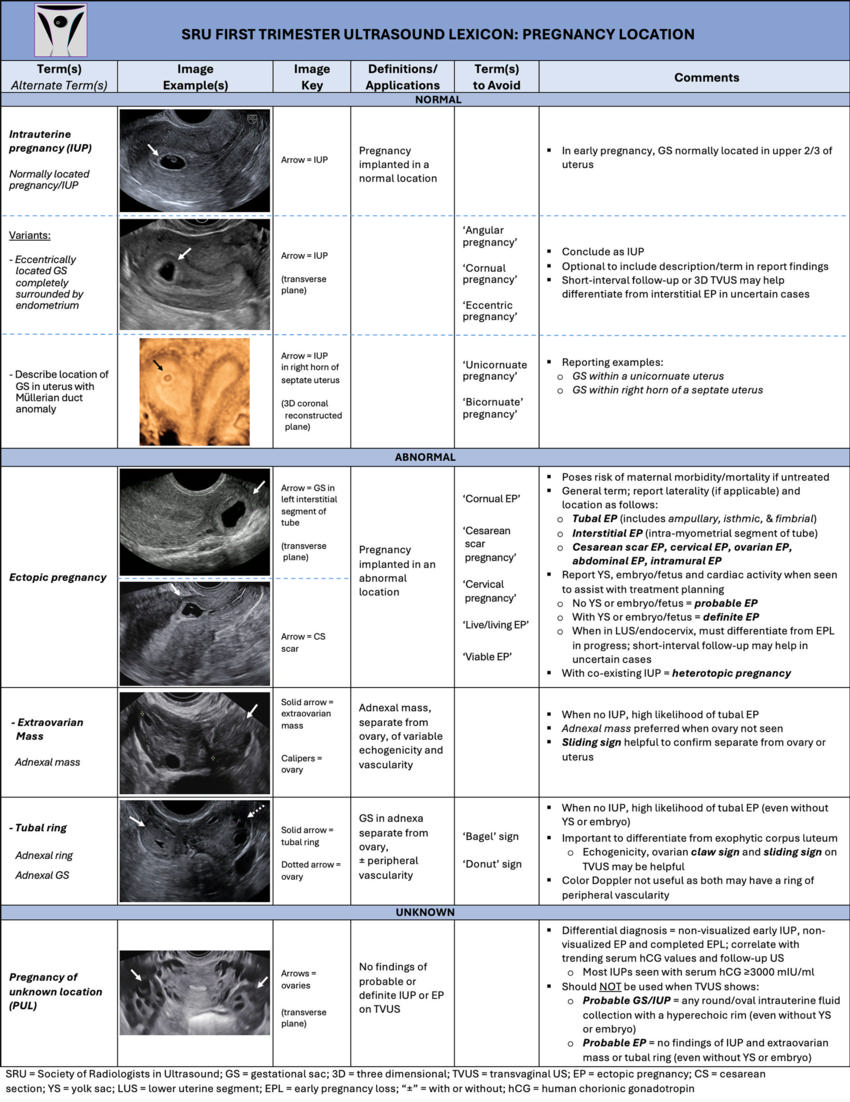
Figure 5. Pregnancy location. The location of a pregnancy is divided into normal, abnormal, and unknown. Lexicon terms are bolded and/or italicized, and terms to avoid are in single quotation marks. The essential word in the definition of intrauterine pregnancy and ectopic pregnancy (EP) is implanted, which helps differentiate pregnancies that are temporarily located in the lower uterine segment. This definition also further clarifies abnormal intrauterine implantation sites as EPs.
High-res (TIF) version
(Right-click and Save As)
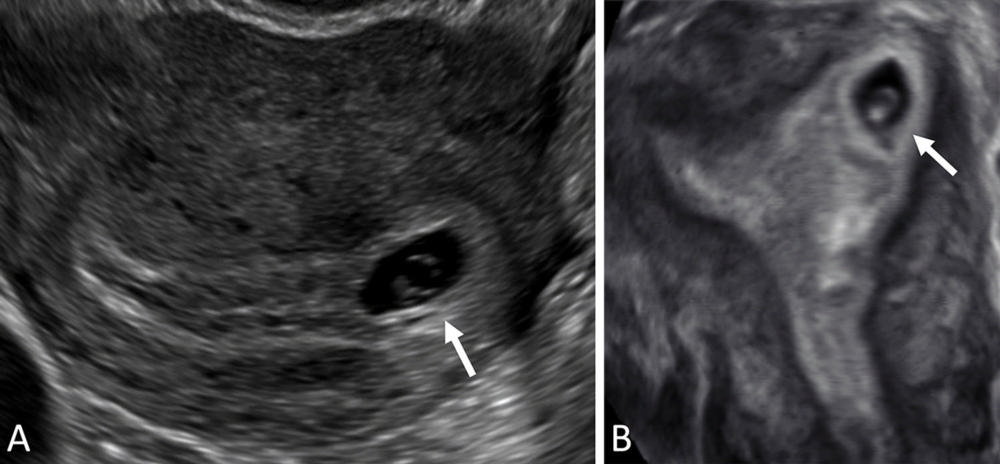
Figure 6. Normal intrauterine pregnancy (IUP) variant: eccentrically located gestational sac (GS) completely surrounded by endometrium. (A) Transvaginal transverse grayscale and (B) coronal reformatted three-dimensional US image in a 36-year-old pregnant patient shows an off-midline (leftward) GS (arrow) at 5 weeks 4 days with yolk sac and embryo. The GS is completely surrounded by endometrium and may be reported as an IUP without further description. If desired, the user may describe as an eccentrically located GS completely surrounded by endometrium but should conclude as an IUP to obviate concern for an interstitial ectopic pregnancy. The terms ‘angular’ or ‘cornual pregnancy’ should be avoided. Coronal reformatted three-dimensional US may help confirm a GS is located within endometrium, as demonstrated in this case.
High-res (TIF) version
(Right-click and Save As)
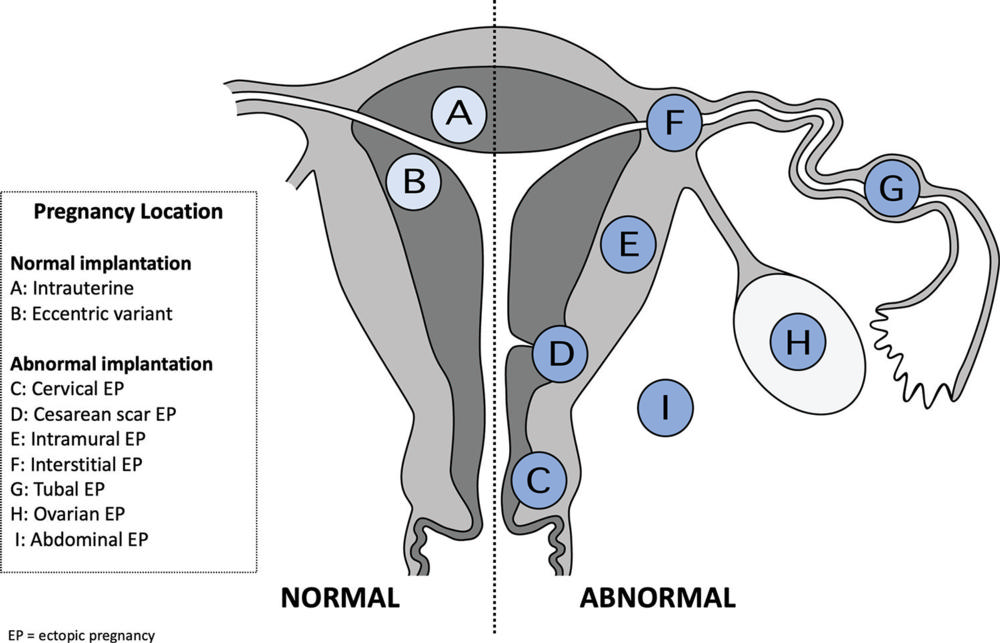
Figure 7. Specific normal and abnormal pregnancy location sites. Schematic illustration of normal pregnancy implantation sites on the left half of the uterine diagram and abnormal implantation sites on the right. Representative round icons indicate the implantation site with corresponding letters to lexicon terms in the box. Of note, it is optional to further describe a tubal ectopic pregnancy location as isthmic, infundibular, or ampullary when the precise location is clear at US.
High-res (TIF) version
(Right-click and Save As)
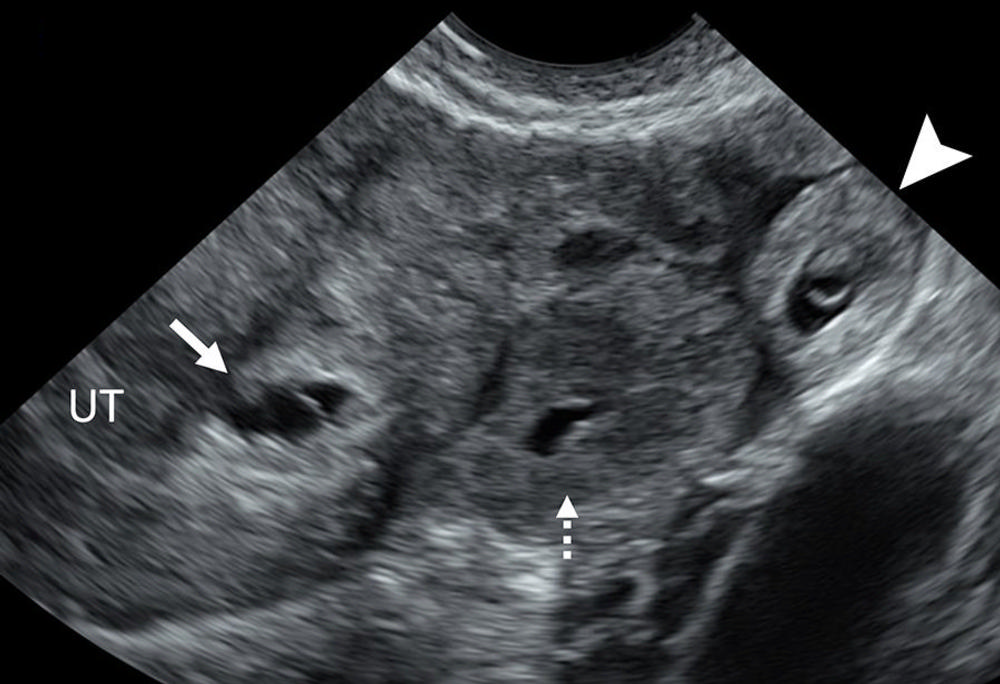
Figure 8. Heterotopic pregnancy. Transvaginal transverse grayscale US image in a 27-year-old pregnant patient shows an early intrauterine pregnancy (IUP) (solid arrow) containing a yolk sac and a tubal ring of ectopic pregnancy (EP) (arrowhead) also containing a yolk sac. The coexistence of an IUP and EP is termed heterotopic pregnancy. The left ovary contains a corpus luteum (dotted arrow) and is seen in the center. The rim of chorionic tissue in the IUP and EP is hyperechoic, whereas in contrast, the corpus luteum is hypoechoic. Echogenicity can help distinguish a tubal ring from a corpus luteum in some cases. UT = uterus.
High-res (TIF) version
(Right-click and Save As)
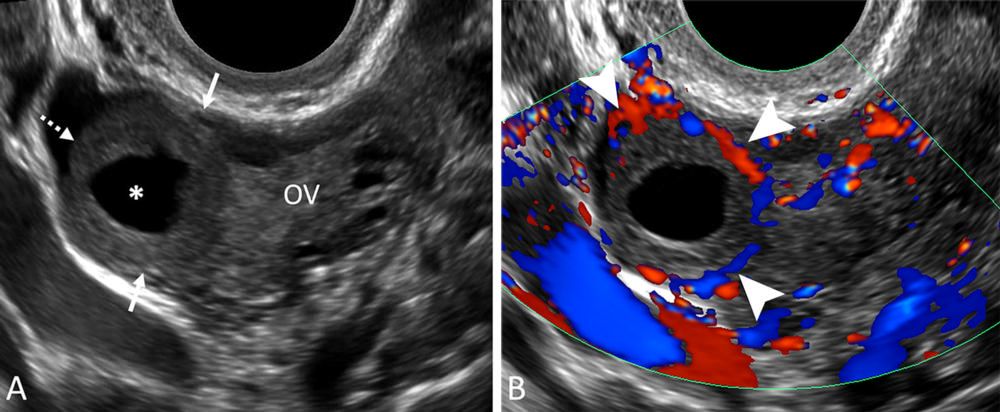
Figure 9. Corpus luteum. (A) Transvaginal sagittal grayscale and (B) color Doppler US image in a 31-year-old pregnant patient shows a round, hypoechoic, thick-walled structure (dotted arrow) with a central cystic space (*) and peripheral vascularity (arrowheads), characteristic of a corpus luteum. This corpus luteum arises in an exophytic fashion from the right ovary (OV), which can mimic a tubal ring of ectopic pregnancy. A helpful feature to diagnose a corpus luteum is a claw sign (solid arrows) of partially surrounding ovarian parenchyma, which confirms an ovarian origin.
High-res (TIF) version
(Right-click and Save As)
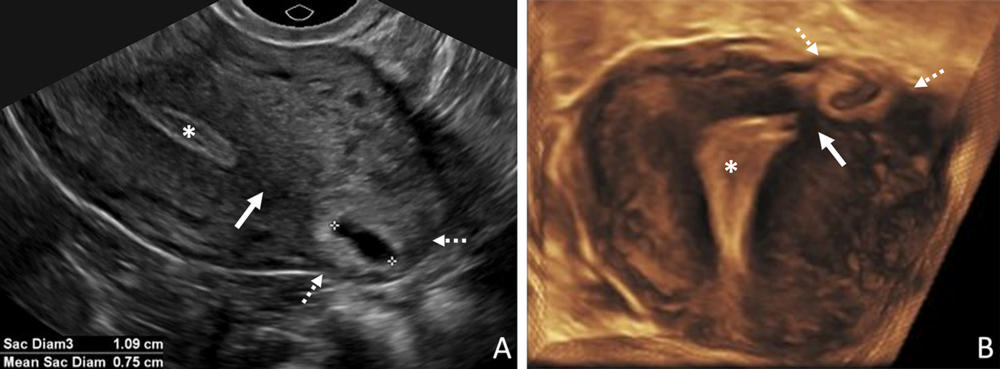
Figure 10. Interstitial ectopic pregnancy (EP). (A) Transvaginal transverse grayscale and (B) coronal reformatted three-dimensional US image in a 29-year-old pregnant patient shows a gestational sac (GS) (calipers) at 5 weeks 3 days. There is intervening myometrium (solid arrow) between the GS and endometrium (*). A claw sign (dotted arrows) of myometrial tissue confirms the pregnancy is implanted in the interstitial (intramyometrial) segment of the tube, termed an interstitial EP. The term ‘cornual EP’ should be avoided. Coronal reformatted three-dimensional US may better demonstrate an interstitial EP separate from the endometrium, as in this case. Diam = diameter.
High-res (TIF) version
(Right-click and Save As)
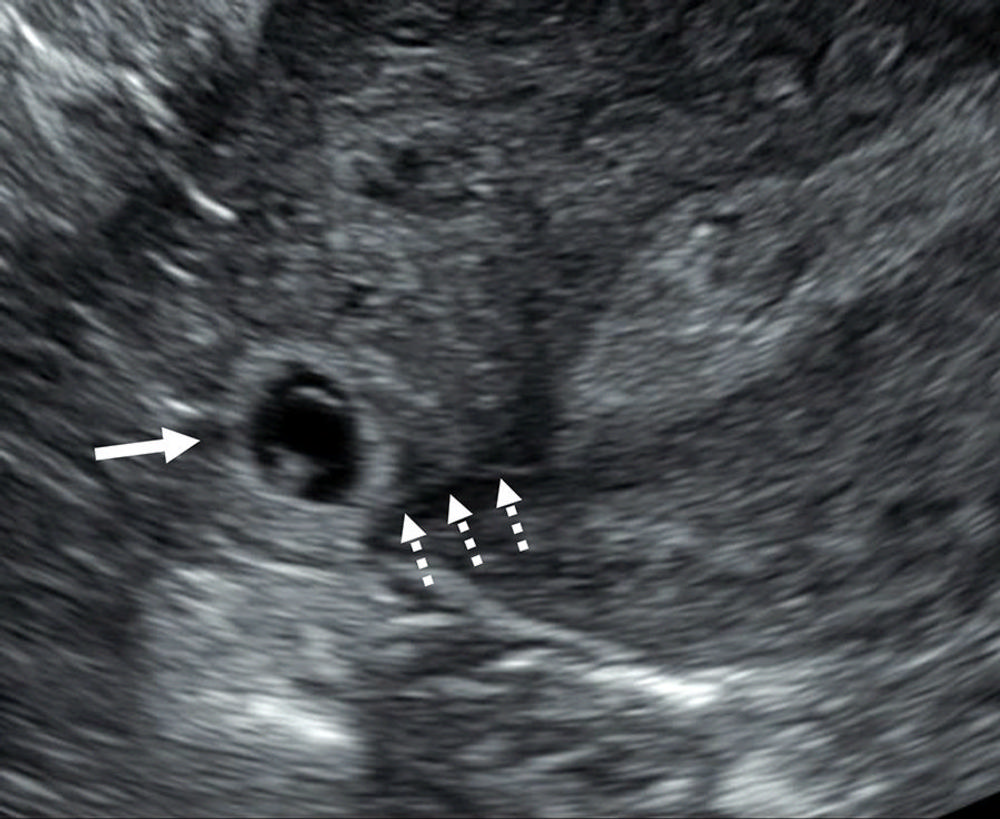
Figure 11. Interstitial line sign. Transvaginal transverse grayscale US image in a 33-year-old pregnant patient shows a right interstitial ectopic pregnancy (EP) (solid arrow) at 6 weeks 0 days. In addition to the characteristic sonographic findings of an interstitial EP shown in Figure 10, there is a thin echogenic line (dotted arrows) representing the interstitial segment of the tube. This line connects the endometrium to the ectopic gestational sac and is called the interstitial line sign.
High-res (TIF) version
(Right-click and Save As)
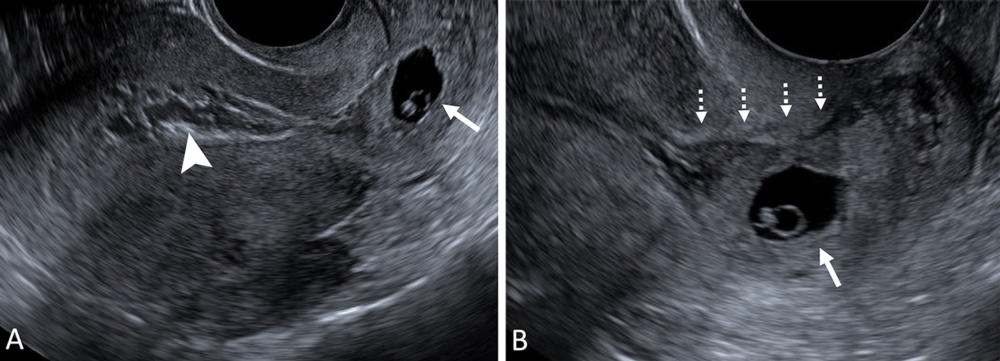
Figure 12. Cervical ectopic pregnancy (EP). (A) Transvaginal sagittal grayscale US of the uterus and (B) high-resolution US image of the cervix in a 31-year-old pregnant patient at 6 weeks 3 days with vaginal bleeding. A gestational sac (GS) (solid arrow) is seen containing an embryo with cardiac activity (not shown) implanted in the cervix. Mixed-echogenicity material (arrowhead) representing blood products expands the endometrial cavity. The location of the GS eccentric to the endocervical canal (dotted arrows) and cardiac activity help make the diagnosis of a cervical EP. The term ‘cervical pregnancy’ should be avoided.
High-res (TIF) version
(Right-click and Save As)

Figure 13. Ovarian ectopic pregnancy (EP). Transvaginal sagittal grayscale US image in a 35-year-old pregnant patient at 6 weeks 4 days shows a gestational sac (GS) (arrow) containing a yolk sac and embryo with cardiac activity (not shown) within the ovary (Ov) (calipers), diagnostic of an ovarian EP. A peripheral follicle is present in the ovary (arrowhead). To avoid misdiagnosing a corpus luteum for the rare ovarian EP, a yolk sac or embryo should be present in the intraovarian thick-walled cystic structure representing the GS. UT = uterus.
High-res (TIF) version
(Right-click and Save As)
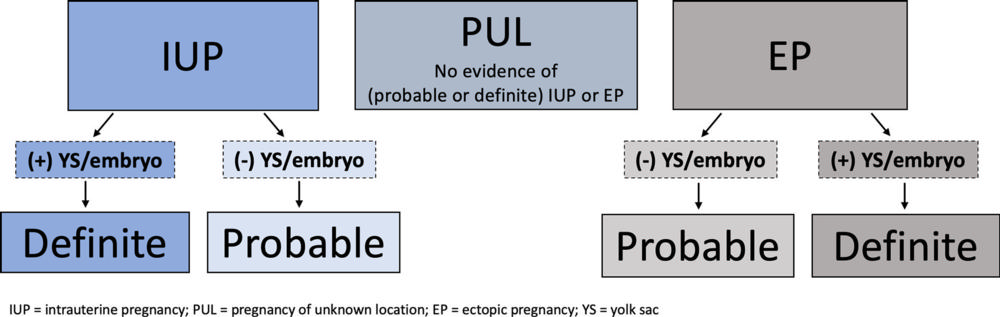
Figure 14. Pregnancy of unknown location (PUL). The original definition of PUL is maintained; however, it is clarified in the lexicon to clearly state that there should be no evidence of probable or definite intrauterine pregnancy (IUP) or ectopic pregnancy (EP) to qualify as a PUL. An empty gestational sac is considered a probable pregnancy whether implanted in a normal location (IUP) or abnormal location (EP) and should not be termed a PUL.
High-res (TIF) version
(Right-click and Save As)
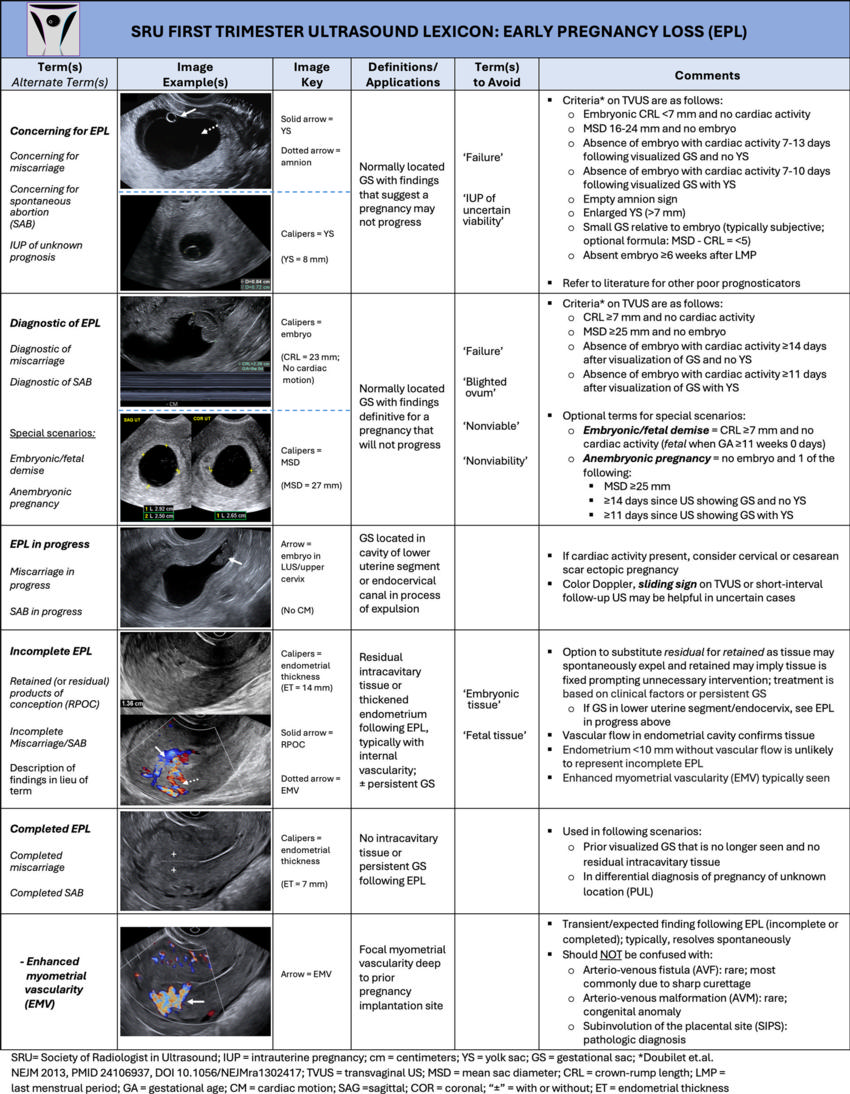
Figure 15. Early pregnancy loss (EPL). There are five main categories of EPL: concerning for, diagnostic of, in progress, incomplete, and completed. Enhanced myometrial vascularity (EMV) is included in the lexicon since increased myometrial vascularity deep to a prior implantation site is commonly confused with other rare entities, such as an arteriovenous fistula and arteriovenous malformation, which may lead to unnecessary work-up.
High-res (TIF) version
(Right-click and Save As)
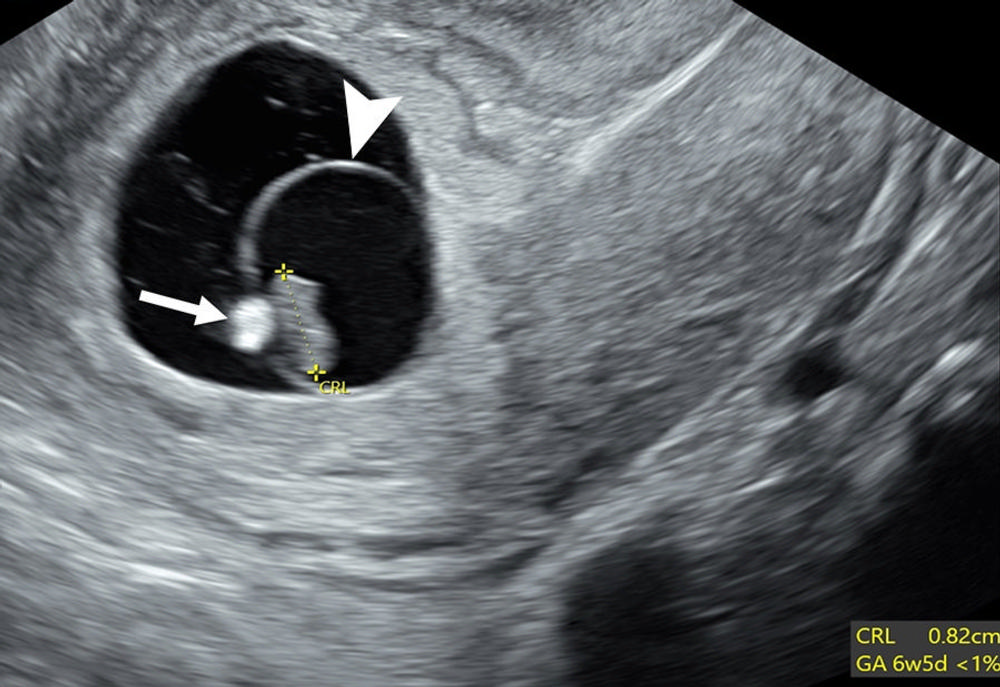
Figure 16. Poor prognosticators: calcified yolk sac and expanded amnion sign. Transvaginal sagittal grayscale US image in a 27-year-old pregnant patient shows an 8-mm embryo (calipers) without cardiac activity (M-mode not shown) sufficient for the interpretation of diagnostic of early pregnancy loss (EPL). Additional poor prognosticators include a calcified yolk sac (arrow) and an enlarged amniotic cavity (arrowhead) relative to the crown-rump length (CRL) of the embryo, called the expanded amnion sign. These additional observations, on their own, are only concerning for EPL. GA = gestational age.
High-res (TIF) version
(Right-click and Save As)
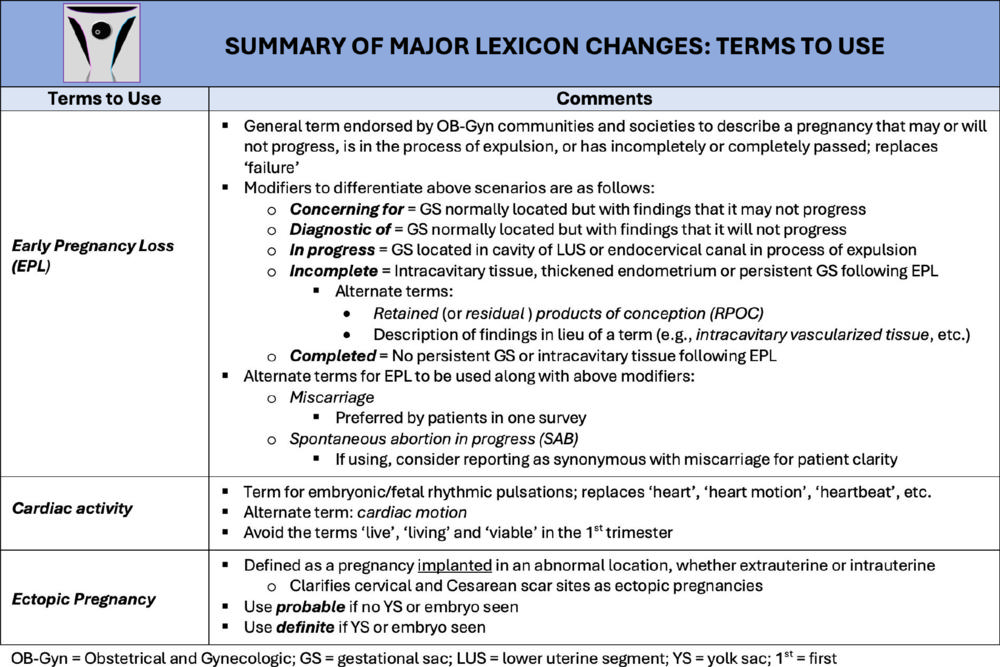
Figure 17. Summary of major lexicon changes highlighting terms to use. The major changes from currently used terminology to describe sonographic findings in the first trimester are (a) early pregnancy loss in lieu of ‘failure’; (b) cardiac activity in lieu of ‘heart motion’; and (c) defining ectopic pregnancy as an abnormal implantation site. The terms ‘live,’ ‘living,’ and ‘viable’ are commonly used terms to describe cardiac activity. However, as these terms may be misleading, they are best avoided in the first trimester.
High-res (TIF) version
(Right-click and Save As)
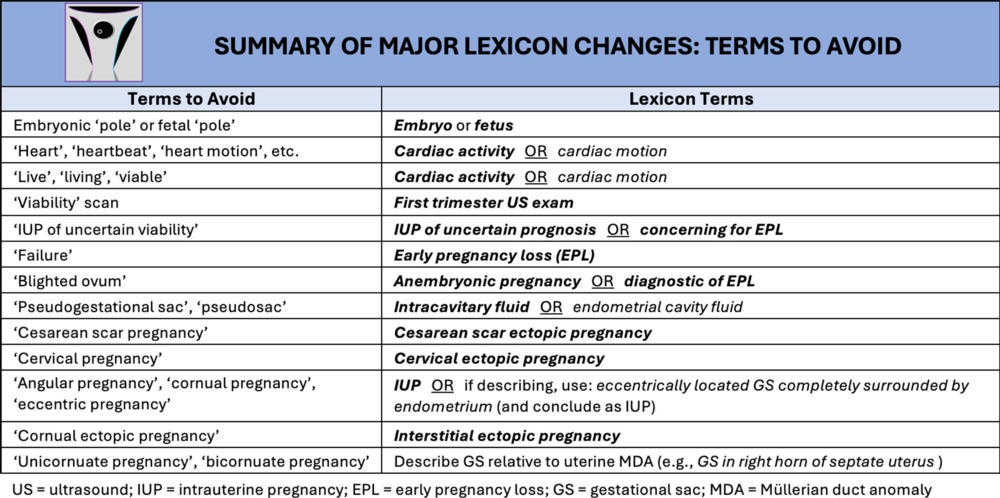
Figure 18. Summary of major lexicon changes highlights terms to avoid. Equally important as terms to use are those terms that are best avoided since they are obsolete or confusing (single quotation marks). This is accompanied by recommended lexicon terms (bold and italicized) to use instead.
High-res (TIF) version
(Right-click and Save As)

