Coronary Artery Calcium Score Predictive of Heart Attacks, Strokes
Released: March 05, 2024
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Coronary artery calcium scoring with CT can identify symptomatic patients with a very low risk of heart attacks or strokes, according to a new study published today in Radiology, a journal of the Radiological Society of North America (RSNA). Researchers said the findings may one day help some patients with stable chest pain avoid invasive coronary angiography.
Coronary artery calcium scoring with CT was developed to noninvasively measure the amount of calcium in the arteries of the heart. Higher scores are linked with atherosclerosis, a buildup of plaque in the arteries. A score of 1 to 399, for instance, suggests a moderate amount of plaque, while 400 or higher indicates a large plaque burden.
“Coronary artery calcium is a strong and independent predictor of cardiovascular events,” said study first author Federico Biavati, an M.D./Ph.D. candidate in the BIOQIC research training group and a radiology resident at Charité – Universitätsmedizin Berlin, Germany. “The presence of coronary artery calcification indicates that atherosclerosis may have been present for some time.”
The complete absence of coronary calcifications, on the other hand, is a good indicator of the absence of advanced atherosclerosis. However, the role of coronary artery calcium in patients with stable chest pain is less clear. Stable chest pain is a temporary but recurring condition triggered by stress, exercise or cold weather.
Under the direction of Marc Dewey, M.D., professor and vice chair of radiology at Charité, Biavati and colleagues assessed the prognostic value of coronary artery calcium scoring for major adverse cardiovascular events in 1,749 individuals, mean age 60. The participants were drawn from the DISCHARGE trial, a research project involving 26 centers in 16 European countries. Participants had stable chest pain and had been referred for invasive coronary angiography, a procedure in which a catheter is threaded to the heart under X-ray guidance. A contrast agent is then injected through the catheter to help doctors visualize the arteries of the heart.
The researchers stratified the patients into low-, intermediate- and high-risk categories based on their coronary artery calcium scores. They followed the participants for an average of 3.5 years and recorded any major adverse cardiovascular events.
People with a coronary artery calcium score of zero showed very low risk of major adverse cardiovascular events at follow-up. Only four of the 755 participants in the group, or 0.5%, had a major adverse cardiovascular event during the follow-up period. The group also had a low risk of only 4.1% for obstructive coronary artery disease.
“This finding may indicate that a zero coronary artery calcium score can play a larger role in patient management strategies,” Dr. Dewey said. “The findings suggest that patients with stable chest pain and a coronary artery calcium score of zero may not require invasive coronary angiography using cardiac catheterization because the risk of cardiovascular events is so low.”
There were 14 events in the 743 participants with a 1 to 399 coronary artery calcium score, for a risk of 1.9%. The 251 participants in the 400 and higher coronary artery calcium score group had 17 events for a significantly higher risk of 6.8%. The researchers found no evidence of a difference between sexes for major adverse cardiovascular events.
Despite the findings, the researchers said that further study is needed before coronary artery calcium scoring can be used to exclude patients from coronary CT angiography.
This is the second article published in Radiology from the DISCHARGE trial, the largest cardiac trial on chest pain. The first article, Effect of Body Mass Index on Effectiveness of CT versus Invasive Coronary Angiography in Stable Chest Pain: The DISCHARGE Trial, found that when patients suspected of having coronary artery disease were stratified by body mass index category, no differences in clinical outcomes were observed between those who underwent initial management with CT and those who underwent invasive coronary angiography.
“Coronary Artery Calcium Score Predicts Major Adverse Cardiovascular Events in Stable Chest Pain.” Collaborating with Dr. Dewey and Biavati were Luca Saba, M.D., Melinda Boussoussou, M.D., Klaus F. Kofoed, M.D., D.M.Sc., Theodora Benedek, M.D., Ph.D., Patrick Donnelly, M.D., José Rodríguez-Palomares, M.D., Ph.D., Andrejs Erglis, M.D., Cyril Štěchovský, M.D., Gintarė Šakalytė, M.D., Nada Čemerlić Ađić, M.D., Matthias Gutberlet, M.D., Ph.D., Jonathan D. Dodd, M.D., Ignacio Diez, M.D., Gershan Davis, M.D., Elke Zimmermann, M.D., Cezary Kępka, M.D., Radosav Vidakovic, MD., Ph.D., Marco Francone, M.D., Ph.D., Małgorzata Ilnicka-Suckiel, M.D., Ph.D., Fabian Plank, M.D., Ph.D., Juhani Knuuti, M.D., Rita Faria, M.D., Stephen Schröder, M.D., Colin Berry, Ph.D., Balazs Ruzsics, M.D., Ph.D., Nina Rieckmann, M.D., Christine Kubiak, Ph.D., Kristian Schultz Hansen, Ph.D., Jacqueline Müller-Nordhorn, M.D., M.P.H., Pál Maurovich-Horvat, M.D., Ph.D., M.P.H., Per E. Sigvardsen, M.D., Ph.D., Imre Benedek, M.D., Ph.D., Clare Orr, M.D., Filipa Xavier Valente, M.D., Ligita Zvaigzne, M.D., Vojtěch Suchánek, M.D., Antanas Jankauskas, M.D., Filip Ađić, M.D., Michael Woinke, M.D., Diarmaid Cadogan, M.D., Iñigo Lecumberri, M.D., Erica Thwaite, M.D., Mariusz Kruk, M.D., Aleksandar N. Neskovic, M.D., Massimo Mancone, M.D., Donata Kuśmierz, M.D., Gudrun Feuchtner, M.D., Mikko Pietilä, M.D., Ph.D., Vasco Gama Ribeiro, M.D., Tanja Drosch, M.D., Christian Delles, M.D., Riccardo Cau, M.D., Michael Fisher, M.D., Ph.D., Bela Merkely, M.D., Ph.D., Charlotte Kragelund, M.D., Ph.D., Rosca Aurelian, M.D., Stephanie Kelly, Bruno García del Blanco, M.D., Ph.D., Ainhoa Rubio, M.D., Bálint Szilveszter, M.D., Ph.D., Jens D. Hove, M.D., Ph.D., Ioana Rodean, M.D., Susan Regan, Hug Cuéllar Calabria, M.D., Ph.D., Ferenc István Édes, M.D., Linnea Larsen, M.D., Ph.D., Roxana Hodas, M.D., Adriane E. Napp, Ph.D., Robert Haase, M.D., Sarah Feger, M.D., Mahmoud Mohamed, M.Sc., Lina M. Serna-Higuita, M.D., Konrad Neumann, Ph.D., Henryk Dreger, M.D., Matthias Rief, M.D., Viktoria Wieske, M.D., Matthew J. Budoff, M.D., Melanie Estrella, Ph.D., Peter Martus, Ph.D., and Maria Bosserdt, Ph.D.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on cardiac CT for calcium scoring, visit RadiologyInfo.org.
Images (JPG, TIF):
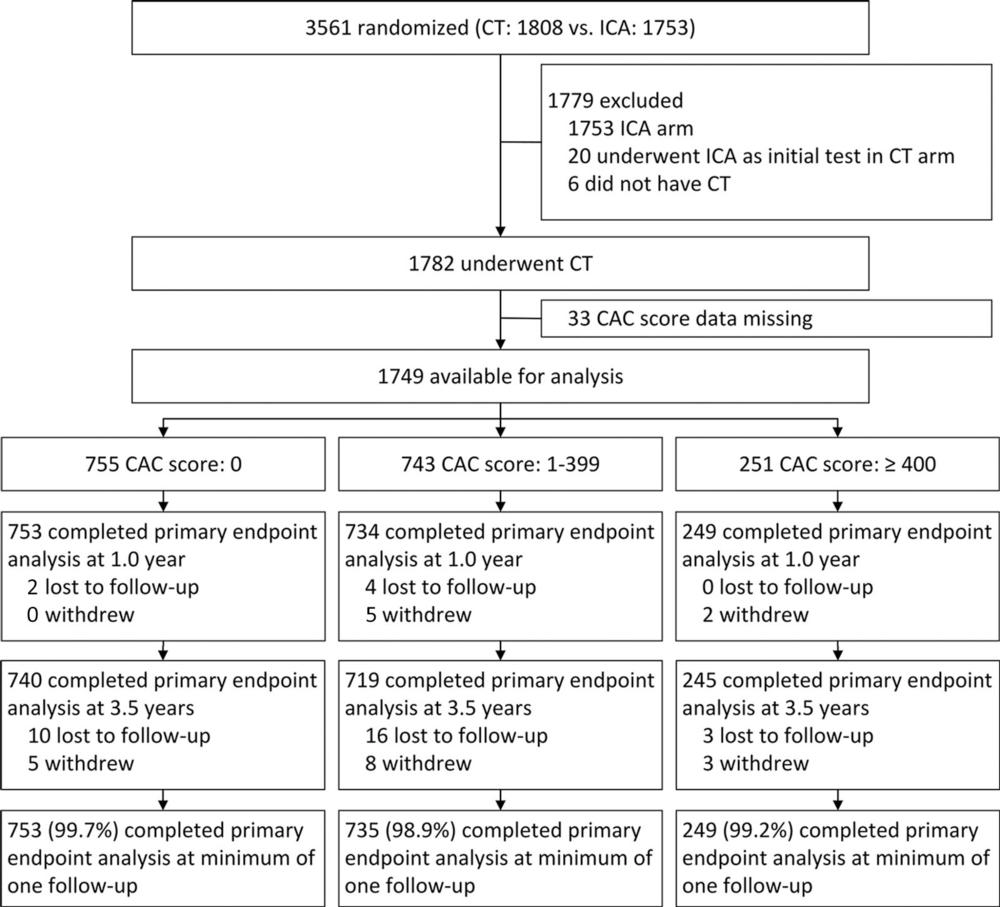
Figure 1. Flowchart of patient selection.
CAC = coronary artery calcium,
ICA = invasive coronary angiography
High-res (TIF) version
(Right-click and Save As)
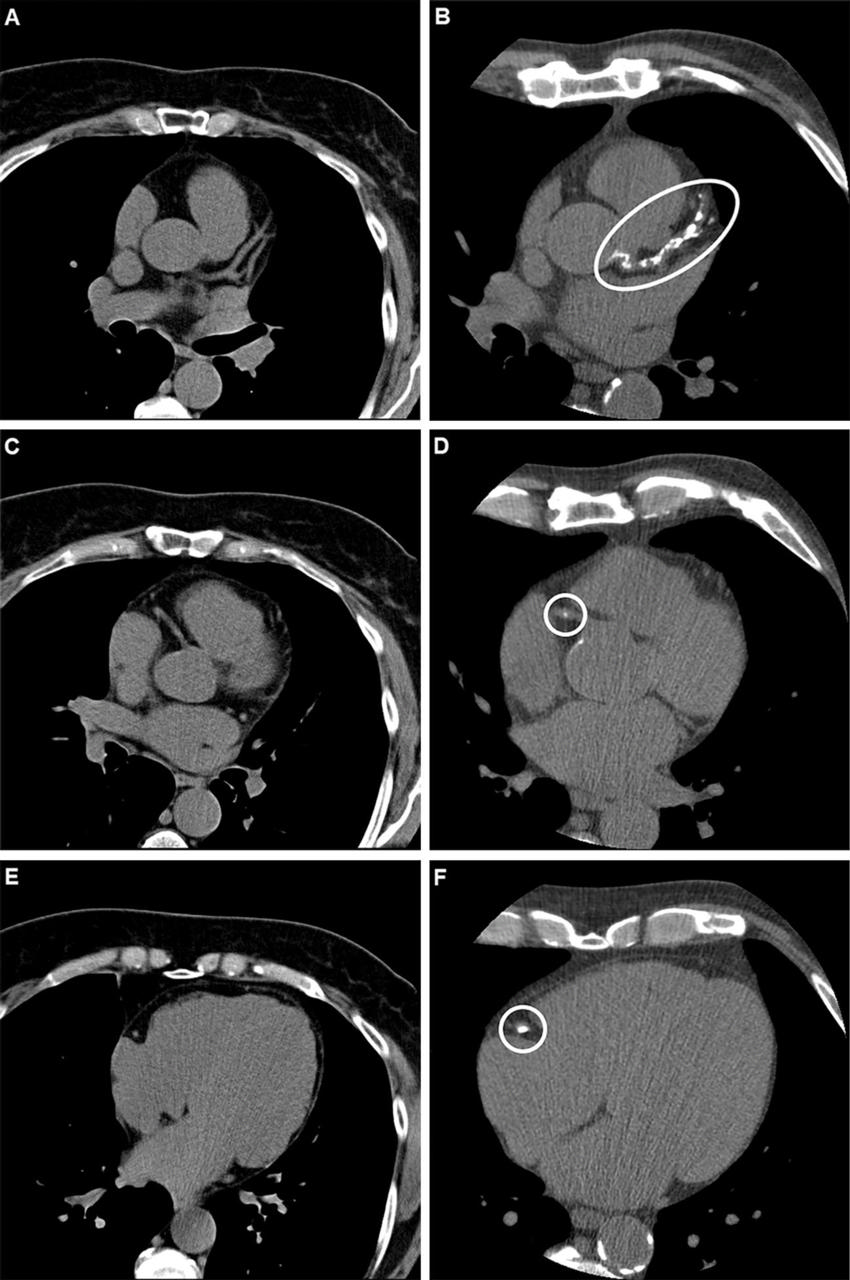
Figure 2. Example axial noncontrast CT scans in (A, C, E) a participant with a coronary artery calcium (CAC) score of 0, no signs of coronary artery disease at CT, and no major adverse cardiovascular events and (B, D, F) a participant who had a CAC score of 1013 (group with a CAC score of 400 or higher) and obstructive coronary artery disease at CT and required a revascularization procedure. With the scan on the left as reference, calcified plaques (ovals) can be seen on the right scan of the left main and left anterior descending arteries (proximal and mid segment, B) and the right coronary artery (proximal vessel segment, D; middle vessel segment, F).
High-res (TIF) version
(Right-click and Save As)
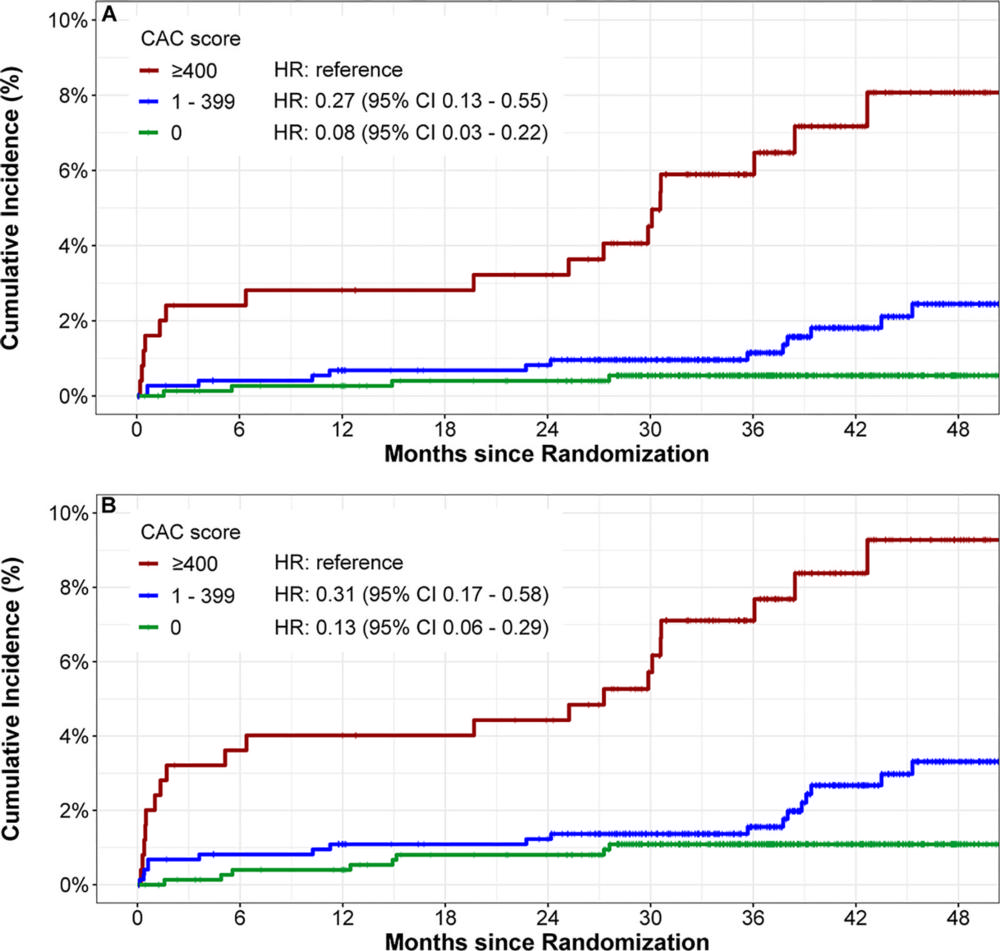
Figure 3. Time-to-event curves for (A) the primary prognostic end point major adverse cardiovascular events (MACE) and (B) secondary prognostic composite end point of expanded MACE (cardiovascular death, myocardial infarction, stroke, transient ischemic attack, or major procedure-related complications). The MACE rate was lower in patients with lower coronary artery calcium (CAC) scores. HR = hazard ratio
High-res (TIF) version
(Right-click and Save As)
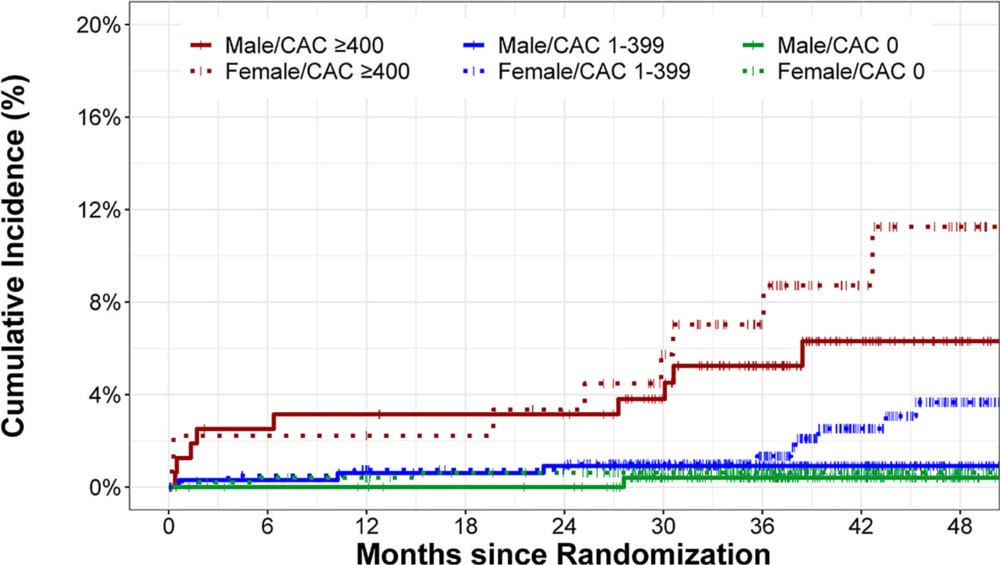
Figure 4. Time-to-event curves for the primary prognostic end point major adverse cardiovascular events (MACE) stratified by sex shows no evidence of a difference between female participants (dotted lines) and male participants (solid lines).
High-res (TIF) version
(Right-click and Save As)

