Novel Technique Has Potential to Transform Breast Cancer Detection
Released: February 09, 2024
At A Glance
- Low-dose positron emission mammography (PEM) provides high sensitivity for detecting breast cancer while significantly reducing the likelihood of false positive results.
- PEM displayed comparable performance to MRI, identifying 24 of 25 invasive cancers (96%), with a false positive rate of 16%, compared with 62% for MRI.
- Unlike traditional mammography, PEM does not require breast compression.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — An innovative breast imaging technique provides high sensitivity for detecting cancer while significantly reducing the likelihood of false positive results, according to a study published today in Radiology: Imaging Cancer, a journal of the Radiological Society of North America (RSNA). Researchers said the technique has the potential to offer more reliable breast cancer screening for a broader range of patients.
Mammography is an effective screening tool for early detection of breast cancer, but its sensitivity is reduced in dense breast tissue. This is due to the masking effect of overlying dense fibroglandular tissue. Since almost half of the screening population has dense breasts, many of these patients require additional breast imaging, often with MRI, after mammography.
Low-dose positron emission mammography (PEM) is a novel molecular imaging technique that provides improved diagnostic performance at a radiation dose comparable to that of mammography.
For the study, 25 women, median age 52, recently diagnosed with breast cancer, underwent low-dose PEM with the radiotracer fluorine 18-labeled fluorodeoxyglucose (18F-FDG). Two breast radiologists reviewed PEM images taken one and four hours post 18F-FDG injection and correlated the findings with lab results.
PEM displayed comparable performance to MRI, identifying 24 of the 25 invasive cancers (96%). Its false positive rate was only 16%, compared with 62% for MRI.
Along with its strong sensitivity and low false-positive rate, PEM could potentially decrease downstream healthcare costs as this study shows it may prevent further unnecessary work up compared to MRI. Additionally, the technology is designed to deliver a radiation dose comparable to that of traditional mammography without the need for breast compression, which can often be uncomfortable for patients.
"The integration of these features—high sensitivity, lower false-positive rates, cost-efficiency, acceptable radiation levels without compression, and independence from breast density—positions this emerging imaging modality as a potential groundbreaking advancement in the early detection of breast cancer," said study lead author Vivianne Freitas, M.D., M.Sc., assistant professor at the University of Toronto. "As such, it holds the promise of transforming breast cancer diagnostics and screening in the near future, complementing or even improving current imaging methods, marking a significant step forward in breast cancer care."
Low-dose PEM offers potential clinical uses in both screening and diagnostic settings, according to Dr. Freitas.
"For screening, its ability to perform effectively regardless of breast density potentially addresses a significant shortcoming of mammography, particularly in detecting cancers in dense breasts where lesions may be obscured," she said. "It also presents a viable option for patients at high risk who are claustrophobic or have contraindications for MRI."
The technology could also play a crucial role in interpreting uncertain mammogram results, evaluating the response to chemotherapy and ascertaining the extent of disease in newly diagnosed breast cancer, including involvement of the other breast.
Dr. Freitas, who is also staff radiologist of the Breast Imaging Division of the Toronto Joint Department of Medical Imaging, University Health Network, Sinai Health System and Women's College Hospital, is currently researching PEM's ability to reduce the high rates of false positives typically associated with MRI scans. Should PEM successfully lower these rates, it could significantly lessen the emotional distress and anxiety linked to false positives, Dr. Freitas said. Additionally, it might lead to a decrease in unnecessary biopsies and treatments.
More studies are needed to determine low-dose PEM's exact role and efficacy in the clinical setting.
"While the full integration of this imaging method into clinical practice is yet to be confirmed, the preliminary findings of this research are promising, particularly in demonstrating the capability of detecting invasive breast cancer with low doses of fluorine-18-labeled FDG," Dr. Freitas said. "This marks a critical first step in its potential future implementation in clinical practice."
"Breast Cancer Detection Using a Low-Dose Positron Emission Digital Mammography System." Collaborating with Dr. Freitas were Xuan Li, Ph.D., Anabel Scaranelo, Ph.D., Frederick Au, M.D., Supriya Kulkarni, M.D., Sandeep Ghai, M.D., Samira Taeb, M.Sc., Oleksandr Bubon, Ph.D., Brandon Baldassi, M.Sc., Borys Komarov, M.Sc., Shayna Parker, M.Sc., Craig A. Macsemchuk, B.Sc., Michael Waterston, M.Sc., M.A., Kenneth O. Olsen, B.Sc., M.B.A., and Alla Reznik, Ph.D.
Radiology: Imaging Cancer is edited by Gary D. Luker, M.D., Michigan Medicine, University of Michigan, Ann Arbor, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/imaging-cancer)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast cancer screening, visit RadiologyInfo.org.
Images (JPG, TIF):
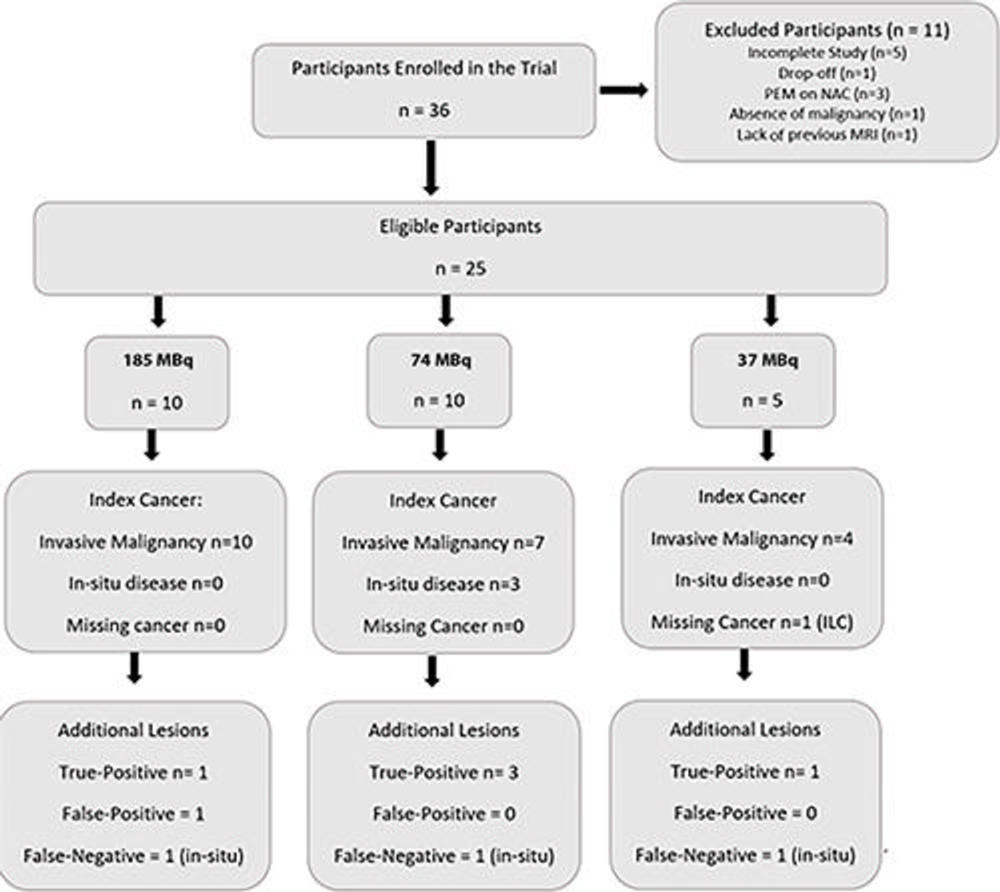
Figure 2. Diagram shows the study workflow. ILC = invasive lobular carcinoma, NAC = neoadjuvant chemotherapy, PEM = positron emission mammography.
High-res (TIF) version
(Right-click and Save As)
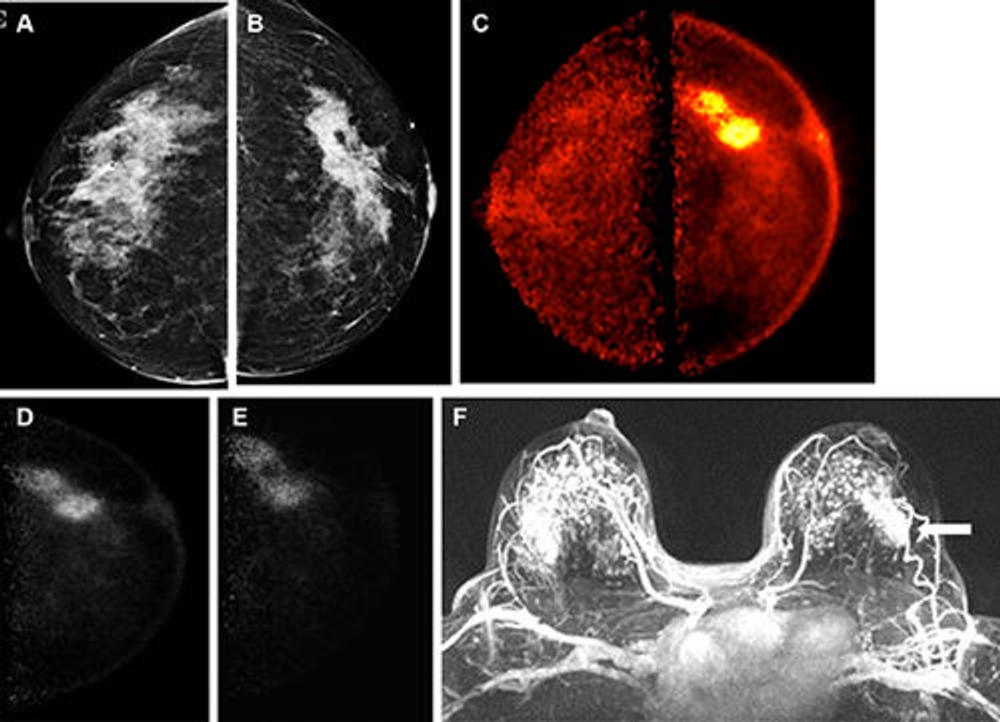
Figure 3. Images obtained in a 50-year-old female patient with a new biopsy-proven malignant lesion in the left breast. (A) Craniocaudal mammogram of the right breast does not show any lesion. (B) The malignant lesion corresponds with a 7.0-cm irregular and spiculated mass on the left craniocaudal mammogram. US-guided core-needle biopsy revealed grade 2 invasive lobular carcinoma. (C) The bilateral positron emission mammographic craniocaudal color image obtained 1 hour after intravenous injection of 185 MBq of fluorine 18–labeled fluorodeoxyglucose (18F-FDG) shows a mass with intense uptake in the left breast with known cancer and no abnormal uptake in the right breast. Positron emission mammographic craniocaudal images of the left breast obtained (D) 1 hour and (E) 4 hours after intravenous injection of 185 MBq of 18F-FDG show no substantial visual difference in uptake of the known cancer. (F) Axial contrast-enhanced fat-saturated subtracted T1-weighted MR image with maximum intensity projection reconstruction obtained 90 seconds after intravenous injection of 0.1 mmol of gadolinium-based contrast material per kilogram of body weight also shows the enhancing mass corresponding to known malignancy (arrow) and marked bilateral background parenchymal enhancement, with multiple nonspecific foci of enhancement in the contralateral breast. The patient opted for bilateral mastectomy, which confirmed left-sided malignancy and no malignancy in the contralateral breast.
High-res (TIF) version
(Right-click and Save As)
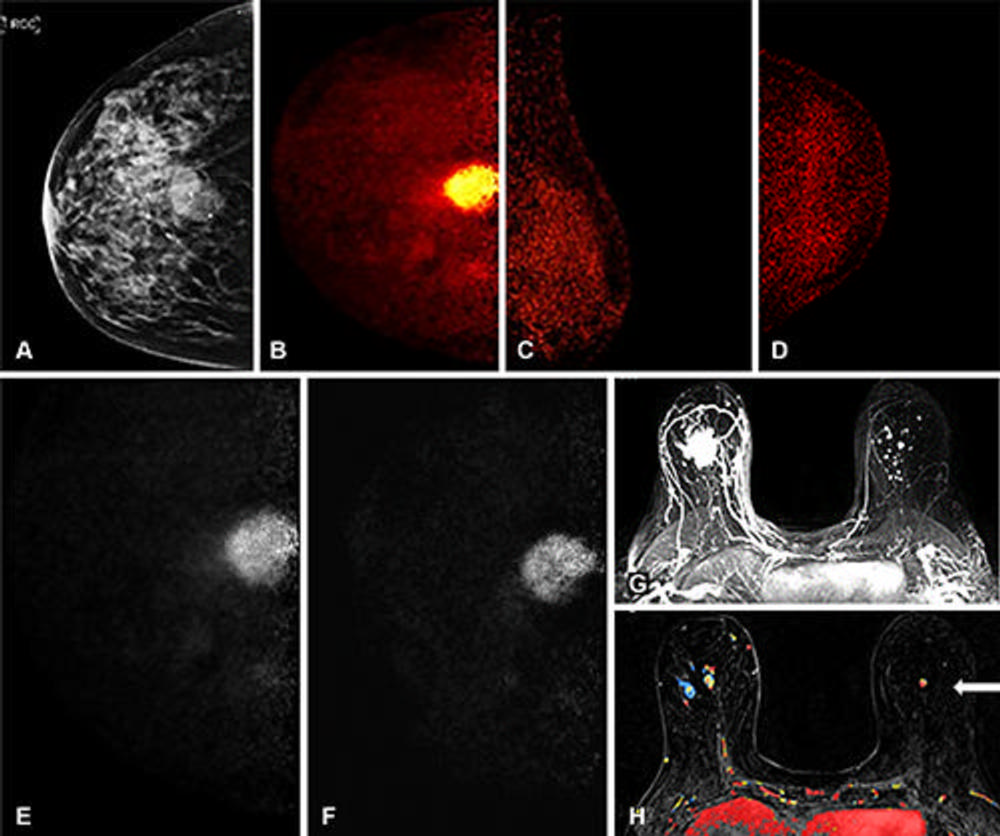
Figure 4. Images obtained in an 85-year-old female patient with a new biopsy-proven malignant lesion in the right breast. (A) The malignant lesion corresponds with a 3.0-cm equal-density mildly irregular mass on right craniocaudal mammogram. US-guided core-needle biopsy revealed grade 3 invasive intracystic papillary carcinoma. (B) Right positron emission mammographic (PEM) craniocaudal color image obtained 1 hour after intravenous injection of 74 MBq of fluorine 18–labeled fluorodeoxyglucose (18F-FDG) shows a 3.2-cm mass (known cancer) with intense uptake. Left PEM (C) mediolateral oblique and (D) craniocaudal color images obtained 1 hour after intravenous injection of 74 MBq of 18F-FDG do not show any abnormal uptake. Right PEM craniocaudal images obtained (E) 1 hour and (F) 4 hours after intravenous injection of 74 MBq of 18F-FDG show no substantial visual difference in uptake of the known cancer. (G, H) Axial contrast-enhanced fat-saturated subtracted T1-weighted MR images with maximum intensity projection reconstruction obtained 90 seconds after intravenous injection of 0.1 mmol of gadolinium-based contrast material per kilogram of body weight also show the enhancing mass corresponding to known malignancy and multiple nonspecific foci of enhancement in the contralateral breast, the largest in the left central breast with washout kinetics (arrow in H). Left-sided MRI-guided biopsy confirmed benign intraductal papilloma. The patient underwent a right lumpectomy with sentinel lymph node biopsy. The final pathologic result confirmed 3.2-cm grade 3 invasive intracystic papillary carcinoma with negative sentinel lymph node biopsy.
High-res (TIF) version
(Right-click and Save As)
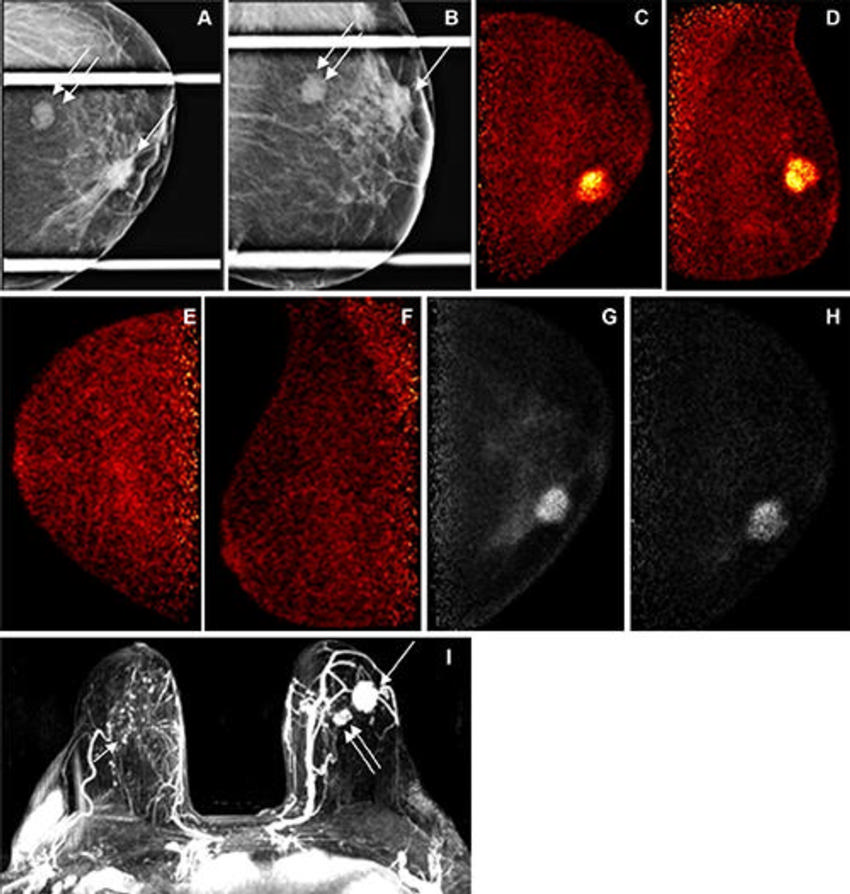
Figure 5. Images obtained in a 69-year-old female patient with a new biopsy-proven malignant lesion in the left breast. (A, B) The malignant lesion corresponds with a 2.5-cm irregular and spiculated mass (arrow) and an additional oval and circumscribed mass (double arrows) on left mediolateral oblique and craniocaudal spot compression mammographic views. US-guided core-needle biopsy revealed grade 3 invasive ductal carcinoma (arrow) and fibroadenoma (double arrow). Left positron emission mammographic (PEM) (C) craniocaudal and (D) mediolateral oblique color images obtained 1 hour after intravenous injection of 74 MBq of fluorine 18–labeled fluorodeoxyglucose (18F-FDG) show a mass (known cancer) with intense uptake and no uptake in the biopsy-proven fibroadenoma. Right PEM (E) craniocaudal and (F) mediolateral oblique color images obtained 1 hour after intravenous injection of 74 MBq of 18F-FDG do not show any abnormal uptake. Left PEM craniocaudal images obtained (G) 1 hour and (H) 4 hours after intravenous injection of 74 MBq of 18F-FDG show no substantial visual difference in uptake of known cancer. (I) Axial contrast-enhanced fat-saturated subtracted T1-weighted MR image with maximum intensity projection reconstruction obtained 90 seconds after intravenous injection of 0.1 mmol of gadolinium-based contrast material per kilogram of body weight also shows the left-sided enhancing mass (arrow) corresponding to known malignancy and the biopsy-proven fibroadenoma (double arrows), as well as multiple nonspecific foci of enhancement in the contralateral breast, with one being the most conspicuous (arrow). The patient underwent bilateral lumpectomy. The final pathologic results in the left breast confirmed grade 3 invasive ductal carcinoma and yielded atypical ductal hyperplasia in the right breast.
High-res (TIF) version
(Right-click and Save As)

