AI May Aid in Diagnosing Adolescents with ADHD
Released: November 29, 2023
At A Glance
- Using AI, researchers found significant differences in nine areas of the brain’s white matter in adolescents with ADHD.
- The AI deep learning model was trained using brain imaging data from 1,704 participants in the Adolescent Brain Cognitive Development Study.
- The findings show promise for an objective method of diagnosis of the condition affecting 5.7 million children and adolescents in the U.S.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
CHICAGO — Using artificial intelligence (AI) to analyze specialized brain MRI scans of adolescents with and without attention-deficit/hyperactivity disorder (ADHD), researchers found significant differences in nine brain white matter tracts in individuals with ADHD. Results of the study will be presented today at the annual meeting of the Radiological Society of North America (RSNA).
ADHD is a common disorder often diagnosed in childhood and continuing into adulthood, according to the Centers for Disease Control and Prevention. In the U.S., an estimated 5.7 million children and adolescents between the ages of 6 and 17 have been diagnosed with ADHD.
“ADHD often manifests at an early age and can have a massive impact on someone’s quality of life and ability to function in society,” said study co-author Justin Huynh, M.S., a research specialist in the Department of Neuroradiology at the University of California, San Francisco, and medical student at the Carle Illinois College of Medicine at Urbana-Champaign. “It is also becoming increasingly prevalent in society among today’s youth, with the influx of smartphones and other distracting devices readily accessible.”
Children with ADHD may have trouble paying attention, controlling impulsive behaviors or regulating activity. Early diagnosis and intervention are key to managing the condition.
“ADHD is extremely difficult to diagnose and relies on subjective self-reported surveys,” Huynh said. “There is definitely an unmet need for more objective metrics for diagnosis. That’s the gap we are trying to fill.”
Huynh said this is the first study to apply deep learning, a type of AI, to identify markers of ADHD in the multi-institutional Adolescent Brain Cognitive Development (ABCD) Study, which includes brain imaging, clinical surveys and other data on over 11,000 adolescents from 21 research sites in the U.S. The brain imaging data included a specialized type of MRI called diffusion-weighted imaging (DWI).
“Prior research studies using AI to detect ADHD have not been successful due to a small sample size and the complexity of the disorder,” Huynh said.
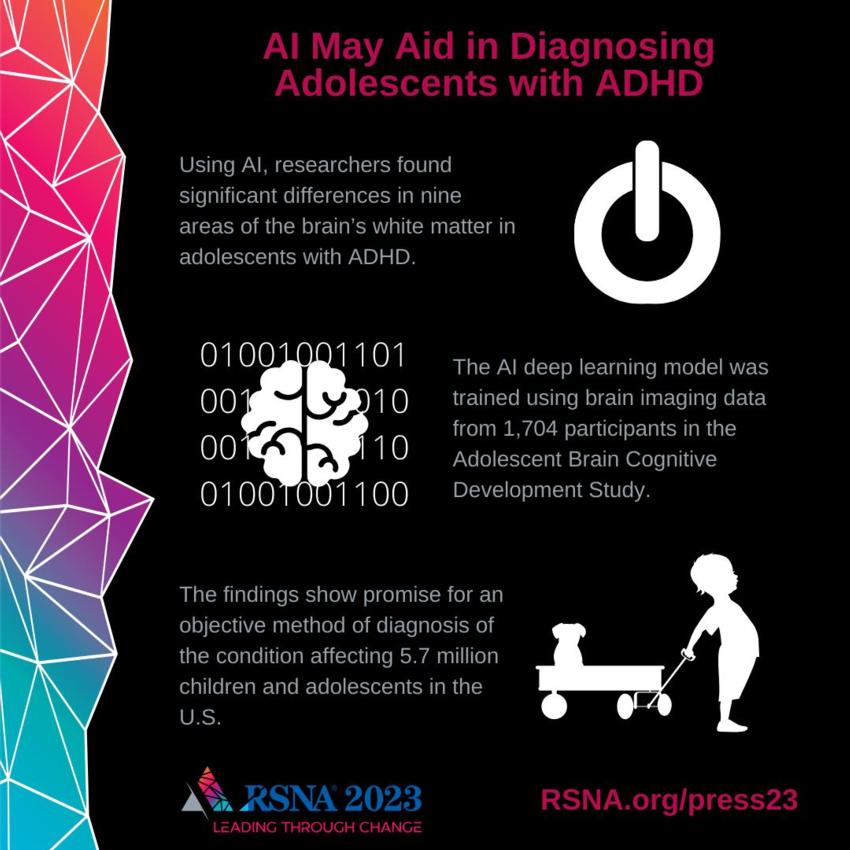
The research team selected a group of 1,704 individuals from the ABCD dataset, including adolescents with and without ADHD. Using DWI scans, the researchers extracted fractional anisotropy (FA) measurements along 30 major white matter tracts in the brain. FA is a measure of how water molecules move along the fibers of white matter tracts.
The FA values from 1,371 individuals were used as input for training a deep-learning AI model, which was then tested on 333 patients, including 193 diagnosed with ADHD and 140 without. ADHD diagnoses were determined by the Brief Problem Monitor assessment, a rating tool used for monitoring a child’s functioning and their responses to interventions.
With the help of AI, the researchers discovered that in patients with ADHD, FA values were significantly elevated in nine white matter tracts.
“These differences in MRI signatures in individuals with ADHD have never been seen before at this level of detail,” Huynh said. “In general, the abnormalities seen in the nine white matter tracts coincide with the symptoms of ADHD.”
The researchers intend to continue obtaining data from the rest of the individuals in the ABCD dataset, comparing the performance of additional AI models.
“Many people feel that they have ADHD, but it is undiagnosed due to the subjective nature of the available diagnostic tests,” Huynh said. “This method provides a promising step towards finding imaging biomarkers that can be used to diagnose ADHD in a quantitative, objective diagnostic framework,” Huynh said.
Co-authors are Pierre F. Nedelec, M.S., M.T.M., Samuel Lashof-Regas, Michael Romano, M.D., Ph.D., Leo P. Sugrue, M.D., Ph.D., and Andreas M. Rauschecker, M.D., Ph.D.
Note: Copies of RSNA 2023 news releases and electronic images will be available online at RSNA.org/press23.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
Editor’s note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA Newsroom at 1-312-791-6610.
For patient-friendly information on brain MRI, visit RadiologyInfo.org.
Video (MP4):
Images (JPG, TIF):
Figure 1. (A) Diffusion MRI white matter tract fractional anisotropy (FA) average anomaly score (mean absolute error) profiles from autoencoder for all cases with ADHD (blue) and without ADHD (orange). (B) Difference between average anomaly score profiles for all cases with ADHD and without ADHD. (C) Average anomaly scores by tract, for cases with ADHD and without ADHD. (D) P-values (t-test) comparing average anomaly scores for cases with ADHD and without ADHD by white matter tract, reveals significant differences in 9 out of 30 tracts.
High-res (TIF) version
(Right-click and Save As)
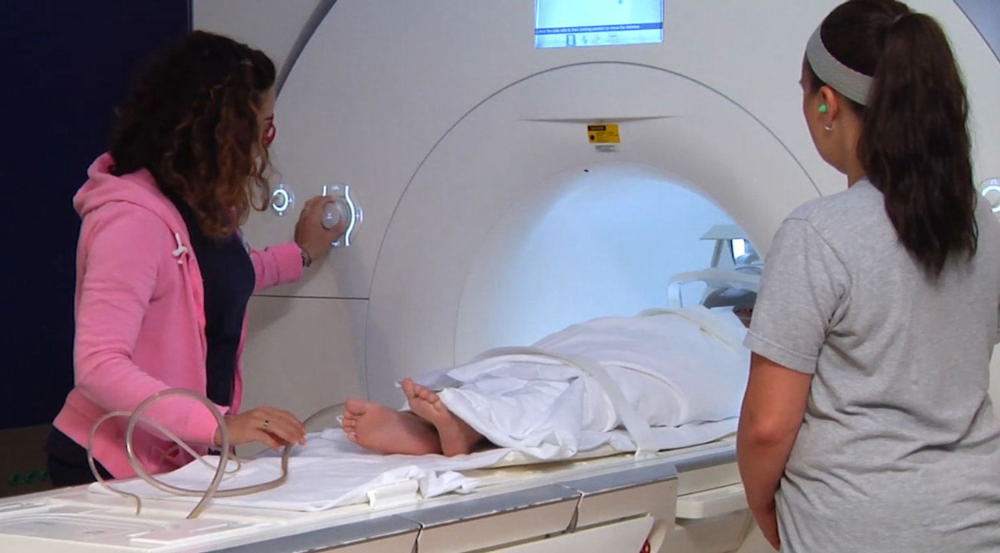
Figure 2. Child undergoing pediatric MRI. (Courtesy of RadiologyInfo.org)
High-res (TIF) version
(Right-click and Save As)
Additional Resources