Screening Sharply Improves Lung Cancer Long-term Survival
Released: November 07, 2023
At A Glance
- Early detection of lung cancer with low-dose CT screening drastically improves the long-term survival rate.
- The results of the large-scale international study showed that the overall 20-year survival rate screening participants who were diagnosed with early-stage lung cancer was 81%.
- This is the first published study of 20-year survival rates from lung cancer screening.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Diagnosing early-stage lung cancer with low-dose CT screening dramatically improves the long-term survival rate of cancer patients, according to a large-scale, 20-year international study published today in Radiology, a journal of the Radiological Society of North America (RSNA). The results show that patients diagnosed with lung cancer by low-dose CT screening have a 20-year survival rate of 81%. If diagnosed in the earliest Stage I, long-term survival was 95%.
"It is the first time that 20-year survival rates from annual screening have been reported," said the study's lead author, Claudia Henschke, Ph.D., M.D., professor of radiology and director of the Early Lung and Cardiac Action Program at the Icahn School of Medicine at Mount Sinai in New York. "This 20-year survival rate of 81% is the estimated cure rate of all participants with lung cancers diagnosed by annual screening. This is a huge benefit compared to waiting for a diagnosis that, in usual care, is symptom-prompted."
Lung cancer is the leading cause of cancer death. According to the American Lung Association, the average lung cancer five-year survival rate is 18.6%. Only 16% of lung cancers are diagnosed at an early stage, and more than half of people with lung cancer die within one year of being diagnosed.
While treatments of more advanced-stage cancers with targeted therapy and immunotherapy have come a long way, the best tool in the fight against cancer deaths is early diagnosis through low-dose CT screening before symptoms appear.
Since 1992, Dr. Henschke and colleagues have been studying the effectiveness of low-dose CT screening for lung cancer. This led to the creation of the International Early Lung Cancer Action Program (I-ELCAP) which has enrolled more than 89,000 participants in over 80 institutions worldwide. This international program will continue its collaborations in 2024 with clinical and government organizations to roll out lung screening programs for underserved and low-income countries on two additional continents.
In 2006, the researchers identified a 10-year survival rate of 80% for the patients whose cancer was identified by CT screening. For this study, they looked at 20-year survival rates.
"We were excited to see that the estimated cure rate we reported in 2006 has persisted after 20 years of follow-up," Dr. Henschke said.
The new study also found that among the 1,257 I-ELCAP participants diagnosed with lung cancer, 81% had Stage I disease. A Stage I lung cancer is a very small tumor that has not spread to any lymph nodes. In this study, the long-term survival rate for Stage I cancers was 87%.
The findings demonstrate the importance of low-dose CT screening for early detection of lung cancer.
The researchers also included participants who have smoked less than 10 pack-years, including those who had never smoked cigarettes but had passive exposure to cigarette smoke.
"The less than 10 pack-years of smoking includes people who have never smoked," Dr. Henschke said. "In the United States, some 25% of lung cancers are diagnosed in people who have never smoked."
The results from this study show that after 20 years, patients diagnosed with lung cancer at an early stage via CT screening have significantly better outcomes. By treating the cancer when it is small, patients can be effectively cured in the long term.
"Lung cancer can be cured if you enroll in an annual screening program using a well-defined protocol and comprehensive management system," Dr. Henschke said. "It is important to return for annual screening."
The U.S. Preventive Services Task Force recommends annual lung cancer screening with low-dose CT in adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years.
On November 1, the American Cancer Society updated its lung cancer screening guidelines to recommend low-dose CT screening for people aged 50 to 80 years who currently smoke or formerly smoked and have a 20 pack-year or greater history of smoking. The guidelines also eliminated "years since quitting" as inclusion or exclusion criteria for screening.
"A 20-year Follow-up of the International Early Lung Cancer Action Program (I-ELCAP)." Collaborating with Dr. Henschke were Rowena Yip, Ph.D., M.P.H., Dorith Shaham, M.D., Steve Markowitz, M.D., Jose Cervera Deval, M.D., Javier J. Zulueta, M.D., Luis M. Seijo, M.D., Cheryl Aylesworth, M.D., Karl Klingler, M.D., Shahriyour Andaz, M.D., Cynthia Chin, M.D., James P. Smith, M.D., Emanuela Taioli, M.D., Ph.D., Nasser Altorki, M.D., Raja M. Flores, M.D., M.P.H., and David F. Yankelevitz, M.D., for the International Early Lung Cancer Action Program Investigators.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology's legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on lung cancer screening, visit RadiologyInfo.org.
Press Resources:
Images (JPG, TIF):
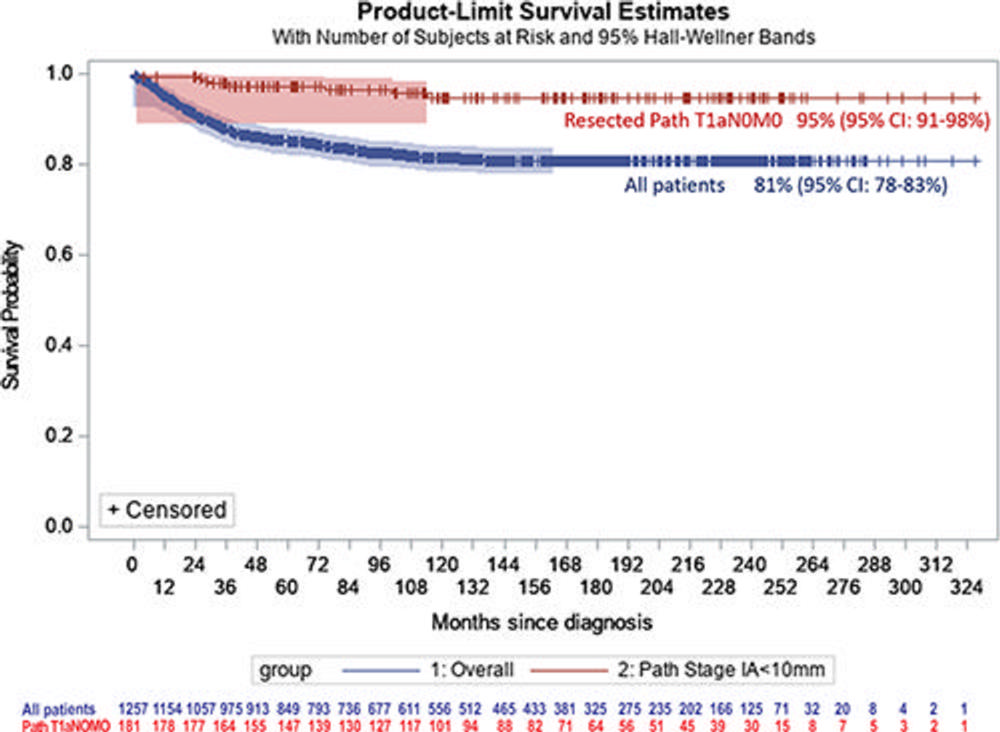
Figure 1. Kaplan-Meier curve shows lung cancer–specific survival for all 1,257 participants with lung cancer and for the 181 participants undergoing resection with resulting pT1aN0M0 and tumor size of 10 mm or less in the pathology specimen.
High-res (TIF) version
(Right-click and Save As)
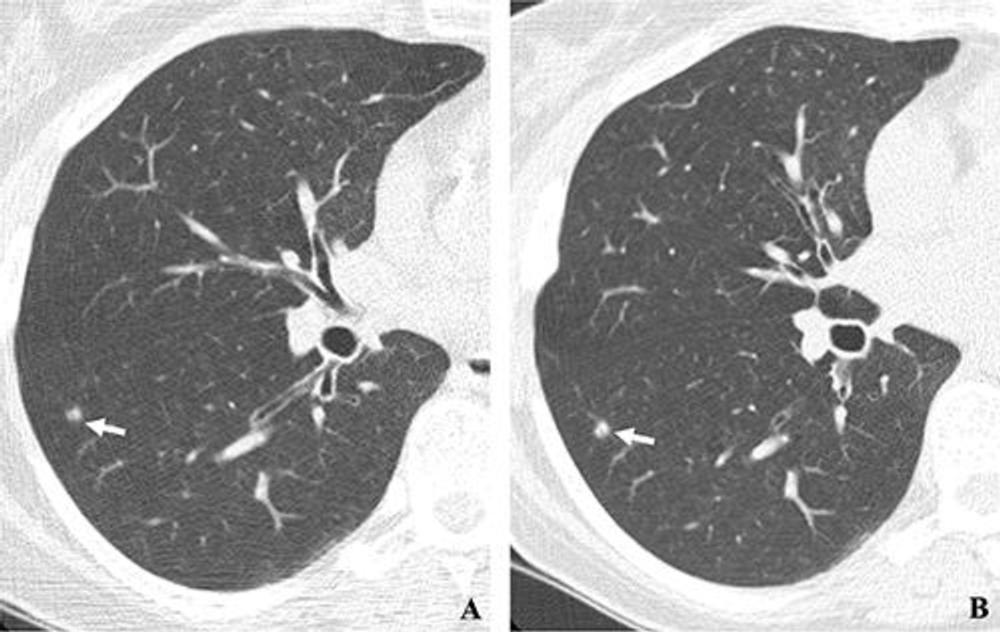
Figure 2. (A, B) Two annual repeat low-dose CT scans in a woman who was 60 years old at baseline enrollment in 1999. At baseline enrollment, she was currently smoking and had a 30-pack-year smoking history. No nodules were identified on baseline low-dose CT scans. On the sixth annual low-dose CT scan (B) , a right lower lobe solid nodule (arrow) measuring 4.5 mm in maximum diameter was identified. The nodule could be identified in retrospect on the prior annual CT scan (arrow in A), when it measured 2.0 mm in maximum diameter. Estimated tumor volume doubling time was 161 days. Lobectomy was performed 2 months later, and diagnosis of stage 1aN0M0 moderately differentiated adenocarcinoma measuring 6.0 mm in maximum diameter was made. Expert pathologic panel review (22) of the pathologic specimen updated the diagnosis to adenocarcinoma with mixed subtype (80% acinar, 20% bronchoalveolar carcinoma components) with 5 mm of invasion.
High-res (TIF) version
(Right-click and Save As)
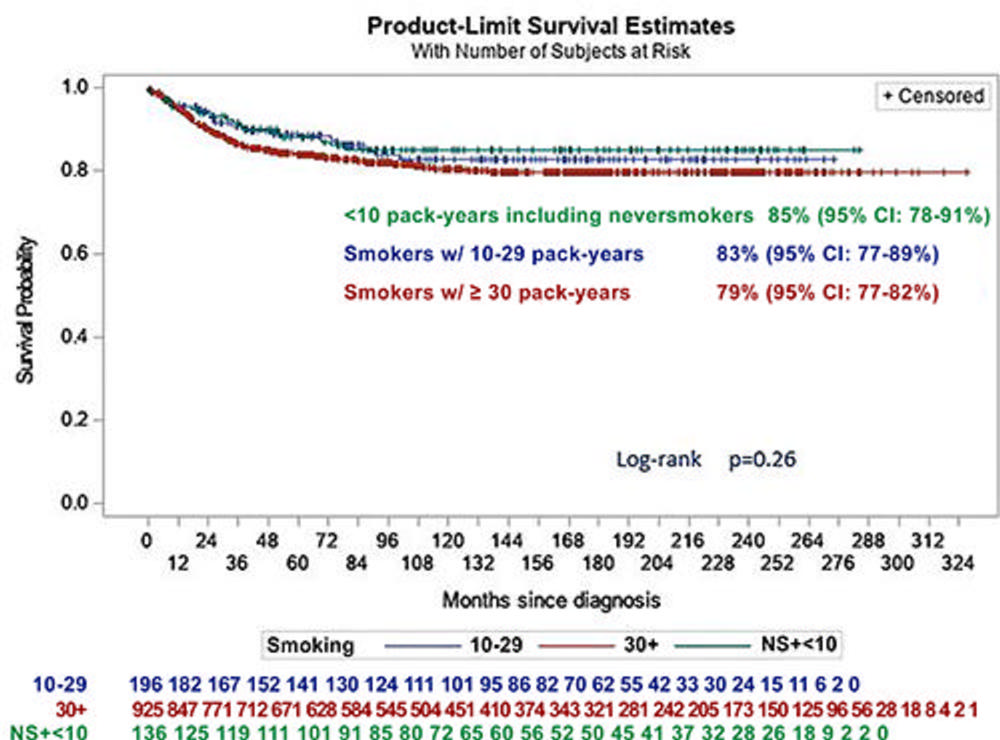
Figure 3. Kaplan-Meier curve shows lung cancer–specific survival for all 1,257 participants with lung cancer, organized by smoking categories (participants who never smoked or who smoked less than 10 pack-years, participants who smoked 10–29 pack-years, and participants who smoked at least 30 pack-years).
High-res (TIF) version
(Right-click and Save As)
