AI Outperformed Standard Risk Model for Predicting Breast Cancer
Released: June 06, 2023
At A Glance
- AI algorithms outperformed a standard clinical risk model for predicting the five-year risk for breast cancer.
- This strong predictive performance suggests AI can identify both missed cancers and breast tissue features that help predict future cancer development.
- Breast cancer risk is currently calculated using clinical risk models like the Breast Cancer Surveillance Consortium risk model.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — In a large study of thousands of mammograms, artificial intelligence (AI) algorithms outperformed the standard clinical risk model for predicting the five-year risk for breast cancer. The results of the study were published in Radiology, a journal of the Radiological Society of North America (RSNA).
A woman's risk of breast cancer is typically calculated using clinical models such as the Breast Cancer Surveillance Consortium (BCSC) risk model, which uses self-reported and other information on the patient—including age, family history of the disease, whether she has given birth, and whether she has dense breasts—to calculate a risk score.
"Clinical risk models depend on gathering information from different sources, which isn't always available or collected," said lead researcher Vignesh A. Arasu, M.D., Ph.D., a research scientist and practicing radiologist at Kaiser Permanente Northern California. "Recent advances in AI deep learning provide us with the ability to extract hundreds to thousands of additional mammographic features."
In the retrospective study, Dr. Arasu used data associated with negative (showing no visible evidence of cancer) screening 2D mammograms performed at Kaiser Permanente Northern California in 2016. Of the 324,009 women screened in 2016 who met eligibility criteria, a random sub-cohort of 13,628 women was selected for analysis. Additionally, all 4,584 patients from the eligibility pool who were diagnosed with cancer within five years of the original 2016 mammogram were also studied. All the women were followed until 2021.
"We selected from the entire year of screening mammograms performed in 2016, so our study population is representative of communities in Northern California," Dr. Arasu said.
The researchers divided the five-year study period into three time periods: interval cancer risk, or incident cancers diagnosed between 0 and 1 years; future cancer risk, or incident cancers diagnosed from between one and five years; and all cancer risk, or incident cancers diagnosed between 0 and 5 years.
Using the 2016 screening mammograms, risk scores for breast cancer over the five-year period were generated by five AI algorithms, including two academic algorithms used by researchers and three commercially available algorithms. The risk scores were then compared to each other and to the BCSC clinical risk score.
"All five AI algorithms performed better than the BCSC risk model for predicting breast cancer risk at 0 to 5 years," Dr. Arasu said. "This strong predictive performance over the five-year period suggests AI is identifying both missed cancers and breast tissue features that help predict future cancer development. Something in mammograms allows us to track breast cancer risk. This is the 'black box' of AI."
Some of the AI algorithms excelled at predicting patients at high risk of interval cancer, which is often aggressive and may require a second reading of mammograms, supplementary screening or short-interval follow-up imaging. When evaluating women with the highest 10% risk as an example, AI predicted up to 28% of cancers compared to 21% predicted by BCSC.
Even AI algorithms trained for short time horizons (as low as 3 months) were able to predict the future risk of cancer up to five years when no cancer was clinically detected by screening mammography. When used in combination, the AI and BCSC risk models further improved cancer prediction.
"We're looking for an accurate, efficient and scalable means of understanding a women's breast cancer risk," Dr. Arasu said. "Mammography-based AI risk models provide practical advantages over traditional clinical risk models because they use a single data source: the mammogram itself."
Dr. Arasu said some institutions are already using AI to help radiologists detect cancer on mammograms. A person's future risk score, which takes seconds for AI to generate, could be integrated into the radiology report shared with the patient and their physician.
"AI for cancer risk prediction offers us the opportunity to individualize every woman's care, which isn't systematically available," he said. "It's a tool that could help us provide personalized, precision medicine on a national level."
"Comparison of Mammography AI Algorithms with a Clinical Risk Model for 5-year Breast Cancer Risk Prediction: An Observational Study." Collaborating with Dr. Arasu were Laurel A. Habel, Ph.D., Ninah S. Achacoso, M.S., Diana S. M. Buist, Ph.D., Jason B. Cord, M.D., Laura J. Esserman, M.D., Nola. M. Hylton, Ph.D., M. Maria Glymour, Sc.D., John Kornak, Ph.D., Lawrence H. Kushi, Sc.D., Don A. Lewis, M.S., Vincent X. Liu, M.D., Caitlin M. Lydon, M.P.H., Diana L. Miglioretti, Ph.D., Daniel A. Navarro, M.D., Albert Pu, M.S., Li Shen, Ph.D., Weiva Sieh, M.D., Ph.D., Hyo-Chun Yoon, M.D., Ph.D., and Catherine Lee, Ph.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology's legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
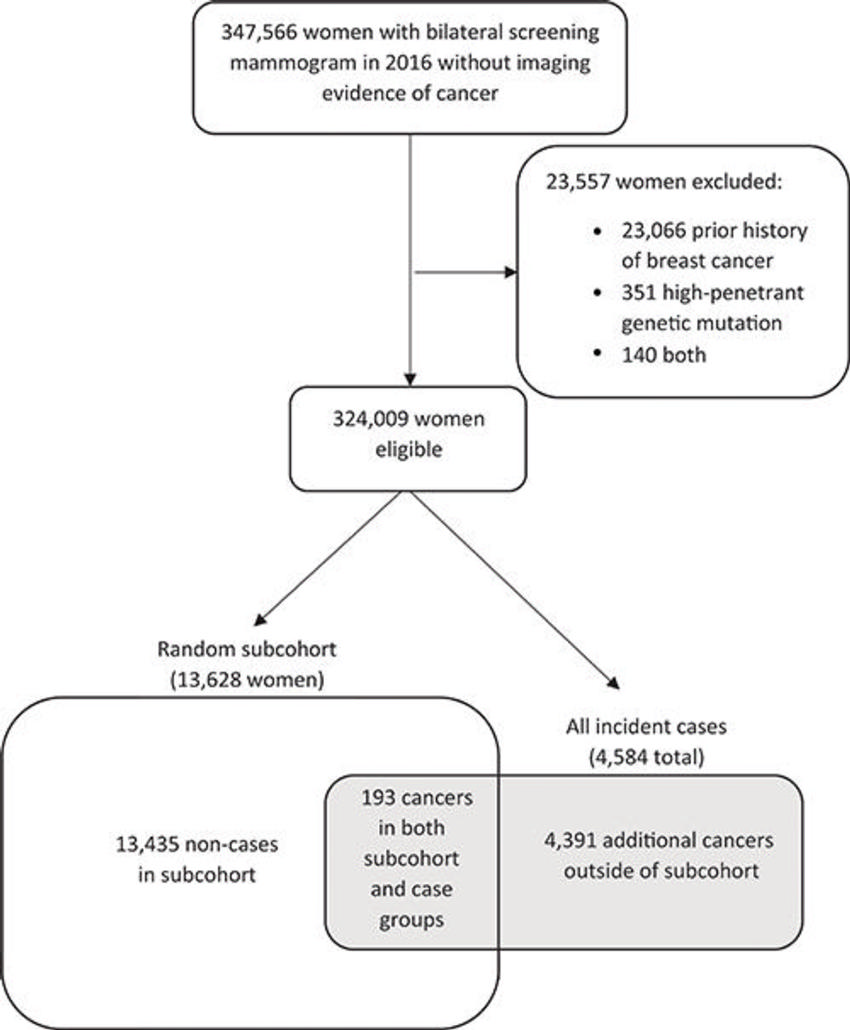
Figure 1. Patient selection flowchart. No imaging evidence of cancer: Screening examination Breast Imaging Reporting and Data System (BI-RADS) 1 or 2, or screening BI-RADS 0 and diagnostic BI-RADS 1 or 2 in 90 days or fewer, or screening BI-RADS 0 and diagnostic BI-RADS 4 or 5 and benign biopsy in 90 days or fewer.
High-res (TIF) version
(Right-click and Save As)
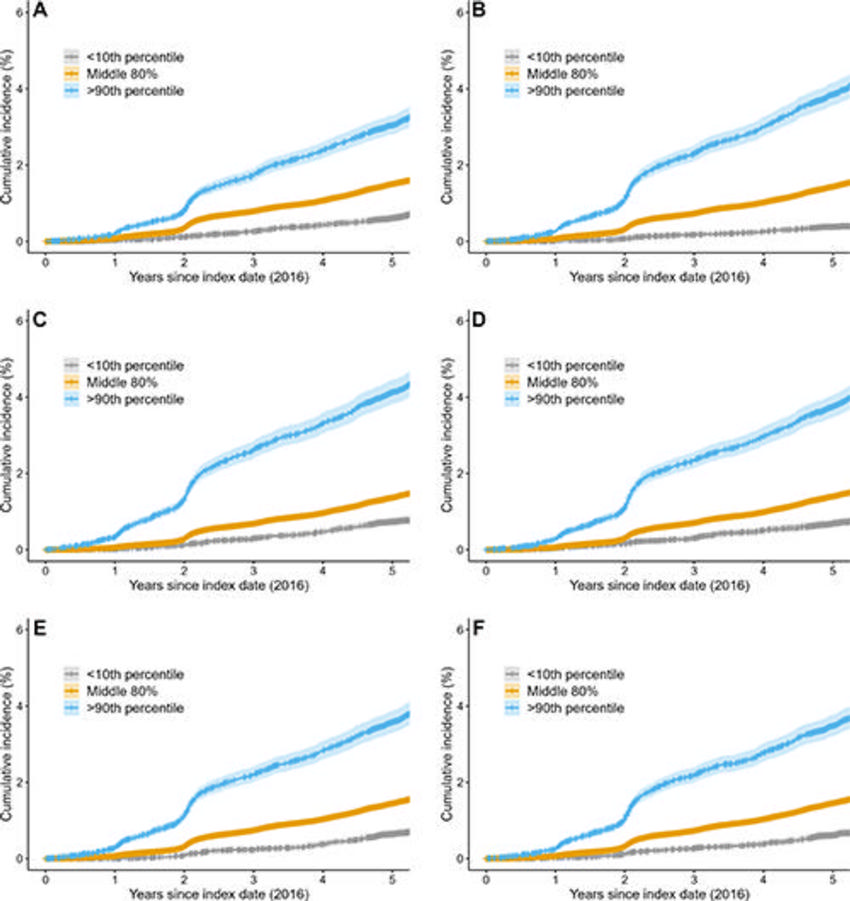
Figure 2. Cumulative risk of breast cancer by risk model type at 5 years. Kaplan-Meier curves for (A) the clinical Breast Cancer Surveillance Consortium (BCSC) risk model and for the mammography-trained artificial intelligence (AI) risk models (B) Mirai, (C) MammoScreen, (D) ProFound, (E) Mia, and (F) Globally-Aware Multiple Instance Classifier. Women with a BCSC risk greater than 90th percentile accounted for 21% of all cancers by 5 years, whereas women with less than 10th percentile risk accounted for 3% of all cancers. Women with AI risk greater than 90th percentile accounted for 24%–28% of all cancers by 5 years, whereas women with less than 10th percentile risk accounted for approximately 2%–5% of cancers across all AI algorithms. The blue line represents women with a risk score greater than 90th percentile, the orange line represents women with a risk score in the middle 80 percentile, and the gray line represents women with a risk score in the less than 10th percentile. Shading surrounding the line is the 95% CI.
High-res (TIF) version
(Right-click and Save As)

Figure 3. Right medial lateral oblique (RMLO) screening mammograms show negative results from 2016 in (A) a 73-year-old woman with Mirai artificial intelligence (AI) risk score with more than 90th percentile risk who developed right breast cancer in 2021 at 5 years of follow-up and (B) a 73-year-old woman with Mirai AI risk score with less than 10th percentile risk who did not develop cancer at 5 years after 5 years of follow-up.
High-res (TIF) version
(Right-click and Save As)
