AI Helpful in Triaging Breast Masses in Low-Resource Areas
Released: May 02, 2023
At A Glance
- AI can analyze breast mass images from low-cost portable ultrasound machines and accurately identify cancer.
- AI correctly identified 96% to 98% of women with cancer on portable ultrasound or standard-of-care ultrasound images.
- In low-resource areas, AI could be a useful tool in identifying breast masses needing urgent attention.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Artificial intelligence (AI) can analyze breast mass images from low-cost portable ultrasound machines and accurately identify cancer, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA). This could prove useful for triage in low-resource settings.
Breast lumps are often found accidentally, during breast self-exam or during a breast exam by a medical professional. Breast cancer screening can find cancers in the breast before the lump can be felt.
While cancer screening has been the focus in Western countries, low- and middle-income countries often lack access to organized screening programs and technology.
In low- and middle-income countries, breast cancer most commonly presents as a palpable lump in the breast. Ultrasound can play a critical role in early detection, resulting in more effective, less invasive treatment and improved outcomes.
“Women in low- and middle-income countries often cannot access breast health care for many months, even when they feel a lump in their breast that may be cancer,” said the study’s lead author Wendie A. Berg, M.D., Ph.D., professor of radiology at the University of Pittsburgh School of Medicine in Pittsburgh, Pennsylvania. “Our study looked at using AI to evaluate breast ultrasound images to distinguish suspicious breast masses needing urgent attention from those that were not cancer.”
For the multicenter study, participants with at least one palpable breast lump were enrolled in Jalisco, Mexico, from December 2017 through May 2021. Ultrasound images were obtained first with portable ultrasound at the site of the lump and adjacent tissue. Women were then imaged with standard-of-care ultrasound. Breast Imaging-Reporting and Data System (BI-RADS) assessments were performed by a radiologist.
After exclusions, 758 masses in 300 women (mean age 50.0 years) were analyzed by the AI software as benign, probably benign, suspicious or malignant (cancerous). The mean patient age was 50.0 years (range 18-92), and the mean largest lesion diameter was 13 mm (range 2-54). Of 758 masses, 360 (47.5%) were palpable, and 56 (7.4%) malignant.
AI correctly identified 96% and 98% of the women with cancer on the low-cost portable ultrasound and standard-of-care ultrasound images, respectively. Of the benign masses, 67% could have been appropriately triaged with standard-of-care ultrasound, and 38% with portable ultrasound.
Although specificity was less than with standard-of-care equipment, AI applied to portable breast ultrasound can potentially reduce about half of specialized hospital referrals in resource-limited regions.
Dr. Berg noted that the researchers did not train AI on images from the portable ultrasound. She also said that low-cost portable ultrasound technology has improved since the study was conducted. With better images and AI training, the researchers expect even better results in the future.
“Our results show great promise for the use of AI and portable ultrasound in low-resource settings, including remote/underserved areas in the United States, to help improve breast health care,” Dr. Berg said. “In reducing the number of women with benign lumps who need to be seen in central facilities and potentially have a biopsy, health care resources can be better focused on women with cancer and reduce delays in diagnosis. This should improve access, health equity and outcomes for women.”
“Toward AI-supported US Triage of Women with Palpable Breast Lumps in a Low-Resource Setting.” Collaborating with Dr. Berg were Ana-Lilia López Aldrete, M.D., Ajit Jairaj, B.S., Juan Carlos Ledesma Parea, M.D., Claudia Yolanda Garcia, M.D., R. Chad McClennan, M.B.A., Steven Yong Cen, Ph.D., Linda H. Larsen, M.D., M. Teresa Soler de Lara, M.S., and Susan Love, M.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology’s legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
Images (JPG, TIF):
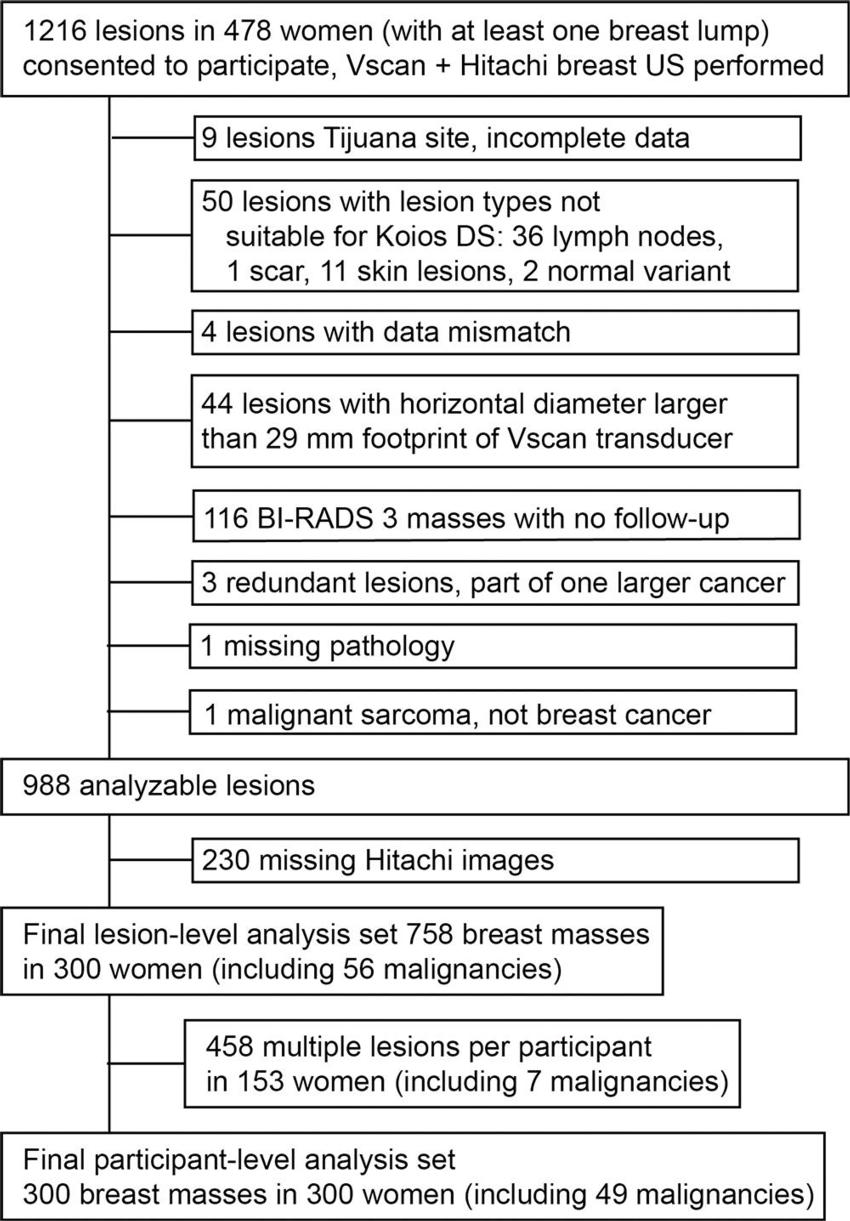
Figure 1. Flowchart shows study population, exclusions, and final analysis set. Multiple lesions per participant were excluded. The palpable mass was retained. If there were multiple palpable masses, the malignant mass was retained. If there were multiple palpable malignancies, we arbitrarily retained the first lesion listed by the site radiologist. BI-RADS = Breast Imaging Reporting and Data System.
High-res (TIF) version
(Right-click and Save As)
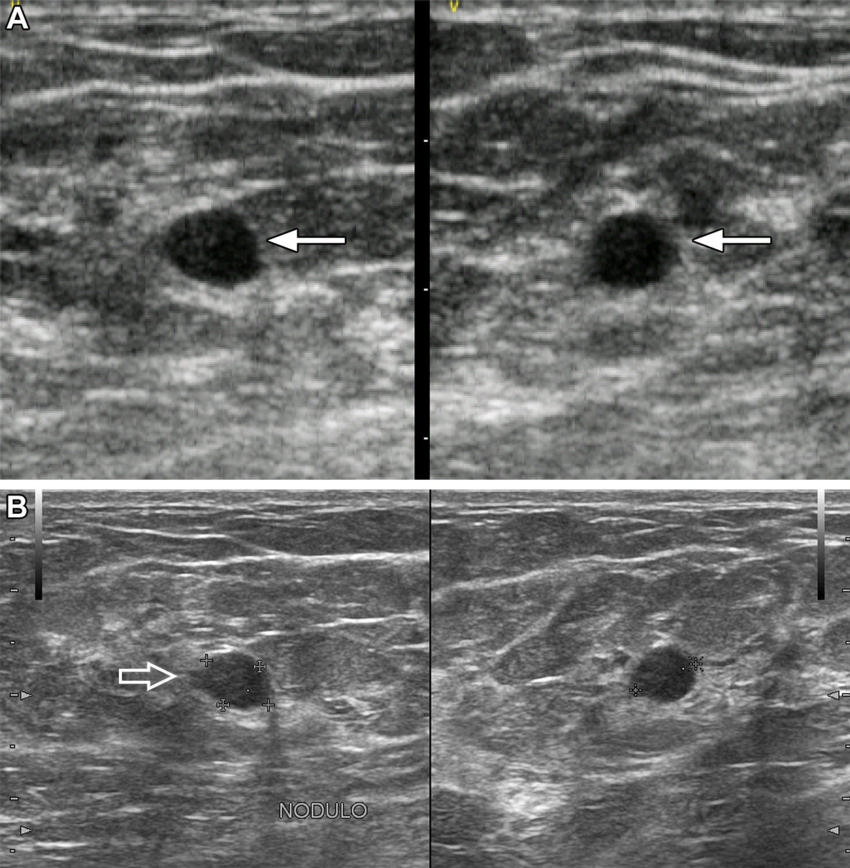
Figure 2. Images in a 37-year-old woman show a palpable mass due to low-grade ductal carcinoma in situ. (A) Orthogonal portable US images show a hypoechoic oval mass with subtly indistinct margins (arrows), assessed as probably benign by artificial intelligence (AI). (B) Orthogonal standard-of-care US images show focal microlobulation (arrow) and were assessed as suspicious with AI and as Breast Imaging Reporting and Data System 4A by the radiologist. US-guided core biopsy and excision showed estrogen and progesterone receptor positive low-grade ductal carcinoma in situ.
High-res (TIF) version
(Right-click and Save As)
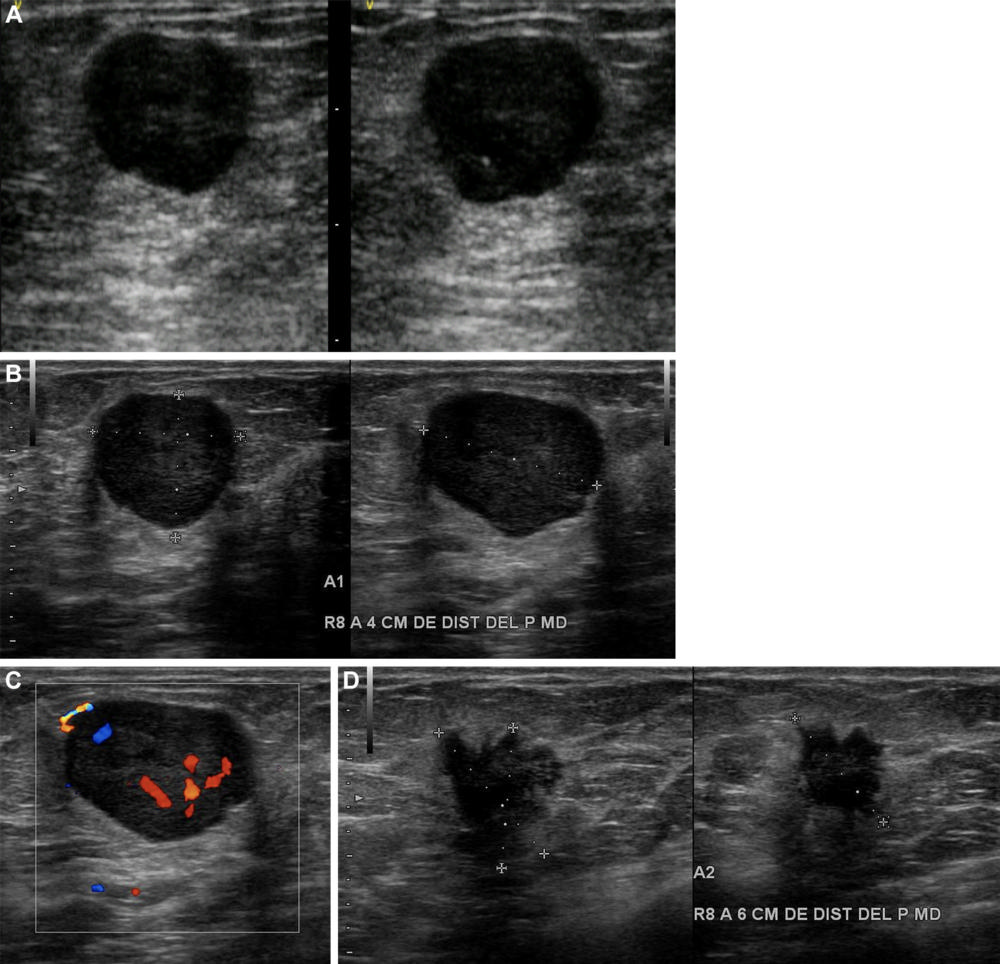
Figure 3. Images in a 60-year-old woman show two palpable masses in the outer right breast. (A) Orthogonal portable US images of mass in right breast at 8 o’clock axis, 4 cm from the nipple, assessed as suspicious by artificial intelligence (AI). (B) Orthogonal standard-of-care (SOC) US images of the same 19-mm mass show circumscribed margins and posterior enhancement. SOC images of the mass were assessed as probably benign by AI and Breast Imaging Reporting and Data System (BI-RADS) 4A, low suspicion, by the radiologist. (C) Color Doppler US image shows strong internal vascularity. Doppler images are not currently evaluated by AI. (D) Orthogonal US images of second palpable mass in right breast at 8 o’clock axis, 6 cm from the nipple, show an irregular 17-mm hypoechoic spiculated mass with posterior shadowing, assessed as probably malignant by AI and BI-RADS 5 by the radiologist. Histopathologic examination of both masses showed grade 3 invasive ductal carcinoma that was estrogen and progesterone receptor positive and human epidermal growth factor receptor 2 negative.
High-res (TIF) version
(Right-click and Save As)
