Breast Tomosynthesis Improves Screening in Community Settings
Released: April 11, 2023
At A Glance
- Researchers have found that digital breast tomosynthesis (DBT) has improved breast cancer screening performance in community settings.
- A total of 896,101 women and 2,301,766 screening exams were included in the retrospective study.
- Radiologist interpretive performance improved with DBT compared to digital mammography.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Researchers have found that digital breast tomosynthesis (DBT) has improved breast cancer screening performance in community practice and identifies more invasive cancers, compared to digital mammography. In addition, radiologists’ interpretive performance improved with DBT. The results of the study were published today in Radiology, a journal of the Radiological Society of North America (RSNA).
“Our study demonstrated that more radiologists in U.S. community practice are meeting recommended performance standards with digital breast tomosynthesis than they did with digital mammography,” said lead author Christoph I. Lee, M.D., professor of radiology at the University of Washington (UW) School of Medicine in Seattle, director of the Northwest Screening and Cancer Outcomes Research Enterprise at UW, and adjunct professor of health systems and population health at the UW School of Public Health. “This is good news for women and breast cancer screening, as digital breast tomosynthesis has quickly become the most popular breast cancer screening modality in the U.S.”
After gaining U.S. Food and Drug Administration (FDA) approval in 2011, DBT was rapidly adopted in the U.S. As of September 2022, 84% of all mammography screening facilities in the U.S. had DBT units.
Breast cancer mortality reduction from routine screening is contingent upon radiologists’ interpretive performance. Since the Mammography Quality Standards Act was enacted in 1992, screening facilities and interpreting radiologists have been required to meet minimum quality standards. Beginning in 2006, the Breast Cancer Surveillance Consortium (BCSC) has published screening performance benchmarks. The BCSC is a collaborative network of breast imaging registries conducting research to assess and improve the delivery and quality of breast cancer screening and related patient outcomes.
To establish performance benchmarks for DBT screening and evaluate performance trends over time in U.S. community practices, the research team collected DBT screening exams from five BCSC registries between 2011 and 2018.
Performance measures included abnormal interpretation rate, cancer detection rate, sensitivity, specificity and false-negative rate.
Compared to BCSC digital mammography screening exams from the same time period and previously published BCSC and National Mammography Database performance benchmarks, all performance measures were higher for DBT except sensitivity and false-negative rate, which were similar to concurrent and prior digital mammography performance measures.
“Radiologists appear to perform better with digital breast tomosynthesis and have higher accuracy on screening 3D mammograms than 2D mammograms across U.S. practices,” Dr. Lee noted. “As this becomes the mainstay screening modality, we hope to see improved screening outcomes for women.”
A total of 896,101 women undergoing 2,301,766 screening exams—458,175 DBT and 1,843,591 2D digital mammography—were included in the retrospective study. The abnormal interpretation rate was 8.3%, cancer detection rate was 5.8 per 1,000 exams, sensitivity was 87.4%, and specificity was 92.2%.
With DBT, 97.6%, 91.8%, 75.0%, and 74.0% of assessed radiologists achieved the recommended acceptable performance ranges for cancer detection rate, sensitivity, abnormal interpretation rate and specificity, respectively.
Dr. Lee notes that these benchmarks are also very important for the emerging field of artificial intelligence.
“Any new AI tools aimed at improving mammography accuracy will have to revise their own performance goals based on the improved radiologist performance with DBT,” he said.
“National Performance Benchmarks for Screening Digital Breast Tomosynthesis: Update from the Breast Cancer Surveillance Consortium.” Collaborating with Dr. Lee were Linn Abraham, M.S., Diana L. Miglioretti, Ph.D., Tracy Onega, Ph.D., Karla Kerlikowske, M.D., Janie M. Lee, M.D., Brian L. Sprague, Ph.D., Anna N. A. Tosteson, Sc.D., Garth Rauscher, Ph.D., Erin J. A. Bowles, M.P.H., Roberta M. diFlorio-Alexander, M.D., and Louise M. Henderson, Ph.D., for the Breast Cancer Surveillance Consortium.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology’s legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research, and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
Video (MP4):

Video 1. Christoph I. Lee, M.D., discusses his research on national performance benchmarks for screening digital breast tomosynthesis.
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
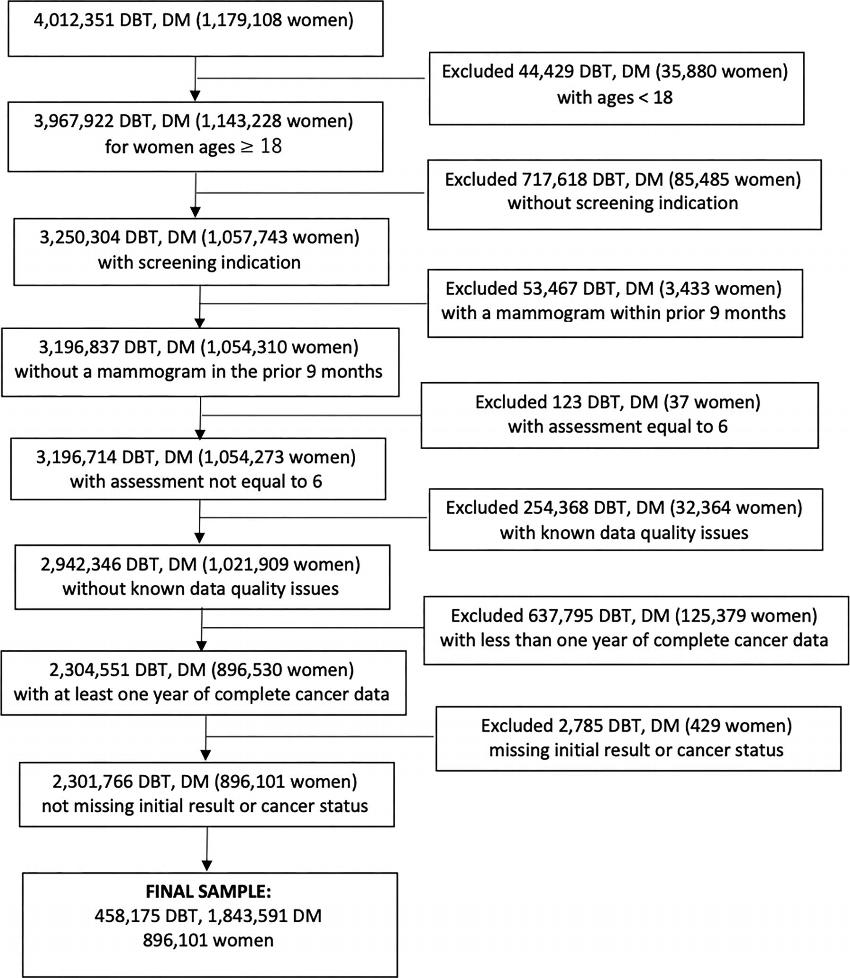
Figure 1. Flow diagram shows selection criteria for study patients. DBT = digital breast tomosynthesis, DM = digital mammogram.
High-res (TIF) version
(Right-click and Save As)
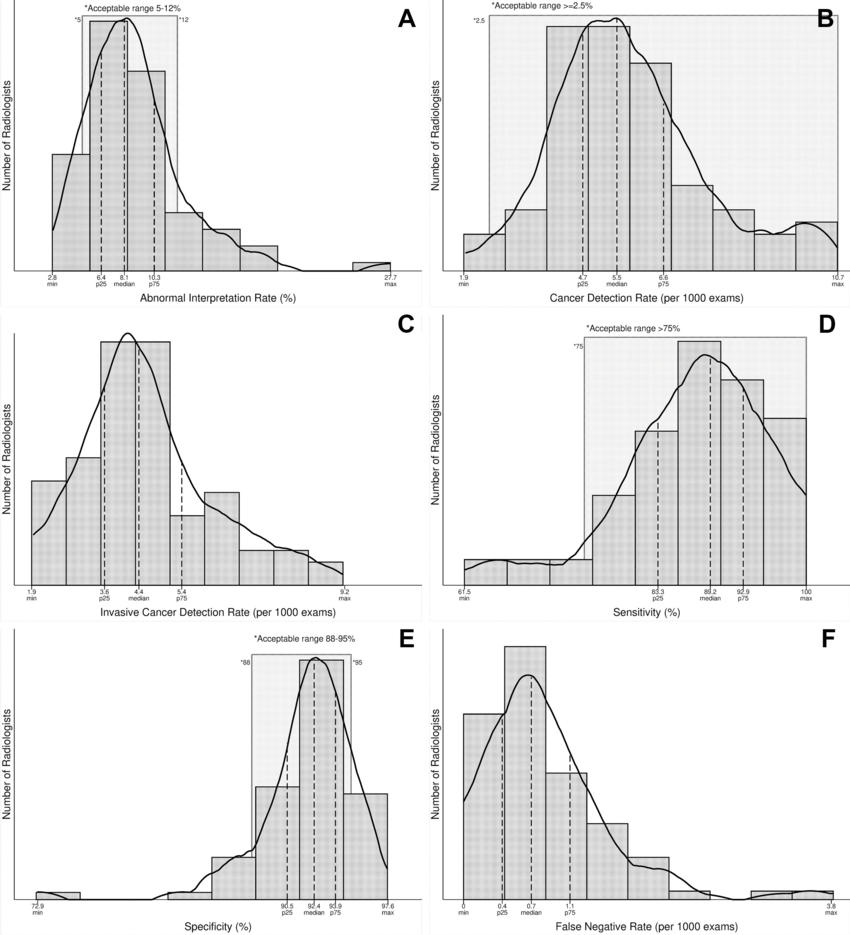
Figure 2. Radiologist digital breast tomosynthesis (DBT) screening performance and acceptable ranges. Histograms show the distribution of DBT screening performance benchmarks by radiologists including (A) abnormal interpretation rate (AIR), (B) cancer detection rate (CDR) (per 1000 examinations), (C) invasive CDR (per 1000 examinations), (D) sensitivity, (E) specificity, and (F) false-negative rate (per 1000 examinations). Lightly shaded region indicates radiologists within acceptable ranges established previously by expert opinion (if applicable). With DBT, 97.6%, 91.8%, 75.0%, and 74.0% of radiologists achieved the recommended acceptable performance ranges for CDR, sensitivity, AIR, and specificity, respectively. Only radiologists with at least 1000 DBT screening interpretations during the study period were included (n = 84). Sensitivity and specificity were restricted to radiologists with at least 10 DBT screening-detected cancers (n = 73). Max = maximum, min = minimum, p25 = 25th percentile, p75 = 75th percentile.
High-res (TIF) version
(Right-click and Save As)
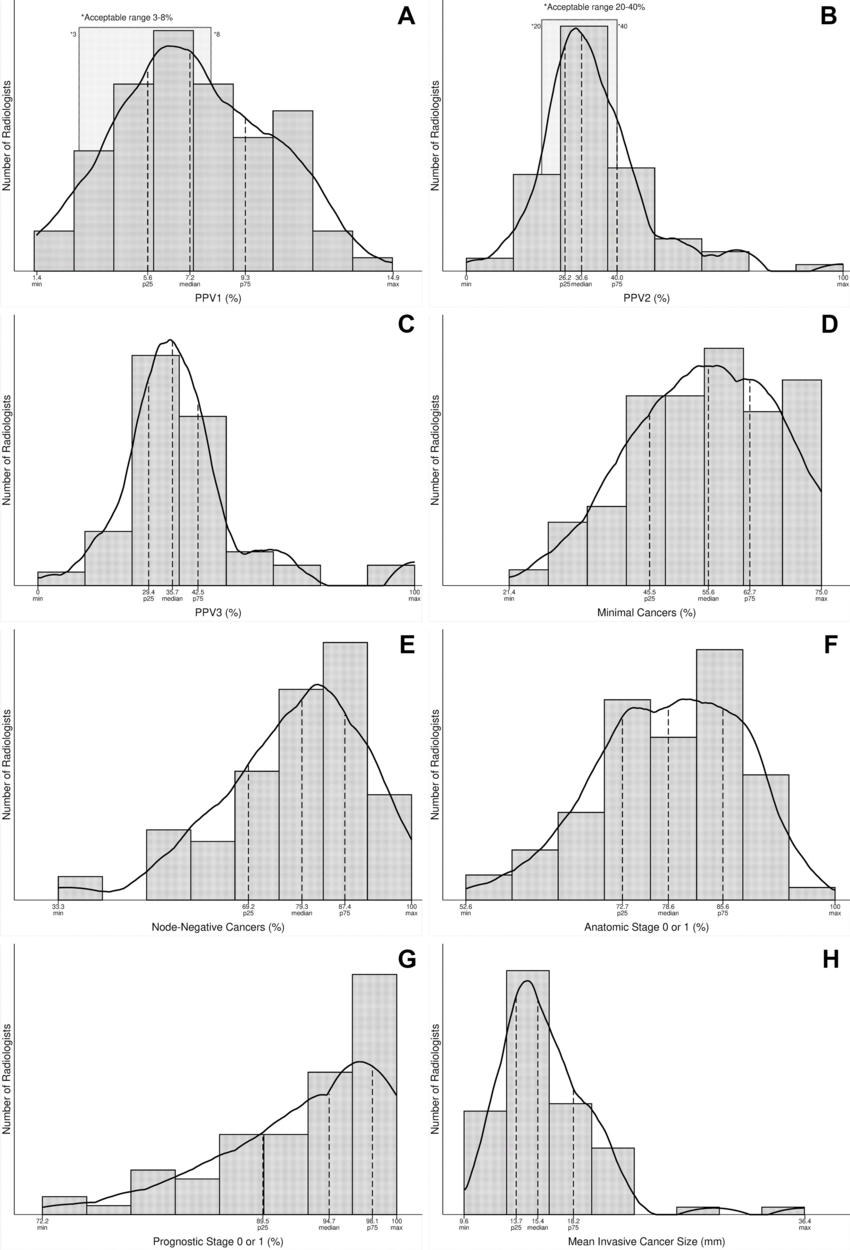
Figure 3. Additional radiologist digital breast tomosynthesis (DBT) screening performance measures and acceptable ranges. Histograms show the distribution of DBT screening performance benchmarks by radiologists including (A) PPV1, (B) PPV2, (C) PPV3, (D) minimal cancers, (E) node-negative cancers, (F) anatomic stage 0 or 1, (G) prognostic stage 0 or 1, and (H) mean invasive cancer size. Lightly shaded region indicates radiologists within acceptable ranges established previously by expert opinion (if applicable). With DBT, 53.6% and 63.5% of radiologists assessed achieved the recommended acceptable performance ranges for PPV1 and PPV2, respectively. Only radiologists with at least 1000 DBT screening interpretations during the study period were included (n = 84). The percentage of minimal cancers and the percentage of node-negative cancers were restricted to radiologists with at least 10 DBT screening-detected cancers (n = 73). BI-RADS = Breast Imaging Reporting and Data System, Max = maximum, min = minimum, p25 = 25th percentile, p75 = 75th percentile, PPV1 = examinations with abnormal interpretation (BI-RADS 0, 3, 4, or 5), PPV2 = recommendation for tissue diagnosis (BI-RADS 4 or 5), PPV3 = PPV of biopsy performed.
High-res (TIF) version
(Right-click and Save As)