Pulsed Radiofrequency with Steroid Injection Brings Sciatica Relief
Released: March 28, 2023
At A Glance
- Pulsed radiofrequency, combined with epidural steroid injection treatment, led to superior, longer-lasting pain reduction in patients with sciatica.
- Pulsed radiofrequency is a minimally invasive procedure in which pulses of energy from a probe are applied directly to nerve roots near the spine.
- The combined procedure takes only 10 minutes and is performed without general anesthesia.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Researchers found that a minimally invasive procedure combined with epidural steroid injection treatment led to superior pain reduction and disability improvement over one year in patients with sciatica. The results of the study were published in Radiology, a journal of the Radiological Society of North America (RSNA). The combined treatment performed better than steroid injections alone.
Sciatica is pain that originates along the sciatic nerve, which extends from the back of the pelvis down the back of the thigh. The sciatic nerve is the largest nerve in the body. Treatments to relieve pain include nonsteroidal anti-inflammatory medications, applying heat or cold, and exercising to help minimize inflammation. When the pain is caused by a lumbar disc herniation, surgery is often the treatment option for pain relief.
“The goal of nonoperative care is to provide the most effective means of symptom resolution, while still avoiding the need for a surgical procedure,” said the study’s lead author, Alessandro Napoli, M.D., Ph.D., associate professor of radiology and interventional radiology at Policlinico Umberto I – Sapienza University of Rome, in Italy. “However, in many cases conventional approaches are ineffective.”
Minimally invasive interventional therapy has become increasingly popular in patients with sciatica who have become resistant to conservative treatments. Among the available options, transforaminal epidural steroid injection (TFESI) is the only interventional procedure recommended in clinical guidelines. However, the duration of benefit is usually short, and additional treatments are often necessary.
Another treatment that researchers have studied for sciatica pain relief is pulsed radiofrequency—a minimally invasive procedure in which pulses of energy from a probe are applied directly to nerve roots near the spine.
For the multicenter randomized trial, researchers wanted to determine the difference in effectiveness between pulsed radiofrequency combined with TFESI versus the steroid injection alone for sciatica pain lasting 12 weeks or longer and not responsive to conservative treatment in patients with due to lumbar disc herniation.
A total of 351 participants (223 men) with sciatica were randomly assigned to receive a single CT-guided pulsed radiofrequency treatment combined with TFESI (174 patients) or TFESI alone (177 patients). Participants were recruited at two tertiary university hospitals and one spine clinic. All procedures were carried out in an outpatient clinic, took only 10 minutes and were performed without general anesthesia.
At four, 12, and 52 weeks there was greater leg pain reduction and greater disability improvement in participants who received pulsed radiofrequency combined with TFESI compared to the participants who only received the steroid injection.
“The results of our trial demonstrate that a combined treatment of pulsed radiofrequency and TFESI leads to better outcomes at one year following a single 10-minute procedure,” Dr. Napoli said.
“CT-guided Pulsed Radiofrequency Combined with Steroid Injection for Sciatica from Herniated Disc: A Randomized Trial.” Collaborating with Dr. Napoli were Giulia Alfieri, M.D., Alessandro De Maio, M.D., Emanuela Panella, R.N., Roberto Scipione, M.D., Giancarlo Facchini, M.D., Ugo Albisinni, M.D., Paolo Spinnato, M.D., Pier Giorgio Nardis, M.D., Roberto Tramutoli, M.D., Jacopo Lenzi, M.D., Pejman Ghanouni, M.D., Ph.D., Alberto Bazzocchi, M.D., Ph.D., Stefano Perotti, M.D., Andrew J. Schoenfeld, M.D., M.Sc., and Carlo Catalano, M.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology’s legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on interventional radiology procedures, visit RadiologyInfo.org.
Images (JPG, TIF):
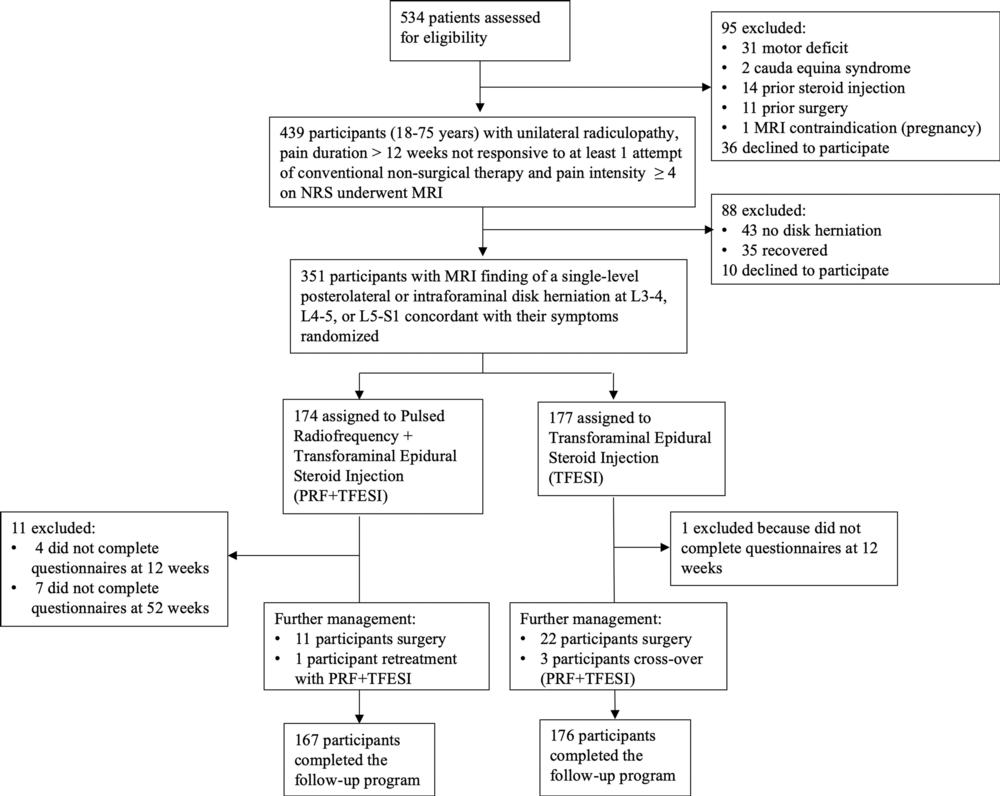
Figure 1. Flowchart shows enrollment and randomization criteria. NRS = numeric rating scale.
High-res (TIF) version
(Right-click and Save As)
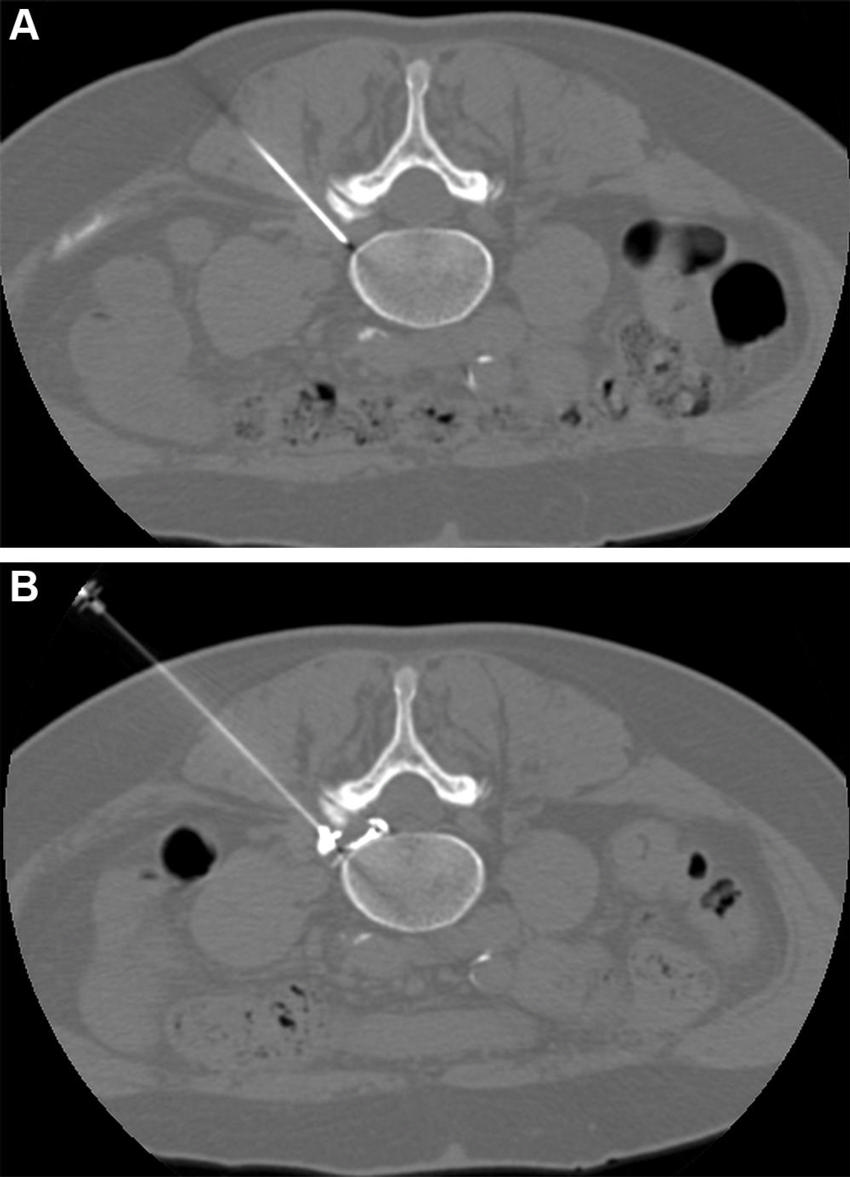
Figure 2. CT-guided pulsed radiofrequency (PRF) with transforaminal epidural steroid injection. A 62-year-old woman underwent PRF followed by transforaminal epidural steroid injection for sciatica due to left contained intraforaminal disk herniation at the L4-5 level. (A) A 22-gauge needle electrode with a 10-mm active tip was introduced and advanced using one 3-mm oblique axial unenhanced CT scan, which revealed that the needle tip was proximate to the target dorsal root ganglion with the lateral foraminal portal of entry. (B) Sensitive stimulation (50 Hz) PRF current with a threshold of no more than 0.2 V was used to confirm proper positioning by evoking tingling or electric pain in the dermatome that had to match the target dorsal root ganglion. Therapeutic PRF was then performed in one 10-minute session with E-dose functionality, maintaining temperature below the threshold for neural damage (42°C) and a constant voltage (45 V). Immediately after PRF administration, epidural spread of 0.3 mL of contrast material was confirmed using intermittent intraprocedural CT fluoroscopic imaging with no intravascular contrast material flow demonstration. A combination of steroid and anesthetic (1 mL lidocaine [ 20 mg/mL] and 2 mL dexamethasone [10 mg/mL]) was then injected without altering needle position to conclude the procedure.
High-res (TIF) version
(Right-click and Save As)
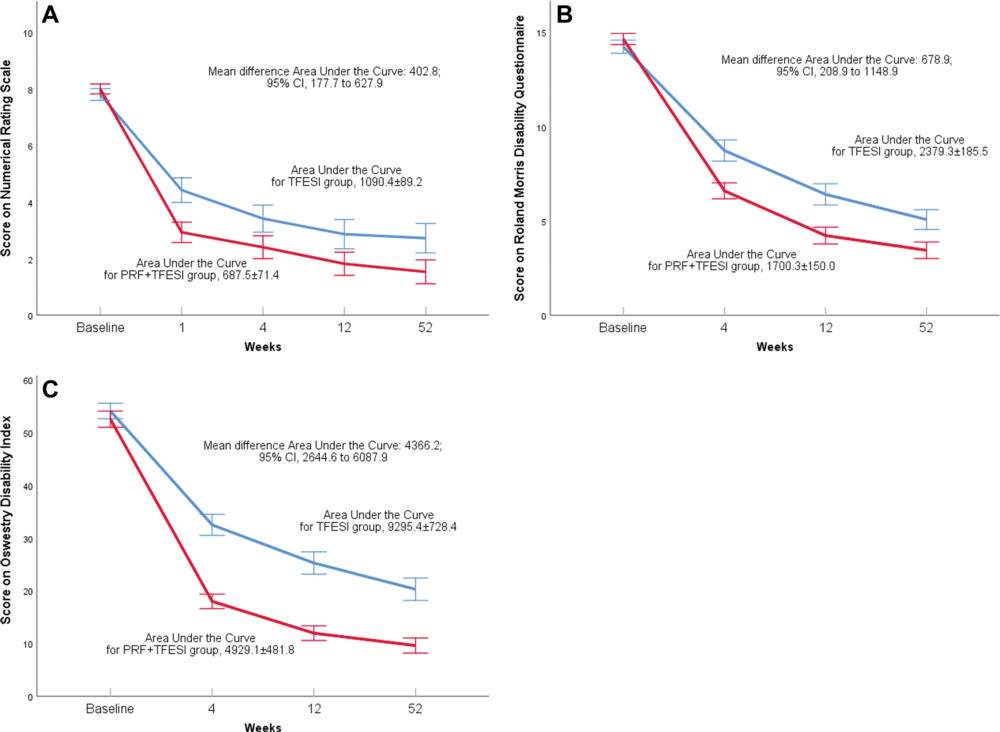
Figure 3. (A) Numeric rating scale (NRS) for leg pain, (B) Roland-Morris Disability Questionnaire (RMDQ), and (C) Oswestry Disability Index (ODI). Panels show curves of means with 95% CIs for the 52-week observation period. Follow-up scores are denoted at 1 week (for NRS only) and at 4, 12, and 52 weeks. Values on the y-axis are expressed as different outcome measures in each panel. Blue indicates the pulsed radiofrequency (PRF) and transforaminal epidural steroid injection (TFESI) treatment group, while red indicates the TFESI group. Mean and mean differences are indicated over the panels for the area under the curve analysis with the respective 95% CIs, as analyzed with the Student t test. Results show statistical significance in favor of the combined treatment protocol at all time points for the NRS and RMDQ and ODI scales.
High-res (TIF) version
(Right-click and Save As)
