Huge Study Finds Tomosynthesis Better at Breast Cancer Detection
Released: March 14, 2023
At A Glance
- Digital breast tomosynthesis showed improved breast cancer screening outcomes in a study including more than 1 million women and over 2 million screening exams.
- The study group consisted of women aged 40 to 79 who were screened with DBT or digital mammography between January 2014 and December 2020.
- DBT had better cancer detection and fewer false positive results.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — In a study of over a million women, digital breast tomosynthesis (DBT) showed improved breast cancer screening outcomes over screening with standard digital mammography alone. The results of the study were published in Radiology, a journal of the Radiological Society of North America (RSNA).
Breast cancer is the most common cancer among women in the United States. While breast cancer mortality has been on the decline since the late 1980s due to improvements in early detection and treatment, it still remains the leading cause of cancer death among women.
The five-year relative survival rate of breast cancer when it is detected early in its localized stage is 99%, according to the American Cancer Society. Regular screening is the most reliable method for the early detection of breast cancer.
Screening with two-dimensional (2D) digital mammography alone is still the standard of care at many sites, but it has its limitations due to its inability to detect some cancers. There is a growing amount of evidence that DBT, a more advanced technology, has a higher breast cancer detection rate due to its ability to capture multiple X-ray images of the breast from different angles rather than the typical single image obtained with a standard 2D mammogram. DBT is especially beneficial for women with denser breast tissue.
“The purpose of our study was to evaluate screening outcomes among a large cohort of women in the United States who were screened with either 2D digital mammography alone or with DBT,” said study co-author Emily F. Conant, M.D., FSBI, professor of radiology and chief in the Division of Breast Imaging at the Hospital at the University of Pennsylvania in Philadelphia.
For this retrospective cohort study, Dr. Conant and colleagues compiled data from five large health care systems across the United States. The study group consisted of over 1 million women aged 40 to 79 who were screened with either DBT or 2D digital mammography alone between January 2014 and December 2020. The screening outcomes such as cancer detection and false positive rates were compared across the two screening groups.
“This study was extremely large with most women having at least 2 screens resulting in over 2 million screening exams across five large and diverse health care systems,” Dr. Conant said.
Compared to 2D digital mammography alone, DBT was associated with important improvements in screening outcomes. The cancer detection rate for patients screened with DBT was higher at 5.3 per 1,000 screened, compared to 4.5 per 1,000 screened with 2D digital mammography only. DBT also had a lower rate of false positives and recalls from screening.
“We showed that the most important mammographic screening outcomes, increased cancer detection combined with fewer false positives, were significantly improved when women were screened with digital breast tomosynthesis compared to 2D digital mammography alone,” Dr. Conant said. “Therefore, women should seek out sites that routinely offer breast cancer screening with DBT.”
“Mammographic Screening in Routine Practice: Multisite Study of Digital Breast Tomosynthesis and Digital Mammography Screenings.” Collaborating with Dr. Conant were Melinda M. Talley, M.D., Chirag R. Parghi, M.D., M.B.A., Bryant C. Sheh, M.D., Su-Ying Liang, Ph.D., Scott Pohlman, M.S., Amey Rane, M.S., B.Pharm., Yoojin Jung, Ph.D., Lauren A. S. Stevens, M.P.H., Jessica K. Paulus, Sc.D., and Nila Alsheik, M.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology’s legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
Images (JPG, TIF):
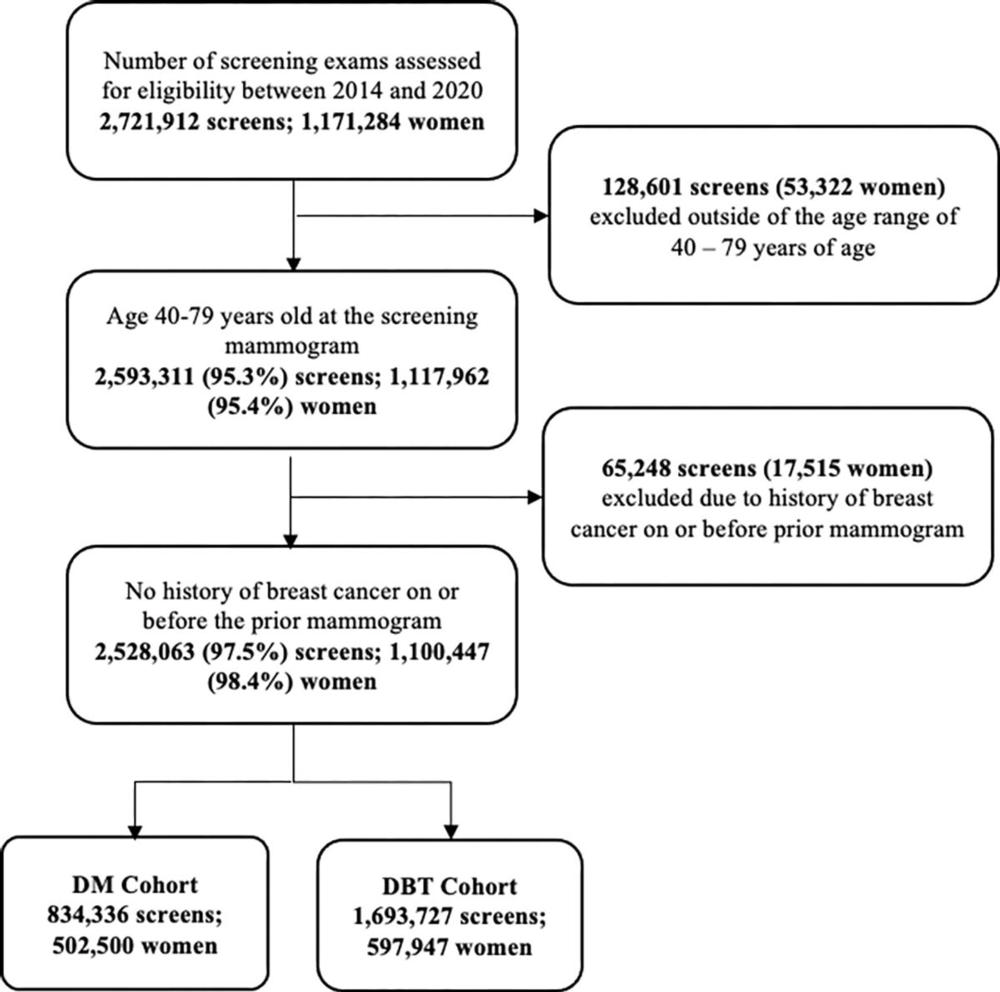
Figure 1. Study cohort creation. Flowchart outlines each inclusion and exclusion criterion required to be met for inclusion in the analysis. Women aged between 40–79 years at the time screening and without a history of breast cancer on or before the prior mammogram were eligible for inclusion.
High-res (TIF) version
(Right-click and Save As)
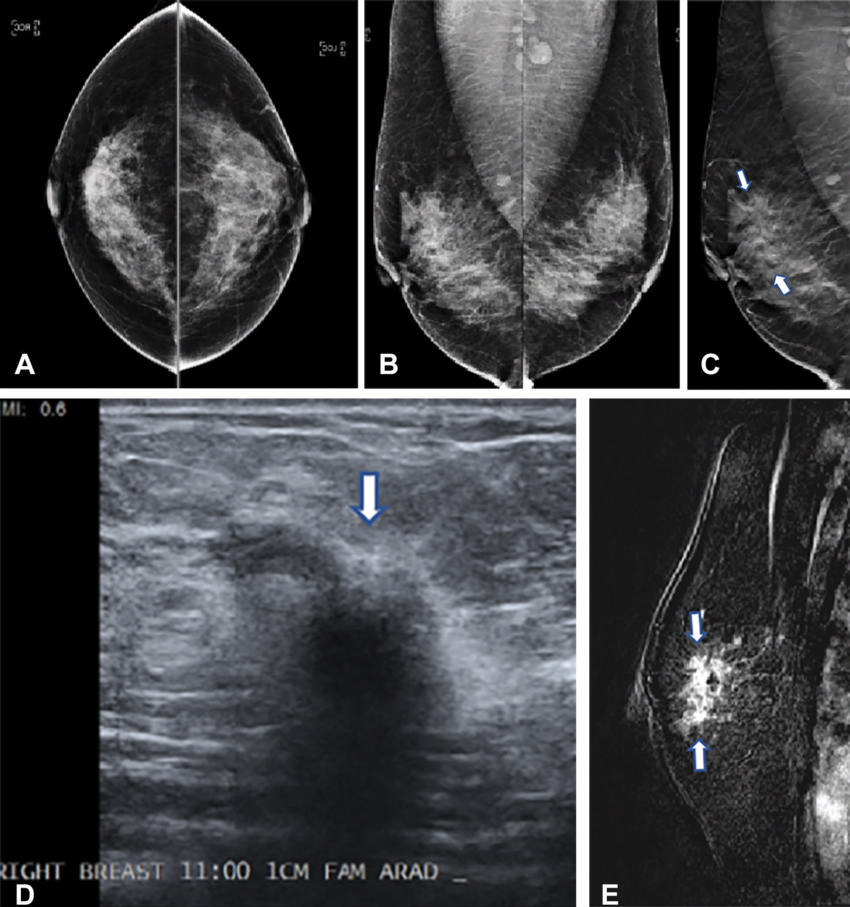
Figure 2. Images in a 42-year-old woman who presented for routine screening. (A) Two-dimensional craniocaudal digital mammogram and (B) two-dimensional mediolateral digital mammogram show heterogeneously dense breast tissue with no abnormality. (C) Mediolateral digital breast tomosynthesis image shows subtle architectural distortion (arrows) extending superiorly from the nipple level. (D) Target US image of the right breast shows a highly suspicious, hypoechoic, irregular mass (arrow). US-guided core biopsy yielded invasive ductal carcinoma with extensive ductal carcinoma in situ (T2N0M0; estrogen receptor–positive, progesterone receptor–positive, and human epidermal growth factor receptor 2–negative). (E) Right-breast MRI scan acquired to evaluate the extent of disease shows a clip artifact in the superior aspect of the irregular enhancing mass (arrows). No other suspicious lesions were seen.
High-res (TIF) version
(Right-click and Save As)
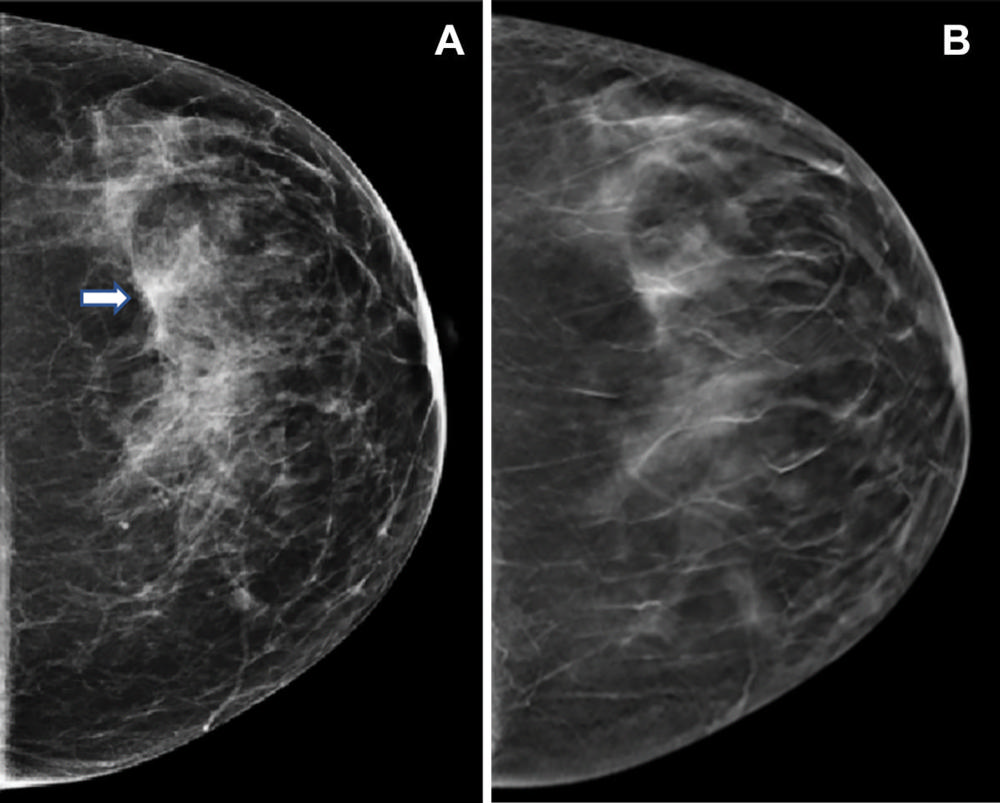
Figure 3. Images in a 47-year-old woman who presented for routine screening. (A) Craniocaudal digital mammogram shows scattered fibroglandular densities. On the left digital mammographic craniocaudal view laterally, an asymmetry (arrow) is present. (B) Left craniocaudal digital breast tomosynthesis image shows no suspicious lesion but rather a superimposition of normal fibroglandular and ligamentous structures.
High-res (TIF) version
(Right-click and Save As)
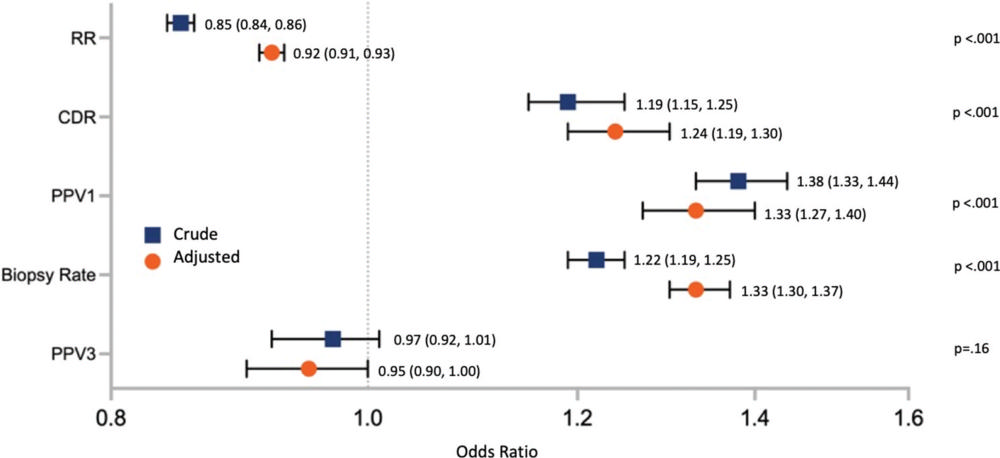
Figure 4. Crude and adjusted associations between screening modality and breast cancer screening outcomes: comparison of digital breast tomosynthesis (DBT) with digital mammography (DM). Forest plot shows the crude and adjusted odds ratios (ORs), with 95% CIs in parentheses and vertical bars showing the range of 95% CIs, for the primary outcomes of recall rate (RR), cancer detection rate (CDR), positive predictive value of recall (PPV1), biopsy rate, and positive predictive value of biopsy (PPV3), comparing DBT with DM. ORs were adjusted for age category (40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, and 75–79 years), breast density, health system, and index year of examination.
High-res (TIF) version
(Right-click and Save As)
