Chest CT Shows Lung Abnormalities Two Years after COVID
Released: February 14, 2023
At A Glance
- Chest CT revealed persistent lung abnormalities in patients two years after being hospitalized with COVID-19.
- CT scans and pulmonary function tests were obtained at six months, 12 months and two years after symptom onset.
- At two-year follow-up, 39% of participants had persistent lung abnormalities, which were associated with respiratory symptoms and decreased lung
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. (February 14, 2023) — Chest CT revealed persistent lung abnormalities in patients two years after COVID-19, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA). This is the first research paper with two-year follow-up data on COVID-19 lung effects.
Globally, more than 600 million people have recovered from COVID-19, but concerns remain that some organs, especially the lungs, may suffer long-term damage after infection.
Qing Ye, M.D., and Heshui Shi, M.D., Ph.D., from Tongji Medical College of Huazhong University of Science and Technology in Wuhan, China, and colleagues set out to assess residual lung abnormalities in patients up to two years post-COVID-19 pneumonia. They also looked at the correlation between residual lung abnormalities and changes in lung function.
In this prospective study, 144 patients (79 men and 65 women, median age 60) discharged from the hospital after SARSCoV-2 infection between January 15 and March 10, 2020, were included. Three serial chest CT scans and pulmonary function tests were obtained at six months, 12 months and two years after symptom onset.
Residual lung abnormalities after discharge from the hospital included fibrosis (scarring), thickening, honeycombing, cystic changes, dilation of the bronchi, and more.
Over two years, the incidence of lung abnormalities gradually decreased. At six months, 54% of patients showed lung abnormalities. On two-year follow-up CT scans, 39% (56/144) of the patients had lung abnormalities, including 23% (33/144) with fibrotic lung abnormalities and 16% (23/144) with non-fibrotic lung abnormalities.
"In particular, the proportion of fibrotic interstitial lung abnormalities, an important precursor to idiopathic pulmonary fibrosis, remained stable throughout follow-up," the authors said. "Therefore, the fibrotic abnormalities observed in our study might represent a stable, irreversible pulmonary condition, such as lung fibrosis, after COVID-19."
The remaining 88 cases (61%) showed no abnormalities.
Patients with lung abnormalities on CT were more likely to have respiratory symptoms and abnormal lung function. The proportion of individuals with respiratory symptoms decreased from 30% at six months to 22% at two years.
At two-year follow-up, the most common respiratory symptom was exertional dyspnea or shortness of breath (14% [20/144]), while mild and moderate pulmonary diffusion—which refers to how well the air sacs in the lungs are delivering oxygen to and removing carbon dioxide from the blood in the tiny blood vessels that surround them—were observed in 29% (38/129) of patients. Pulmonary diffusion was regarded as abnormal when diffusing capacity of the lung for carbon monoxide was less than 75% of the predicted value. The researchers suggest that persisting residual symptoms and abnormal lung function could be related to the patient's ongoing lung damage.
"Long-term and functional consequences of chest CT findings post-COVID-19 are largely unknown," the authors said. "Our prospective study found that 39% of participants had persistent interstitial lung abnormalities at two-year follow-up, which were associated with respiratory symptoms and decreased diffusion function."
The authors advise that patients with residual lung abnormalities or respiratory symptoms after COVID-19 should be followed up to detect and manage pulmonary changes and functional impairment.
"Longitudinal Assessment of Chest CT Findings and Pulmonary Function in Patients after COVID-19." Collaborating with Drs. Ye and Shi were Xiaoyu Han, M.D., Ph.D., Lu Chen, M.D., Yanqing Fan, M.D., Osamah Alwalid, M.D., Xi Jia, M.D., Yuting Zheng, M.D., Jie Liu, M.D., Ph.D., Yumin Li, M.D., Ph.D., Yukun Cao, M.D., Jin Gu, M.D., Ph.D., Jia Liu, M.D., Ph.D., and Chuansheng Zheng, M.D., Ph.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology's legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research, and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on chest CT, visit RadiologyInfo.org.
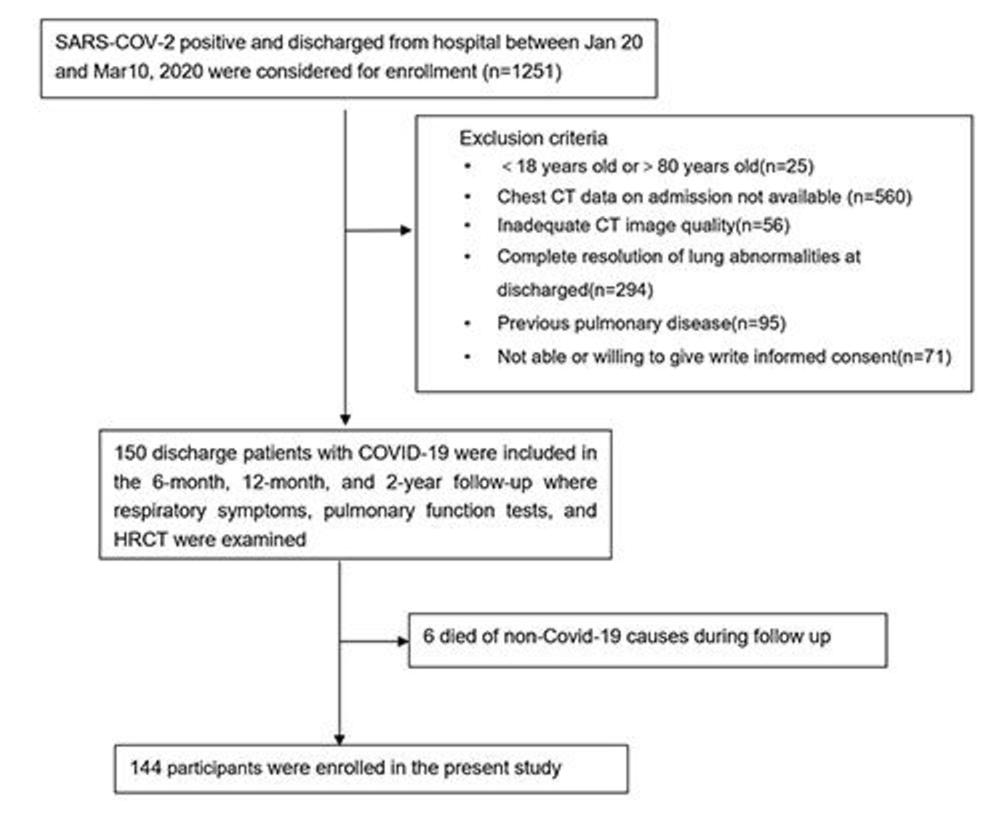
Figure 1. Participant flow diagram. HRCT = high-resolution CT, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
High-res (TIF) version
(Right-click and Save As)
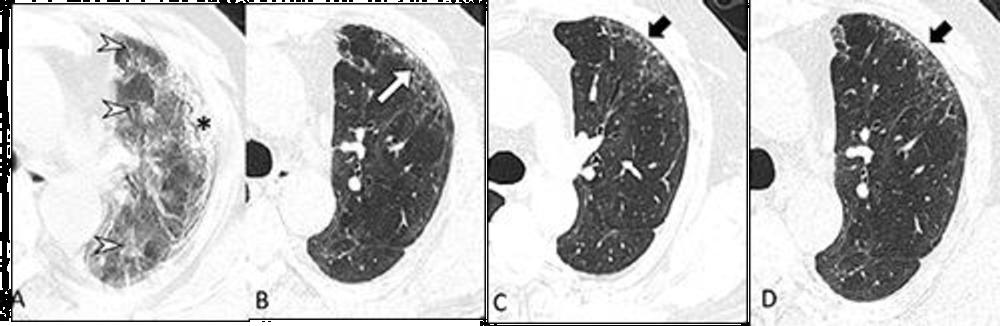
Figure 2. Serial transverse CT scans in a 65-year-old man with severe COVID-19. (A) CT scan obtained on day 23 after onset of symptoms showed diffuse ground-glass opacities (arrow heads) combined with subpleural consolidation (*) at the left upper lobe. (B) Image obtained at 6-month follow up showed subpleural primarily ground-glass opacity in the anterior upper lobe of the left lung along with minor bronchiectasis (white arrow). (C, D) Images obtained at 12-month and 2-year follow up showed presence of subtle, subpleural honeycombing at the same area (black arrows). This patient complained of ongoing exertional dyspnea and showed a mild diffusing capacity of the lung for carbon monoxide (74%) at 2-year follow up.
High-res (TIF) version
(Right-click and Save As)
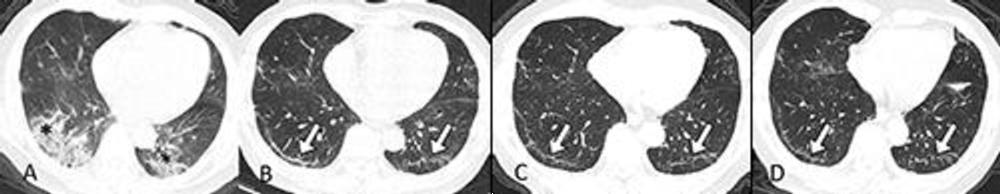
Figure 3. Serial transverse CT scans in a 67-year-old man with moderate COVID-19. (A) CT scan obtained on day 10 after onset of symptoms showed bilateral mixed pattern of ground-glass opacities and consolidation (*) in both lower and upper lobes. (B, C, D) Images obtained at 6-month, 12-month and 2-year follow up, respectively, showed persisting subpleural, bilateral linear, and curvilinear bands (white arrows) in both the lower and upper lobe. This patient did not report residual respiratory symptoms and had normal diffusing capacity of the lung for carbon monoxide (85%) at 2-year follow up.
High-res (TIF) version
(Right-click and Save As)
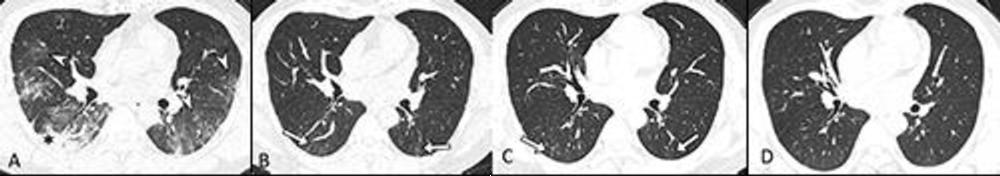
Figure 4. Serial transverse CT scans in a 39-year-old man with moderate COVID-19. (A) CT scan obtained on day 18 after onset of symptoms showed diffuse ground-glass opacities (GGOs, arrowhead) bilaterally combined with consolidation (*) in the right lower lobe. (B) Image obtained at 6-month follow up showed only subtle residual subpleural GGOs and linear opacities (arrows). (C) Image obtained at 12-month follow up showed further partial resorption of the residual GGOs and linear opacities (arrows). (D) Image obtained at 2-year follow up showed complete resolution of the abnormalities. This man was asymptomatic and had normal lung diffusion function at 2-year follow up.
High-res (TIF) version
(Right-click and Save As)
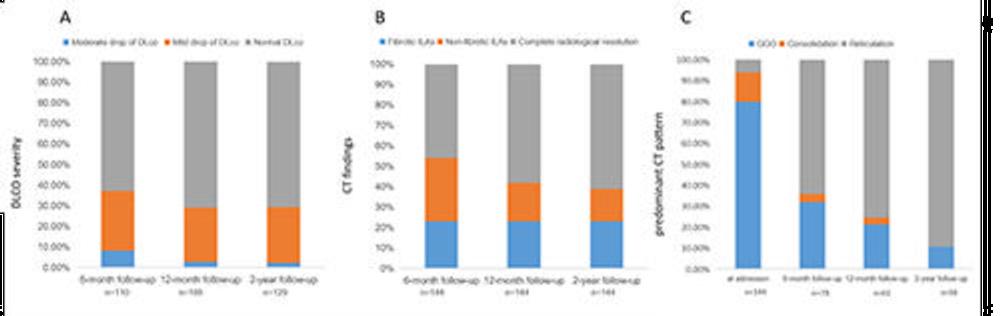
Figure 5. Stacked bar graph showing (A) proportion of participants with different diffusing capacity of the lung for carbon monoxide severity. (B) Proportion of participants with different CT findings in patients with residual lung abnormalities. (C) Proportion of participants with predominant CT pattern over time. n = the denominator at different time points.
High-res (TIF) version
(Right-click and Save As)

Figure 6. Serial transverse CT scans in a 49-year-old female with critical COVID-19. (A) CT scan obtained on day 11 after onset of symptoms showed extensive ground-glass opacities (GGOs) bilaterally with foci of consolidation (*). (B) Scan obtained at 6-month follow up showed focal subpleural reticular lesions in the anterior segment of right upper lobe with traction bronchiectasis (white arrows). Scans obtained at 12-month follow up (C) and 2-year follow up (D) showed slow resorption of the bilateral GGOs but stable abnormalities in the right upper lobe. This patient complained of cough, expectoration, and exertional dyspnea and had moderate diffusing capacity of the lung for carbon monoxide (62%) at 2-year follow up.
High-res (TIF) version
(Right-click and Save As)