Researchers Use Radiomics to Predict Heart Attacks
Released: February 14, 2023
At A Glance
- Radiomics allows researchers to extract measurable data from CT images that can reveal disease characteristics not visible in the images alone.
- Researchers developed a radiomics model that uses information from coronary CT angiography images to assess coronary plaque vulnerability.
- The rupture of vulnerable plaques causes most heart attacks.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — Researchers are using an approach called radiomics to predict future cardiac events like heart attacks, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA). Radiomics allows researchers to extract quantitative, or measurable, data from CT images that can reveal disease characteristics not visible in the images alone.
Coronary artery disease is linked with fatty deposits of plaque that build up inside the artery walls. Large, lipid-rich plaques are vulnerable to rupture. The rupture of these plaques causes most heart attacks. However, predicting which plaques will rupture is challenging.
Researchers in China developed a radiomics model that uses information from coronary CT angiography images to assess plaque vulnerability. They developed the model in 299 patients. They then studied the approach in 708 patients with suspected coronary artery disease.
The model enabled the detection of vulnerable plaques associated with an increased risk for major adverse cardiac events like heart attacks. A high radiomic signature was independently associated with these events over a median three-year follow-up.
"The results of this study are encouraging and exciting," said study co-lead author Long Jiang Zhang, M.D., Ph.D., from the Department of Radiology at Jinling Hospital, Medical School of Nanjing University in Nanjing, China. "Radiomics provided a more accurate approach to detect vulnerable plaques compared to conventional coronary CT angiography anatomical parameters."
The radiomic signature would be easy to add into clinical practice, Dr. Zhang said. In the clinic, it could assess potentially vulnerable plaques and help stratify high-risk patients.
"If the radiomics analysis is embedded into the routine CT angiography workstation, it can automatically identify vulnerable plaques for clinician review," Dr. Zhang said. "Thus, radiomics may significantly improve the accuracy and precision of high-risk plaque detection in routine clinical practice."
The researchers intend to build a radiomics model from different scanner types and vendors. They also are planning a larger, multicenter study of 10,000 patients.
"With the support of large observational studies and randomized controlled trials, the radiomics approach may help guide clinical decision-making and improve patient care in the future," Dr. Zhang said.
"A Coronary CT Angiography Radiomics Model to Identify Vulnerable Plaque and Predict Cardiovascular Events." Collaborating with Dr. Zhang were Qian Chen, M.D., Tao Pan, M.B.B.S., Yi Ning Wang, M.D., Ph.D., U. Joseph Schoepf, M.D., Samuel L. Bidwell, B.S., Hongyan Qiao, M.D., Yun Feng, M.D., Cheng Xu, M.D., Hui Xu, M.Sc., Guanghui Xie, M.B.B.S., Xiaofei Gao, M.D., Xin-Wei Tao, M.Sc., Mengjie Lu, Ph.D., Peng Peng Xu, M.D., Jian Zhong, M.B.B.S., Yongyue Wei, Ph.D., Xindao Yin, M.D., Ph.D., and Junjie Zhang, Ph.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology's legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research, and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on coronary CT angiography, visit RadiologyInfo.org.
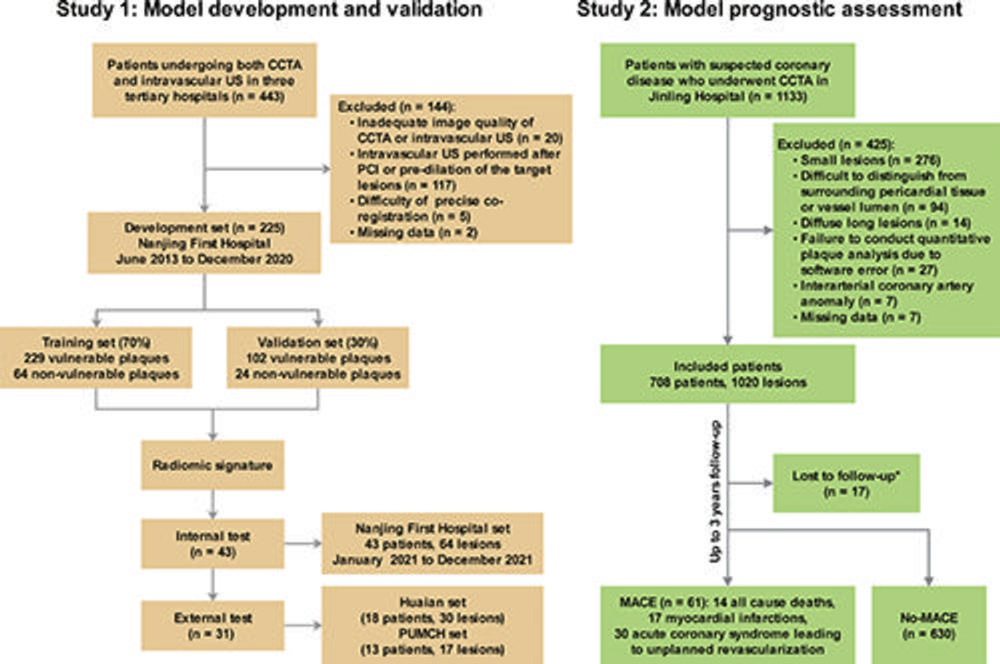
Figure 1. Study flowchart. Huaian set = Affiliated Huaian No. 1 People’s Hospital of Nanjing Medical University set; PUMCH set = Peking Union Medical College Hospital set. * = Lost to follow-up was defined as failure to contact participants at scheduled (90-day, 1-year and 3-year) telephone visits and no relevant medical records available after enrollment. CCTA = coronary CT angiography, MACE = major adverse cardiac events, PCI = percutaneous coronary intervention.
High-res (TIF) version
(Right-click and Save As)
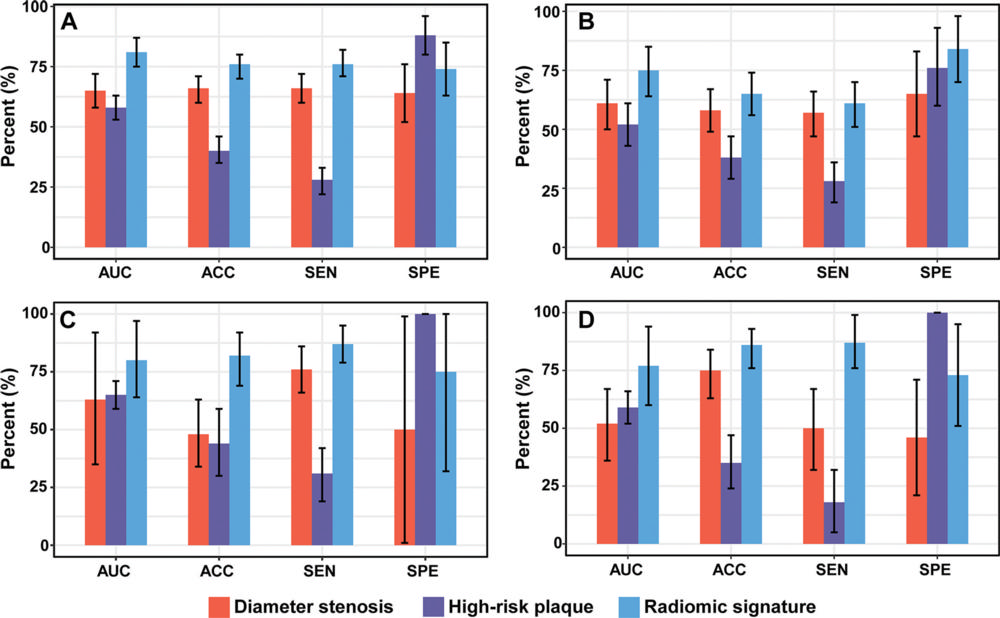
Figure 2. Bar charts show diagnostic performance for identifying vulnerable plaques defined with intravascular US in different data sets. Comparison of the area under the curve (AUC), accuracy (ACC), sensitivity (SEN), and specificity (SPE) among the radiomic signature, high-risk plaque (HRP) model, and diameter stenosis model in the (A) training set, (B) validation set, (C) internal test set, and (D) external test set. HRP was defined as a lesion with at least two features of adverse plaque characteristics at coronary CT angiography, including positive remodeling, low-attenuation plaque, spotty calcification, and napkin-ring sign. Error bars indicate 95% CIs.
High-res (TIF) version
(Right-click and Save As)
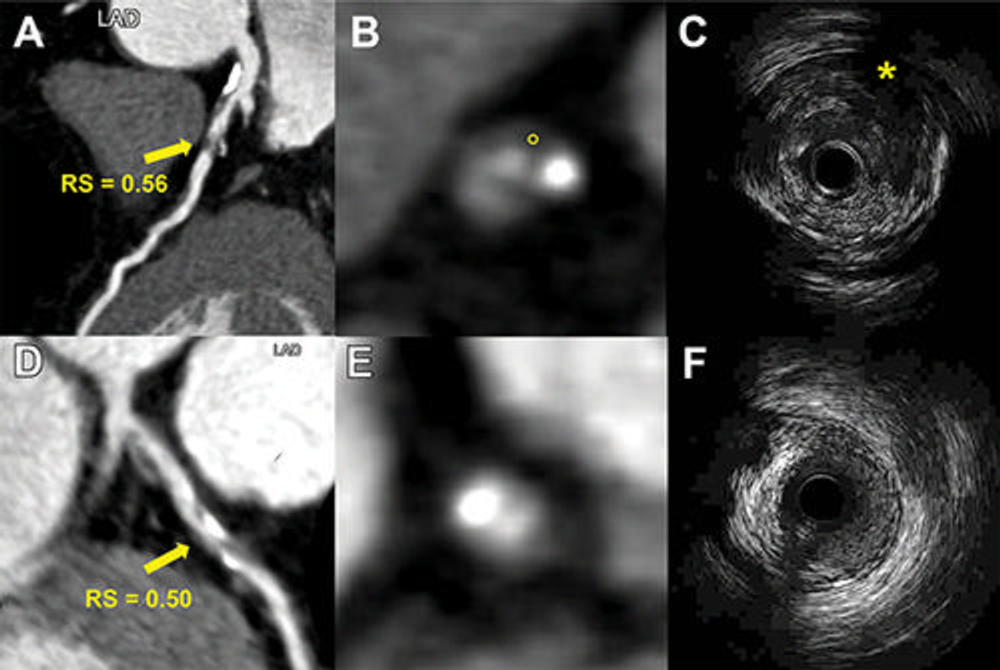
Figure 3. Representative images from two patients demonstrate the use of a radiomic signature (RS) to discriminate vulnerable plaques defined with intravascular US. (A–C) Images depict a vulnerable plaque with a high RS. (A) Image from coronary CT angiography (CCTA) shows a partially calcified plaque (arrow) with RS value of 0.56 in the proximal left anterior descending artery (LAD). (B) Corresponding axial CCTA image shows the plaque with low-attenuation area (circle, 25 HU). (C) Corresponding intravascular US scan confirms the plaque as an attenuated plaque (*). (D–F) Images show a nonvulnerable plaque with low RS. (D, E) CCTA images show a partially calcified plaque (arrow in D) with RS value of 0.50 in the proximal left anterior descending artery. (F) Corresponding intravascular US scan confirms the plaque as a partially calcified plaque without echo attenuation and echolucent zone. High versus low RS lesion was defined using an optimal cut-off value of 0.53 (range, 0.46–0.58).
High-res (TIF) version
(Right-click and Save As)
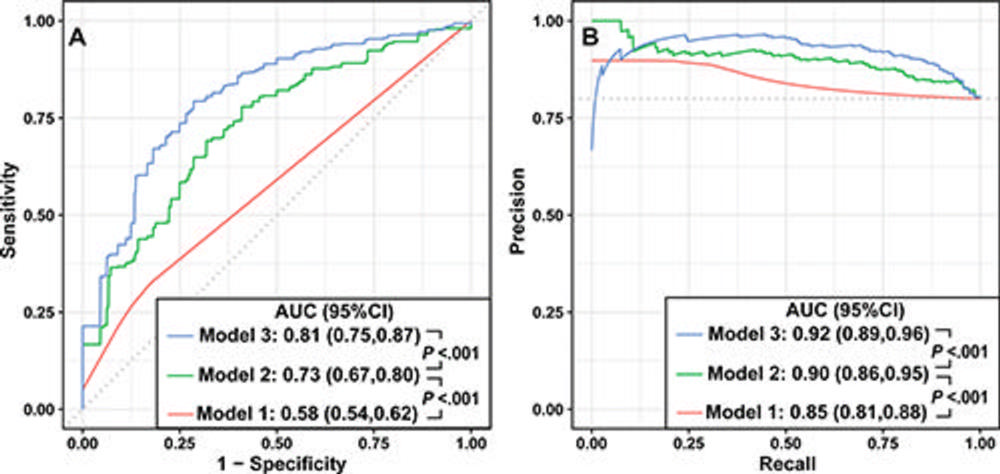
Figure 4. Incremental performance in the identification of vulnerable plaques defined with intravascular US. (A) Receiver operating characteristic curves show that the addition of a radiomic signature (RS) improves the conventional high-risk plaque (HRP) model and plaque volumes model in discriminating vulnerable plaques. (B) Precision-recall curves demonstrate a similar result as receiver operating characteristic curves. Model 1 = HRP; model 2 = HRP plus plaque volumes; model 3 = HRP plus plaque volumes plus RS. HRP was defined as a lesion with at least two features of adverse plaque characteristics at coronary CT angiography, including positive remodeling, low-attenuation plaque, spotty calcification, and napkin-ring sign. AUC = area under the curve.
High-res (TIF) version
(Right-click and Save As)
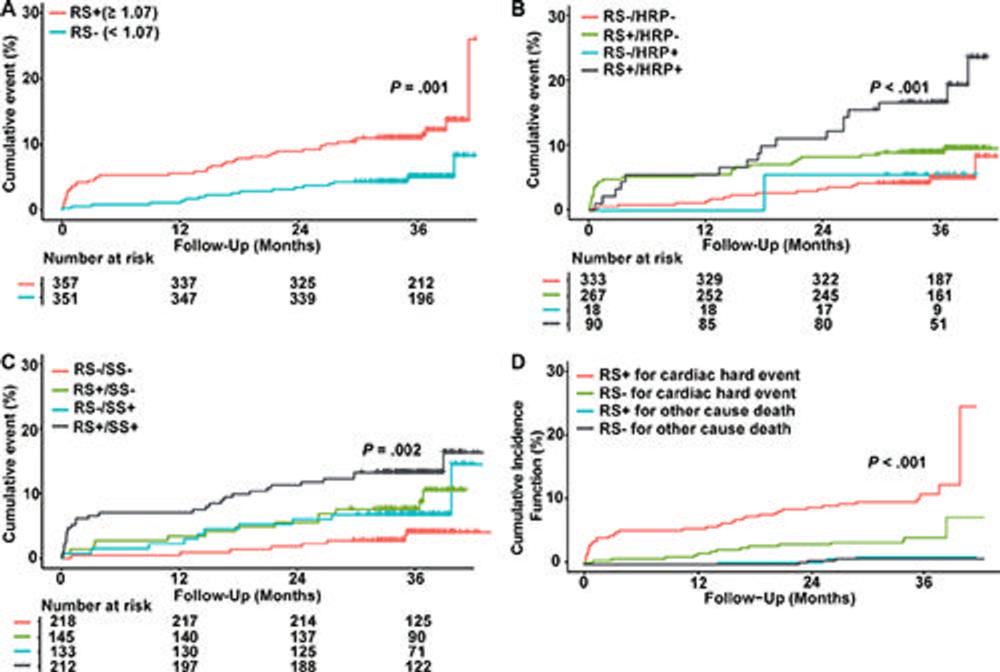
Figure 5. Kaplan-Meier curves show prognostic value of the radiomic signature (RS). (A) Curves for major adverse cardiac events (MACE) stratified according to RS. RS+ = RS positive, RS– = RS negative. (B, C) Estimates stratified by the presence (+) or absence (−) of (B) high RS and high-risk plaque (HRP) and (C) high RS and significant stenosis (SS). (D) Cumulative incidence function curves for a cardiac hard event and other cause death stratified by the RS. High versus low RS in patients was defined using an optimal cut-off value of 1.07 (range, 0.46–3.17). HRP was defined as a lesion with at least two features of adverse plaque characteristics, including positive remodeling, low-attenuation plaque, spotty calcification, and napkin-ring sign. Significant stenosis was defined as 50% diameter stenosis or greater in any coronary artery.
High-res (TIF) version
(Right-click and Save As)
