AI Improves Lung Nodule Detection on Chest X-rays
Released: February 07, 2023
At A Glance
- AI-based software significantly improved the detection of lung nodules on chest X-rays.
- The study included 10,476 individuals who had undergone chest X-rays at a health screening center.
- Analysis showed that the detection rate for actionable lung nodules on chest X-rays was higher when aided by AI.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — In a pioneering, randomized controlled study evaluating the effect of artificial intelligence (AI)-based software in real clinical practice, researchers found that AI significantly improved the detection of lung nodules on chest X-rays. The results of the study were published today in Radiology, a journal of the Radiological Society of North America (RSNA).
Lung nodules, which are abnormal growths that form on the lungs, are very common and typically form from previous lung infections. In rare instances, they can be a sign of lung cancer. One of the common screening methods used for identifying lung nodules is chest X-rays. AI can be a powerful tool to help identify lung nodules, especially when radiologists are experiencing a high volume of cases.
"Detecting lung nodules, a primary finding of lung cancer, is one of the crucial tasks in chest X-rays," said study co-author Jin Mo Goo, M.D., Ph.D., from the Department of Radiology at Seoul National University Hospital in Korea. "Many studies have suggested that AI-based computer-aided detection software can improve radiologists' performance, but it is not widely used."
To identify the actual effect that AI has in clinical practice, researchers included 10,476 patients with an average age of 59, who had undergone chest X-rays at a health screening center between June 2020 and December 2021.
"As our trial was conducted with a pragmatic approach, almost all enrolled participants were included, which is a real clinical setting," Dr. Goo said.
Patients completed a self-reported health questionnaire to identify baseline characteristics such as age, sex, smoking status and past history of lung cancer. Eleven percent of the patients were current or former smokers.
The patients were randomly divided evenly into two groups—AI or non-AI. The first group's X-rays were analyzed by radiologists aided by AI while the second group's X-rays were interpreted without the AI results.
Solid nodules with diameters either larger than 8 millimeters or subsolid nodules with a solid portion larger than 6 millimeters were identified as actionable, meaning that the nodule required follow-up according to lung cancer screening criteria.
Lung nodules were identified in 2% of the patients. Analysis showed that the detection rate for actionable lung nodules on chest X-rays was higher when aided by AI (0.59%) than without AI assistance (0.25%). There were no differences in the false-referral rates between the AI and non-AI interpreted groups.
While older age and a history of lung cancer or tuberculosis were associated with positive reports, these and the other health characteristics did not have an impact on the efficacy of the AI system. This suggests that AI may work consistently across different populations, even for those with diseased or postoperative lungs.
"Our study provided strong evidence that AI could really help in interpreting chest radiography. This will contribute to identifying chest diseases, especially lung cancer, more effectively at an earlier stage," Dr. Goo said.
The researchers plan to conduct a similar study using chest CT which will also identify clinical outcomes and efficiency of workflow.
"AI Improves Nodule Detection on Chest Radiographs in a Health Screening Population: A Randomized Controlled Trial." Collaborating with Dr. Goo were Ju Gang Nam, M.D., Ph.D., Eui Jin Hwang, M.D., Ph.D., Jayoun Kim, Ph.D., Nanhee Park, M.S., Eun Hee Lee, M.D., Ph.D., Hyun Jin Kim, M.D., Ph.D., Miyeon Nam, M.D., Jong Hyuk Lee, M.D., Ph.D., and Chang Min Park, M.D., Ph.D.
In 2023, Radiology is celebrating its 100th anniversary with 12 centennial issues, highlighting Radiology's legacy of publishing exceptional and practical science to improve patient care.
Radiology is edited by Linda Moy, M.D., New York University, New York, N.Y., and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research, and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on chest X-rays, visit RadiologyInfo.org.
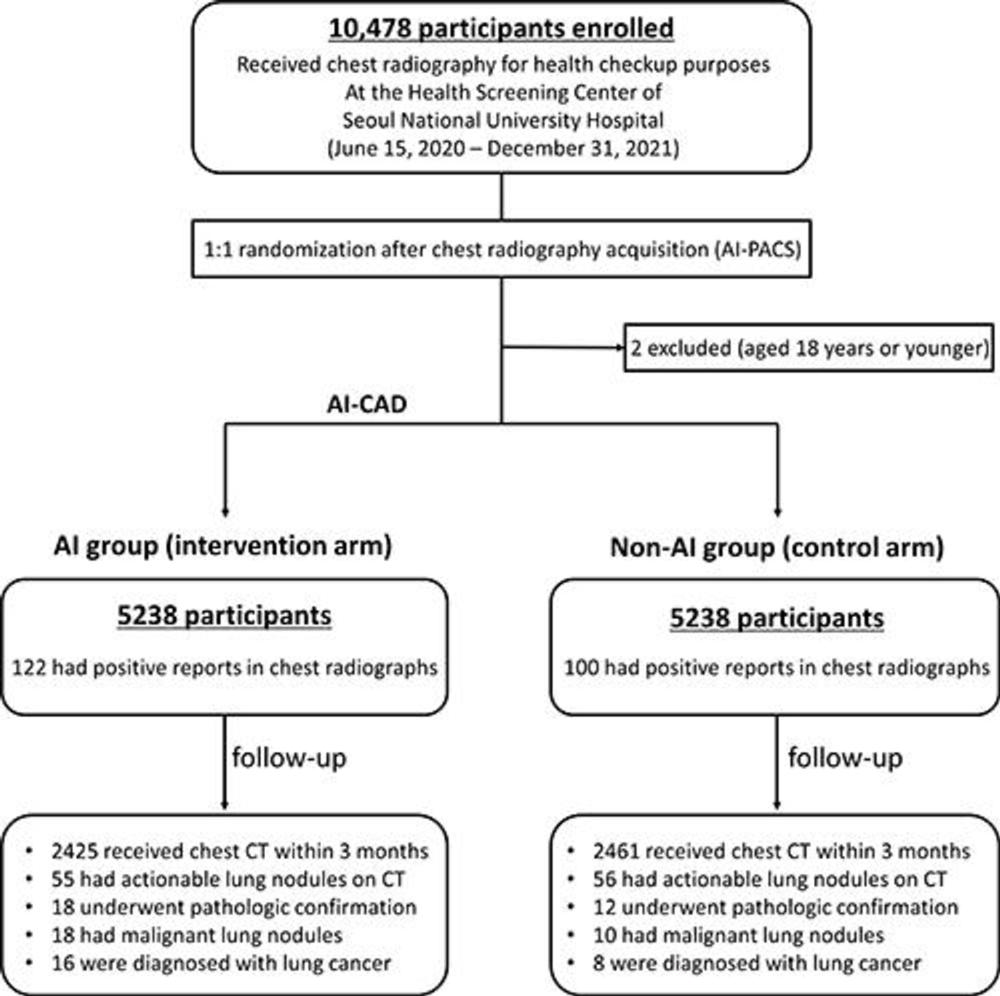
Figure 1. Participant flow diagram. AI = artificial intelligence, CAD = computer-aided detection, PACS = picture archiving and communication system.
High-res (TIF) version
(Right-click and Save As)
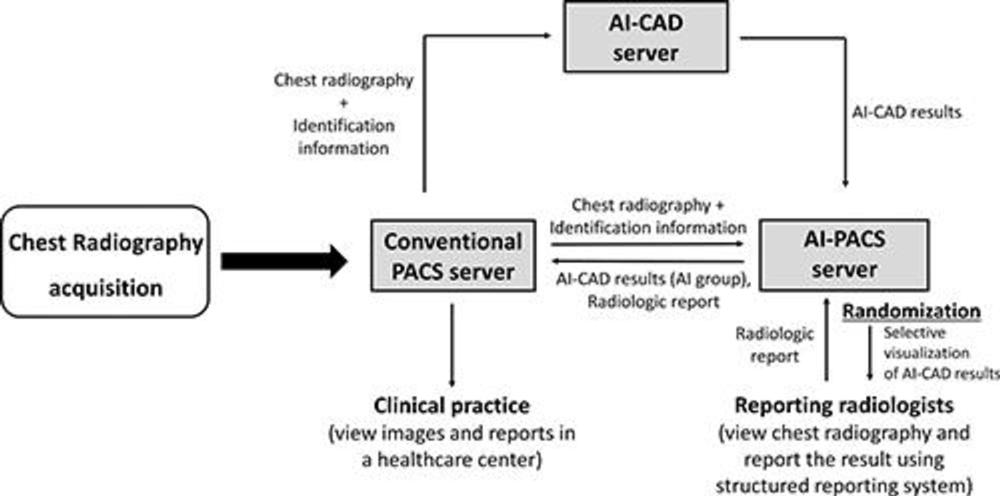
Figure 2. Work process of chest radiography interpretation during the clinical trial. When a chest radiograph was acquired at the health screening center, the image and identification information were immediately transmitted to the artificial intelligence (AI)–based computer-aided detection (CAD) server and AI picture archiving and communication system (PACS) server. The AI-based CAD server analyzed the image and sent the results to the AI-based CAD–implemented PACS (AIPACS) server, and the AI-PACS server randomized the participant into either the AI or non-AI group. If the participant was allocated to the AI group, the AI-PACS server provided AI-based CAD results and sent this information back to the conventional PACS server. These sequences took place immediately after the chest radiograph acquisition. The reporting radiologists viewed and reported chest radiographs using a structured reporting system implemented in the AI-PACS, and the final radiologic report was immediately sent to the conventional PACS server. Clinicians at the health screening center viewed the images and radiologic reports using the conventional PACS for clinical practice.
High-res (TIF) version
(Right-click and Save As)
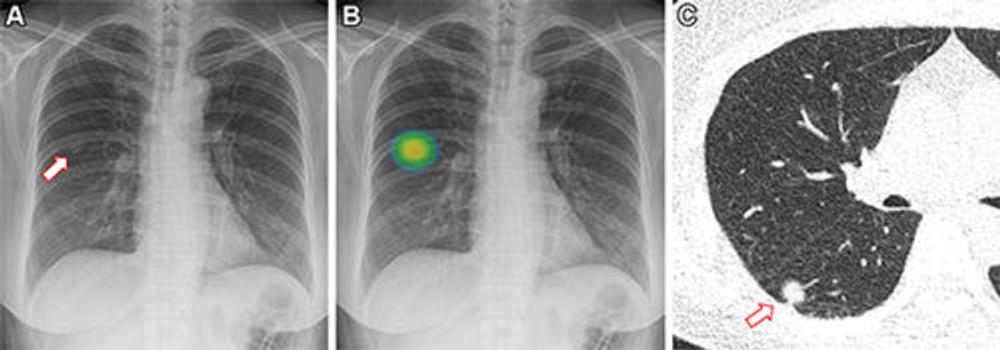
Figure 3. Images in a 60-year-old woman who underwent chest radiography for health checkup purposes and was allocated to the artificial intelligence (AI) group. (A) Frontal chest radiograph shows a subtle nodular opacity (arrow) in the right middle lung zone. (B) The lesion was detected by the AI-based computer-aided detection software, with an abnormality probability of 81.1%. The designated radiologist reported this chest radiograph as positive. (C) Axial, noncontrast, low-dose chest CT scan shows a 1.1-cm solid nodule (arrow) in the right lower lobe. The patient underwent percutaneous needle biopsy, and the nodule was confirmed to be adenocarcinoma.
High-res (TIF) version
(Right-click and Save As)
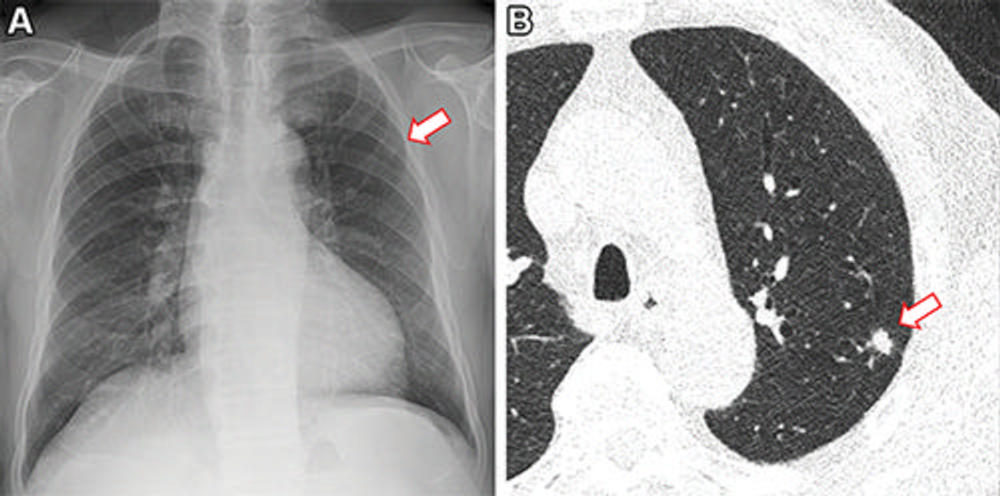
Figure 4. Images in a 73-year-old man who underwent chest radiography and low-dose CT for health checkup purposes and was allocated to the non–artificial intelligence (AI) group. (A) Frontal chest radiograph shows a small nodular opacity (arrow) in the left upper lung zone, which was missed by the designated reporting radiologist. (B) Axial, noncontrast, low-dose chest CT scan shows a 9-mm solid nodule (arrow) in the left upper lobe. The nodule showed low metabolism at PET and decreased in size at follow-up CT. It was confirmed to be an inflammatory nodule.
High-res (TIF) version
(Right-click and Save As)
