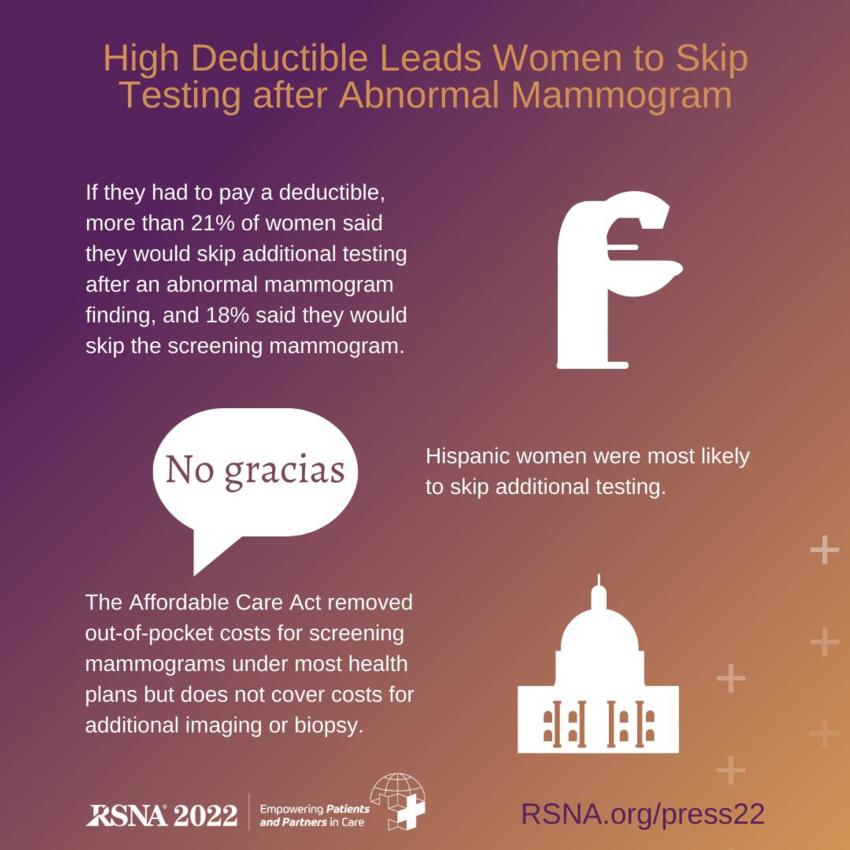
High Deductible Leads Women to Skip Testing after Abnormal Mammogram
Released: November 29, 2022
At A Glance
- If they had to pay a deductible, more than 21% of women said they would skip additional testing after an abnormal mammogram finding, and 18% said they would skip the screening mammogram.
- Hispanic women were most likely to skip additional testing.
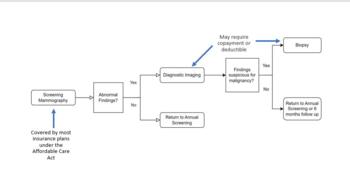
- The Affordable Care Act removed out-of-pocket costs for screening mammograms under most health plans but does not cover costs for additional imaging or biopsy.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
CHICAGO — One in five women is likely to forgo additional testing after an abnormal finding on a screening mammogram if there is a deductible, according to a new study presented today at the annual meeting of the Radiological Society of North America (RSNA).
As health care costs and insurance premiums have increased in recent years and with the advent of the Affordable Care Act (ACA), high-deductible health plans (HDHPs) have grown in popularity, particularly among younger, healthy people.
It is believed that HDHPs lower overall health care costs by making individuals more cognizant of their medical expenses. The higher deductible also lowers monthly insurance premiums, making these plans an attractive option for healthy people who may typically need coverage only for preventative care or health emergencies.
But while HDHPs offer some advantages, the high out-of-pocket deductible cost—in excess of $1,400 for individuals and $2,800 for families—may prevent people from seeking necessary care.
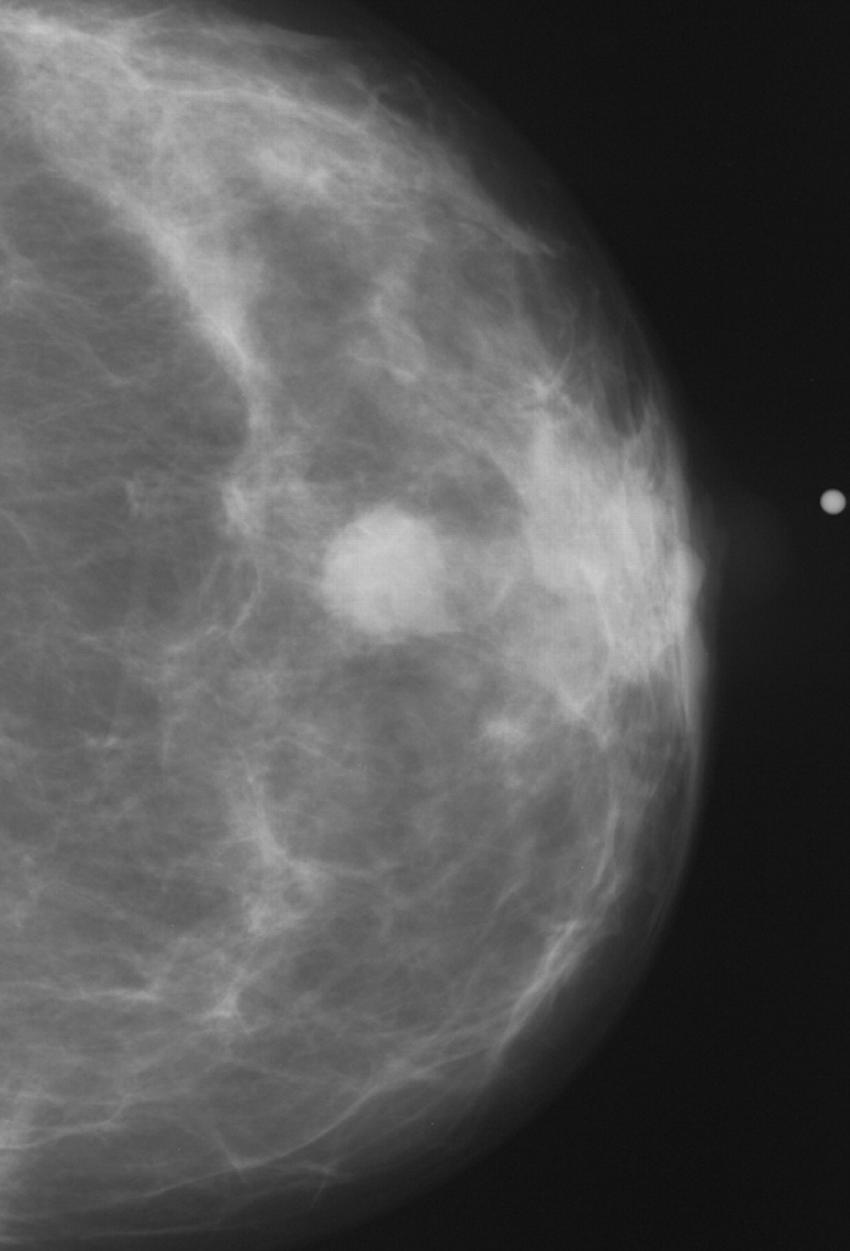
"The ACA removed out-of-pocket costs for screening mammograms under most health plans to encourage women to partake in this important preventative health care measure," said the study's lead author, Michael Ngo, M.D., radiology resident at Boston Medical Center and Boston University Chobanian & Avedisian School of Medicine. "However, the screening mammogram is only the first step in detecting breast cancer. If the radiologist detects an abnormal finding on the screening image, then additional images and a biopsy are needed to determine if the patient has cancer. The ACA does not mandate insurance to cover the costs of these additional services."
Dr. Ngo and colleagues set out to determine the relationship between HDHPs and patient's willingness to undergo indicated breast imaging.
"Prior studies have shown that out-of-pocket costs deter patients from attending screening mammography," Dr. Ngo said. "Other studies found that screening rates go down when there is an out-of-pocket cost for follow-up imaging after an abnormal finding on screening mammography. However, there is a lack of research into patient adherence to the recommended follow-up imaging when there is a deductible. Our research aims to address this paucity."
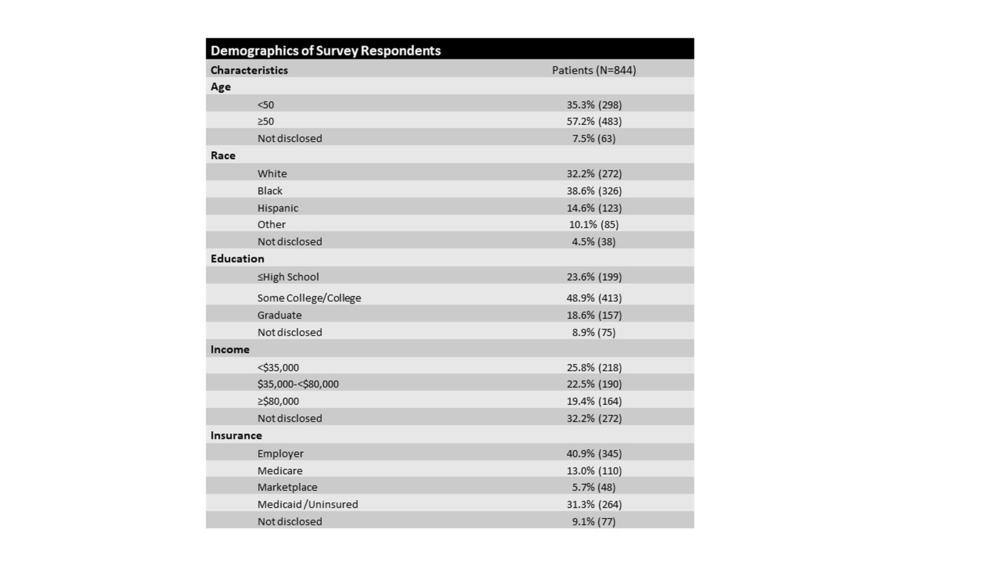
For the study, the researchers surveyed 932 patients presenting for breast imaging at Boston Medical Center between September 2021 and February 2022. The survey was comprised of demographic questions on race, education level, annual household income and insurance payor, as well as scenarios about utilization of breast imaging. There was a variable response rate on questions.
When asked whether they would skip indicated imaging if they knew they had to pay a deductible, of 714 respondents, 151 (21.2%) said they would skip imaging, 424 (59.4%) said they would not skip imaging, and 139 (19.5%) were undecided.
The groups with the highest percentage of responses indicating they would skip additional imaging were Hispanic (33.0%), high school educated or less (31.0%), household income less than $35,000 (27.0%) and Medicaid/uninsured (31.5%).
The survey also asked whether respondents would forgo the initial screening mammography exam if they knew they would have to pay a deductible for follow-up tests. Of 707 respondents, 129 (18.3%) said they would skip the screening mammography exam, 465 (65.8%) would not skip mammography, and 113 (16.0%) were undecided.
"The results show that a deductible payment for follow-up breast imaging after an abnormal finding on screening mammography discourages 21% of women from returning for additional evaluation and appears to lead 18% of women to skip the initial free screening altogether," Dr. Ngo said.
Identifying socioeconomic barriers to health care is critical in addressing existing disparities and ensuring better outcomes for vulnerable patient populations. The researchers hope that these findings will be useful in efforts to remove financial barriers to care.
"Our study demonstrates that out-of-pocket payments will discourage people, especially those belonging in the most vulnerable populations, from completing the last steps in the breast cancer screening process," Dr. Ngo said. "These results could be used to advocate for legislation that will cover these important follow-up tests and prevent further exacerbation of existing health inequities."
Co-authors are Geunwon Kim, M.D. Ph.D., Priscilla J. Slanetz, M.D., M.P.H., and Muhammad Qureshi, M.B.B.S., M.P.H.
Note: Copies of RSNA 2022 news releases and electronic images will be available online at RSNA.org/press22.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
Editor's note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA Newsroom at 1-312-791-6610.
For patient-friendly information on mammography, visit RadiologyInfo.org.
Video (MP4):

Video 1. Woman with radiologic technologist during screening mammography exam.
Download MP4
(Right-click and Save As)

Video 2. Radiologic technologist capturing mammography images.
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
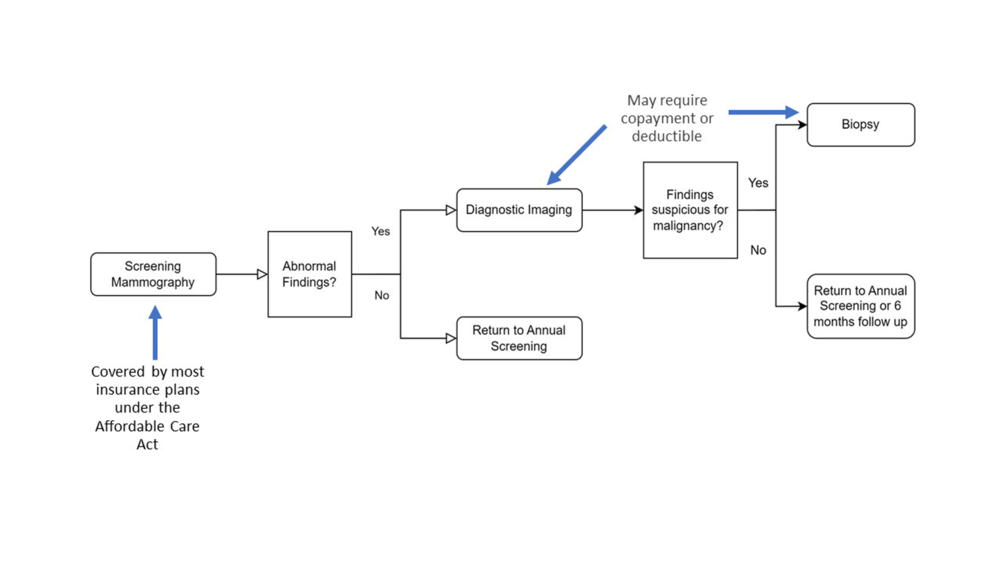
Figure 1. Flowchart of breast cancer detection process.
High-res (TIF) version
(Right-click and Save As)
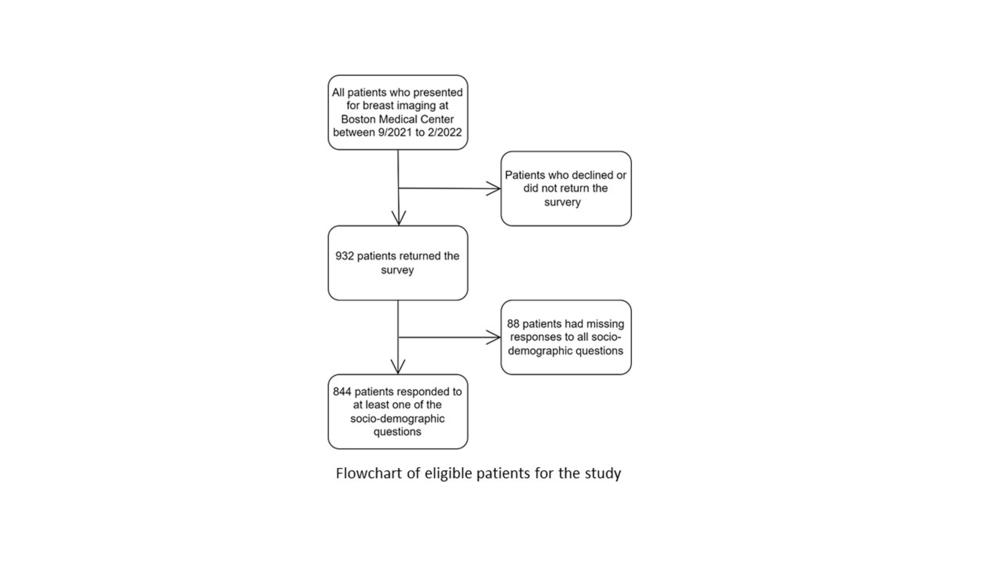
Figure 2. Flowchart of eligible patients for the study.
High-res (TIF) version
(Right-click and Save As)
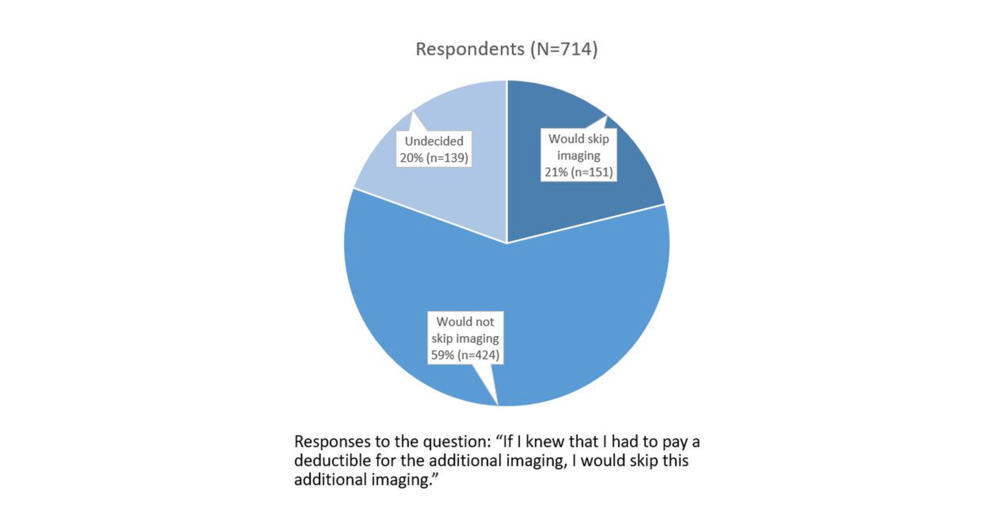
Figure 4. Pie chart of patient responses to additional imaging if they had to pay a deductible.
High-res (TIF) version
(Right-click and Save As)
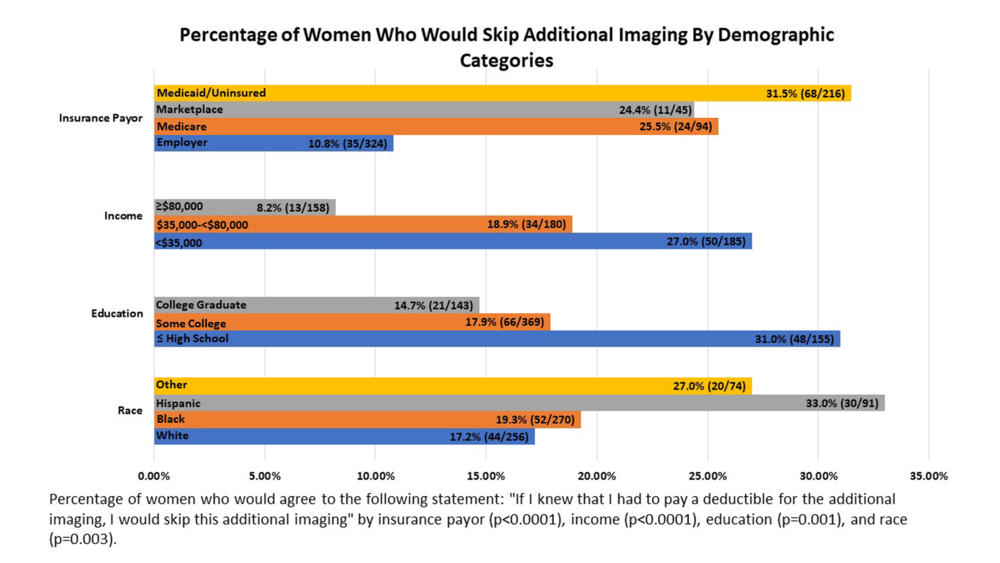
Figure 5. Bar graph of women who would skip additional imaging by demographic categories.
High-res (TIF) version
(Right-click and Save As)
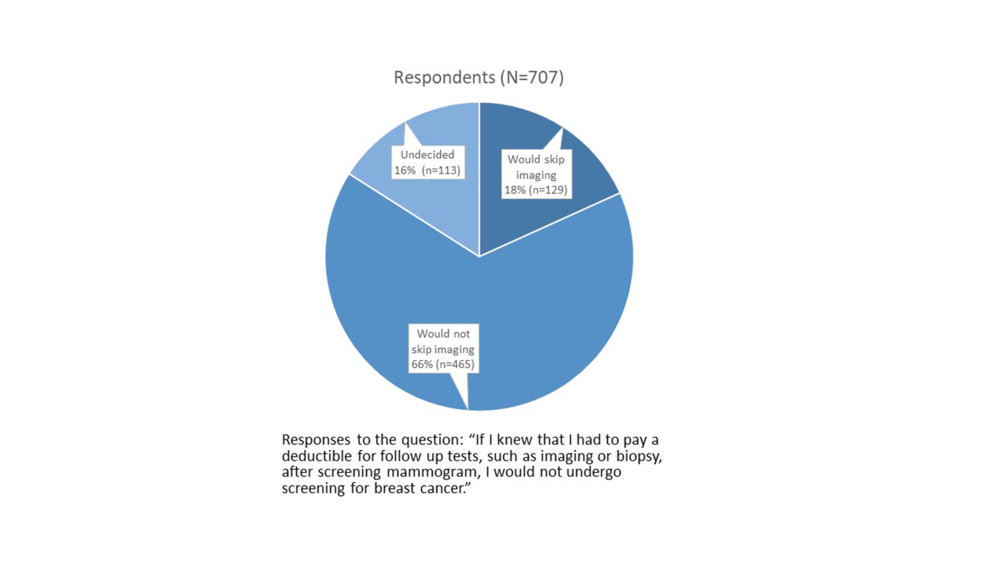
Figure 6. Pie chart of patient responses for follow-up testing (such as imaging or biopsy) after screening mammography if they had to pay a deductible.
High-res (TIF) version
(Right-click and Save As)
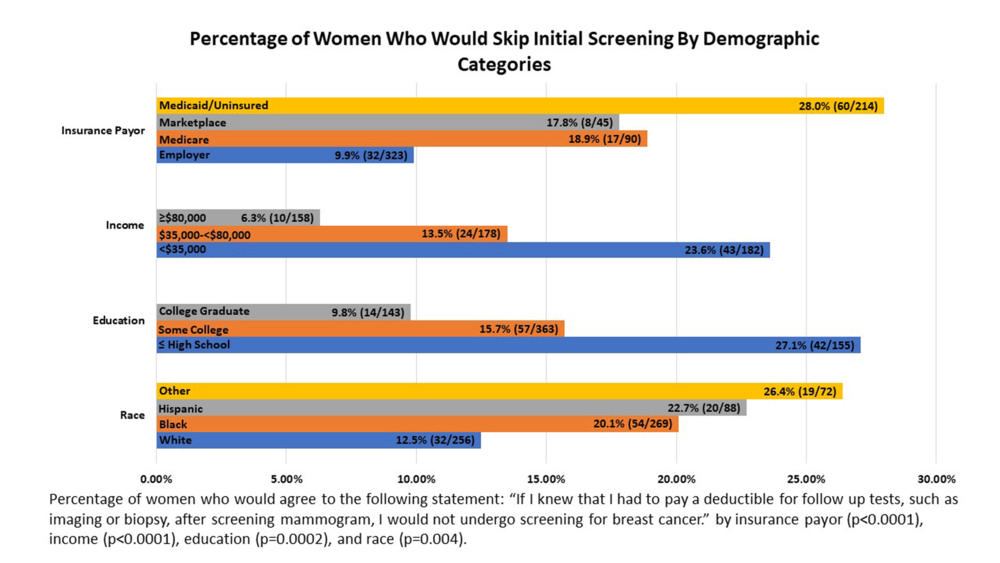
Figure 7. Bar graph of women who would skip initial screening by demographic categories.
High-res (TIF) version
(Right-click and Save As)

Figure 10. Woman with radiologic technologist during screening mammography exam.
High-res (TIF) version
(Right-click and Save As)

Figure 11. Woman with radiologic technologist during screening mammography exam.
High-res (TIF) version
(Right-click and Save As)
Powerpoint:
(Right-click and Save As)
Additional Resources