Novel Treatment Effective for Sidewall Brain Aneurysm
Released: April 19, 2022
At A Glance
- A novel mesh plug was found to be effective in treating aneurysms on the sidewall of blood vessels in the brain.
- Researchers compared the device in two types of aneurysms using a large database spanning more than 10 years from 23 institutions.
- The device closes off the aneurysm and reduces the risk of bleeding without requiring supporting stents or blood thinners.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — A novel mesh plug that has been traditionally used to treat brain aneurysms occurring where the blood vessels branch out was found to be equally effective in treating aneurysms on the side of the vessel, according to a study in the journal Radiology.
Aneurysms result from a weakness in the blood vessel wall that typically occurs where the vessel branches or bifurcates—where the vessel divides or forks into two branches. Untreated, an aneurysm can grow and rupture. A common treatment involving the placement of tiny platinum coils into the aneurysm has limitations.
"If the aneurysm has a wide neck, the coil might fall into the blood vessel and lead to clot formation and incomplete aneurysm occlusion," said study lead author Nimer Adeeb, M.D., from the Department of Neurosurgery and Interventional Neuroradiology at Louisiana State University in Shreveport, Louisiana. "Many times, you end up putting a stent in the blood vessel to prevent the coils from falling out and to keep them compacted within the aneurysm. This can have its own complications and requires using blood thinners."
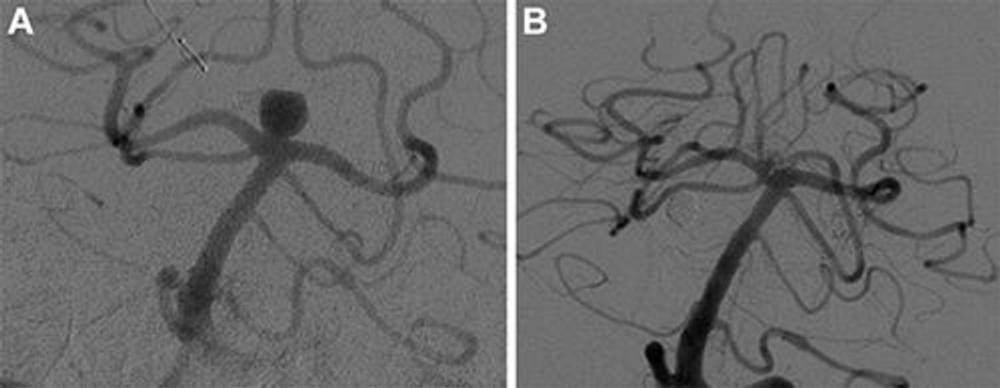
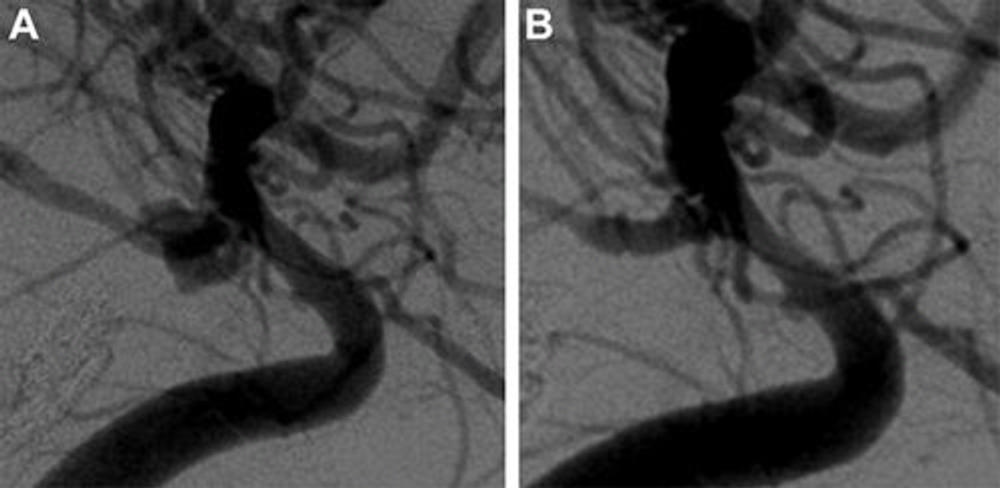
A braided wire device known as the Woven EndoBridge (WEB) was developed to overcome those limitations. The device is placed inside the aneurysm under angiographic guidance, where it causes a clot to form, closing off the aneurysm and reducing the risk of bleeding without requiring supporting stents or blood thinners.
"After you put the WEB device through the neck of the aneurysm, it opens up," Dr. Adeeb said. "Given that it's bigger than the neck of the aneurysm, it usually stays in place. One quick procedure is usually enough for successful treatment."
The U.S. Food and Drug Administration (FDA) approved the WEB device for wide-neck intracranial bifurcation aneurysms. Some specialists have used it off-label for the treatment of sidewall aneurysms, a type of wide-necked aneurysm that occurs at the side of a blood vessel rather than its bifurcation tip.
Research on the WEB device's use in wide-necked sidewall aneurysms has been limited to studies with a small number of cases.
For the new study, Dr. Adeeb and colleagues compared the WEB device in bifurcation and sidewall aneurysms using a large database spanning more than 10 years from the WorldWideWEB consortium, a group of 23 academic institutions in North America, South America, Australia and Europe. Dr. Adeeb co-led the effort with Adam A. Dmytriw, M.D., from Massachusetts General Hospital in Boston.
A total of 683 intracranial aneurysms were treated using the WEB device in 671 patients. Of those, 572 were bifurcation aneurysms, and 111 were sidewall aneurysms. Propensity score matching, a way to increase the power of a study by accounting for differences in patients, resulted in 91 bifurcation and sidewall aneurysms pairs.
The complication rate was very similar between the two approaches.
"We found out that there is no significant difference using the WEB device in sidewall aneurysms compared with bifurcation aneurysms," Dr. Adeeb said. "The results show that the WEB device is safe and effective to use for sidewall aneurysms."
Dr. Adeeb hopes that the study will help drive a discussion about expanding the indications for the WEB device to include certain sidewall aneurysms.
As additional institutions continue to join the consortium, Dr. Adeeb and his colleagues are continuing the research, comparing the WEB device with other treatments for different types and locations of aneurysms. They also plan to track changes that happen to device shape and compaction over time and its relationship to aneurysm occlusion status.
"Our ultimate goal is to provide our patients with the best possible treatment for their brain aneurysms," he said.
"Multicenter Study for the Treatment of Sidewall versus Bifurcation Intracranial Aneurysms with Use of Woven EndoBridge (WEB)." Collaborating with Drs. Adeeb and Dmytriw were Mahmoud Dibas, M.D., Jose Danilo Bengzon Diestro, M.D., Hugo H. Cuellar-Saenz, M.D., Ahmad Sweid, M.D., Sandeep Kandregula, M.D., Sovann V. Lay, M.D., Adrien Guenego, M.D., Leonardo Renieri, M.D., Sri Hari Sundararajan, M.D., Guillaume Saliou, M.D., Ph.D., Assala Aslan, M.D., Markus Möhlenbruch, M.D., Justin E. Vranic, M.D., Robert W. Regenhardt, M.D., Ph.D., Amey Savardekar, M.D., Ahmed Mamilly, M.D., Ivan Lylyk, M.D., Paul M. Foreman, M.D., Jay A. Vachhani, M.D., Vedran Župančić, M.D., Muhammad U. Hafeez, M.D., Caleb Rutledge, M.D., Muhammad Waqas, M.B.B.S., Carmen Parra Farinas, M.D., Vincent M. Tutino, Ph.D., Yasuaki Inoue, M.D., Shervin Mirshahi, M.D., James D. Rabinov, M.D., Yifan Ren, M.D., Clemens M. Schirmer, M.D., Ph.D., Mariangela Piano, M.D., Anna L. Kühn, M.D., Ph.D., Caterina Michelozzi,,M.D., Stéphanie Elens, M.D., Robert M. Starke, M.D., Ameer Hassan, D.O., Arsalaan Salehani, M.D., Peter Sporns, M.D., Alex Brehm, M.D., Jesse Jones, M.D., Marios Psychogios, M.D., Julian Spears, M.D., M.S., Boris Lubicz, M.D., Ph.D., Pietro Panni, M.D., Ajit S. Puri, M.D., Guglielmo Pero, M.D., Christoph J. Griessenauer, M.D., Hamed Asadi, M.D., Ph.D., Christopher J. Stapleton, M.D., Adnan Siddiqui, M.D., Andrew F. Ducruet, M.D., Felipe C. Albuquerque, M.D., Peter Kan, M.D., Vladimir Kalousek, M.D., Pedro Lylyk, M.D., Srikanth Boddu, M.D., M.Sc., Jared Knopman, M.D., Mohammad A. Aziz-Sultan, M.D., Nicola Limbucci, M.D., Pascal Jabbour, M.D., Christophe Cognard, M.D., and Aman B. Patel, M.D. For the WorldWideWEB Consortium.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on brain imaging, visit RadiologyInfo.org.
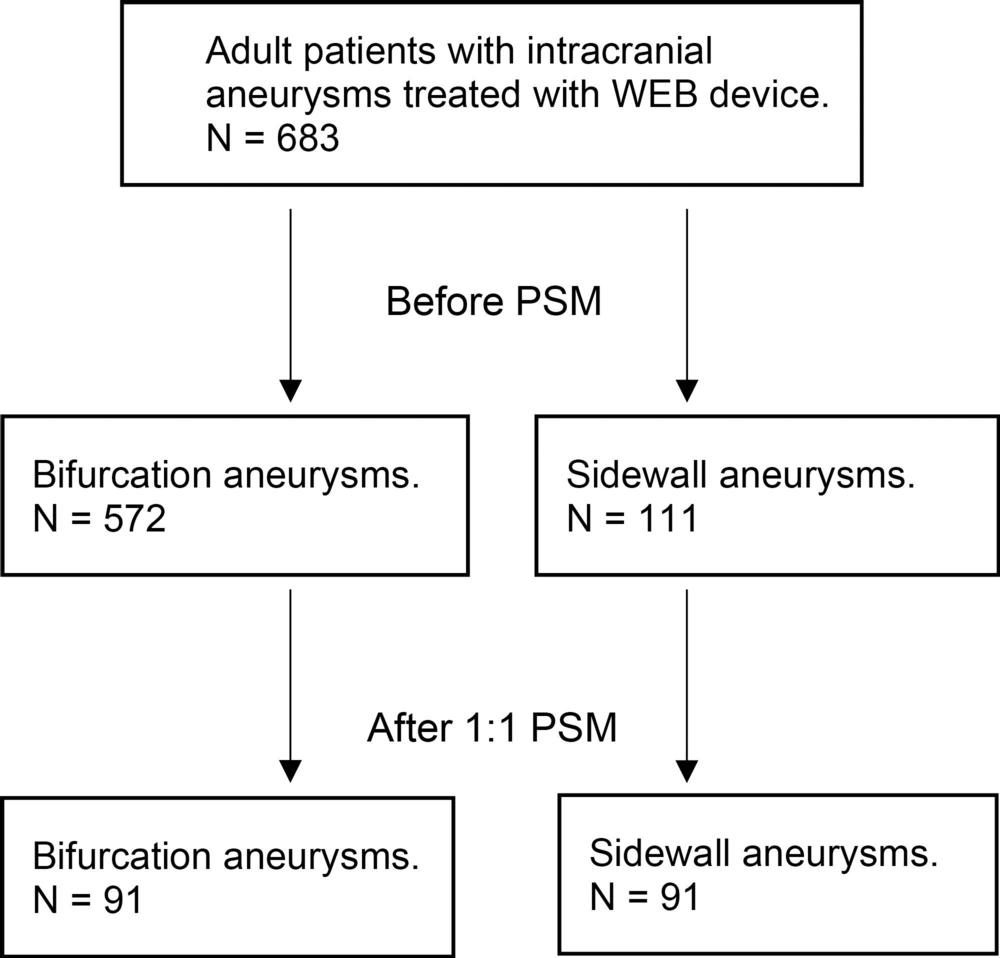
Figure 1. Flowchart shows the inclusion for patients and aneurysms in this study. PSM = propensity score matching, WEB = Woven EndoBridge.
High-res (TIF) version
(Right-click and Save As)