Study Finds COVID-19 Less Severe in Fully Vaccinated
Released: February 01, 2022
At A Glance
- Approximately 59% of fully vaccinated patients had no evidence of COVID-19 pneumonia on CT, compared to 22% of unvaccinated patients.
- Fully and partially vaccinated patients were at significantly lower risk of requiring supplemental oxygen or ICU admission.
- In the study, 6.2% of COVID-19 patients were breakthrough infections.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
OAK BROOK, Ill. — The clinical and imaging characteristics of COVID-19 breakthrough infections in fully vaccinated patients tend to be milder than those of partially vaccinated or unvaccinated patients, according to a new multicenter study published in the journal Radiology.
The number of confirmed COVID-19 cases worldwide now exceeds 270 million with an overall mortality rate of approximately 2%.
COVID-19 vaccines are effective and critical tools for bringing the pandemic under control. However, vaccines are not 100% effective at preventing illness. Breakthrough infections are defined as the detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) ribonucleic acid (RNA) or antigen in a respiratory specimen collected from a person 14 days or more after receiving all recommended doses of COVID-19 vaccines.
Breakthrough cases are on the rise with the highly transmissible Omicron variant. Therefore, it is important to know how vaccination impacts not only COVID-19 disease severity but also clinical data and medical imaging results.
“Although the risk of infection is much lower among vaccinated individuals, and vaccination reduces the severity of illness, clinical and imaging data of COVID-19 breakthrough infections have not been reported in detail,” said the study’s senior author, Yeon Joo Jeong, M.D., Ph.D., from the Department of Radiology and Biomedical Research Institute at Pusan National University Hospital in Busan, South Korea. “The purpose of this study was to document the clinical and imaging features of COVID-19 breakthrough infections and compare them with those of infections in unvaccinated patients.”
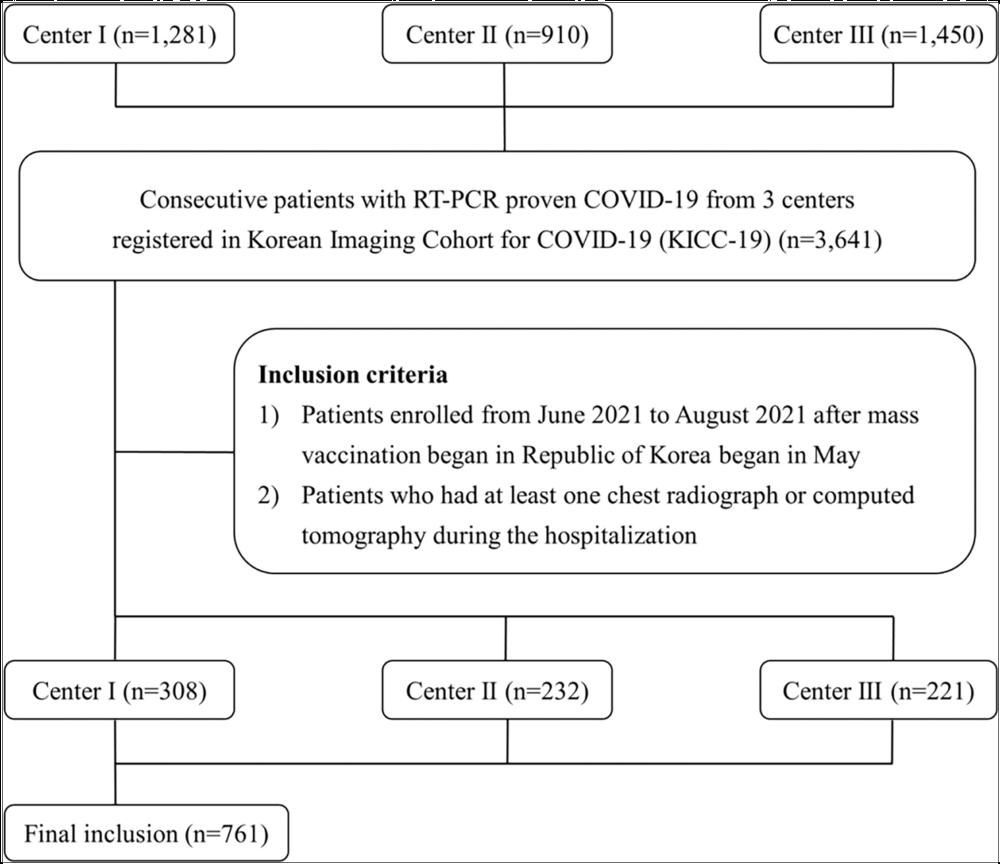
In this retrospective multicenter cohort study, Dr. Jeong and colleagues analyzed data from adult patients registered in an open data repository for COVID-19—Korean Imaging Cohort for COVID-19 (KICC-19)—between June and August 2021. Hospitalized patients with baseline chest X-rays were divided into three groups, according to their vaccination status. The researchers evaluated differences between clinical and imaging features and analyzed associations between clinical factors—including vaccination status—and clinical outcomes.
Of the 761 hospitalized patients with COVID-19, the mean age was 47 years, and 385 (51%) were women. Forty-seven patients (6.2%) were fully vaccinated (breakthrough infection), 127 were partially vaccinated (17%), and 587 (77%) were unvaccinated. Chest CT scans were performed on 412 (54%) of the patients during hospitalization. Of patients undergoing CT, the proportion of CT scans without pneumonia was 22% (71/326) of unvaccinated patients, 30% (19/64) of partially vaccinated patients, and 59% (13/22) of fully vaccinated patients. Fully vaccinated status was associated with a lower risk of requiring supplemental oxygen than unvaccinated status, as well as lower risk of intensive care unit (ICU) admission.
The results also showed associations between the risk of severe disease and clinical characteristics such as higher age, history of diabetes, lymphocytopenia, thrombocytopenia, elevated LDH (lactate dehydrogenase), and elevated CRP (C-reactive protein). Notably, age was also found to be an important predictor of more severe disease in COVID-19 patients, even in those with a breakthrough infection.
The researchers noted that observed differences in clinical characteristics may reflect differences in vaccination priorities based on underlying comorbidities. During the study period, high-risk groups, such as individuals over 65 years old, health care workers and people with disabilities were priority targets for COVID-19 vaccination. Therefore, elderly patients and patients with at least one comorbidity were more common in the vaccinated group than in unvaccinated group in the study.
“Despite these differences, mechanical ventilation and in-hospital death occurred only in the unvaccinated group,” Dr. Jeong said. “Furthermore, after adjusting for baseline clinical characteristics, analysis showed that fully vaccinated patients were at significantly lower risk of requiring supplemental oxygen and of ICU admission than unvaccinated patients.”
Although additional research will be needed as different variants emerge, this study sheds light on the clinical effectiveness of COVID-19 vaccination in the context of breakthrough infections.
“Imaging and Clinical Features of COVID-19 Breakthrough Infections: A Multicenter Study.” Collaborating with Dr. Jeong were Jong Eun Lee, M.D., Minhee Hwang, M.D., Yun-Hyeon Kim, M.D., Ph.D., Myung Jin Chung, M.D., Ph.D., Byeong Hak Sim, M.D., Kum Ju Chae, M.D., and Jin Young Yoo, M.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on chest CT, visit RadiologyInfo.org.
Images (JPG, TIF):
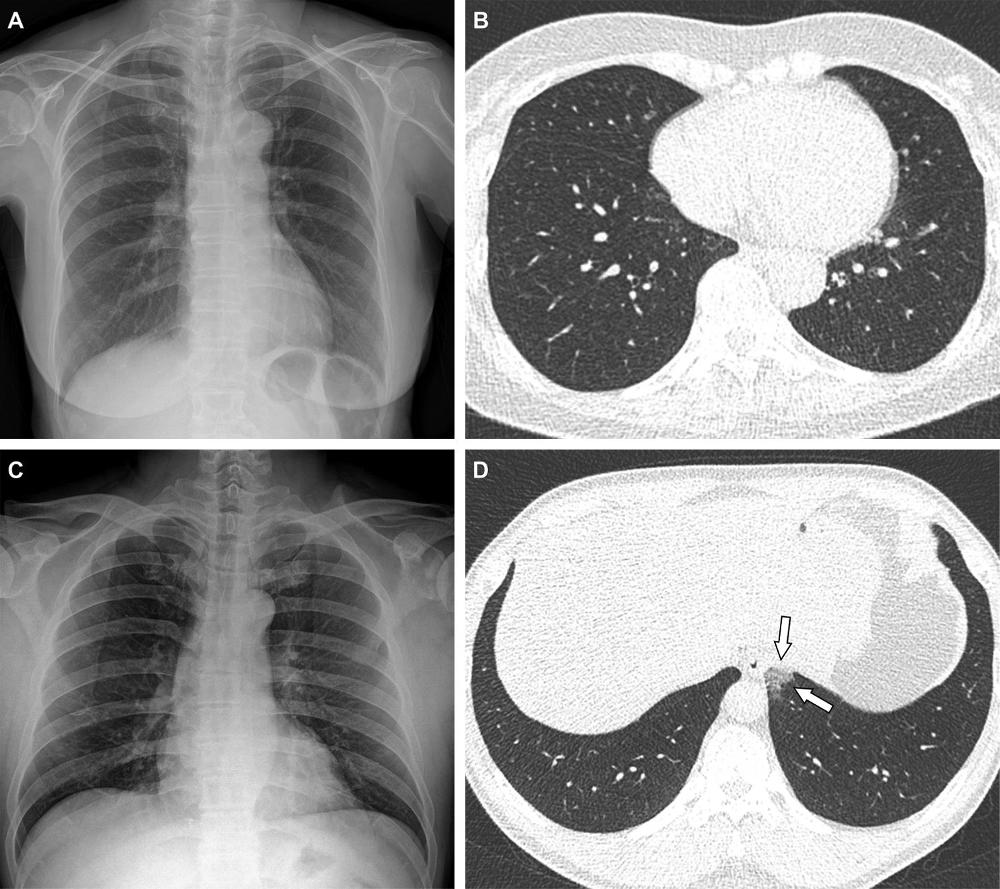
Figure 2. Representative cases showing pneumonia extents and patterns on chest X-ray (CXR) and CT images. (A and B) A 65-year-old female with breakthrough infection 2 months after a second dose of the Pfizer vaccine (fully vaccinated). The patient had a history of hypertension. (A) CXR obtained at admission showing no abnormal opacification in both lung zones. The CXR extent of pneumonia was scored as 0 (no evidence of pneumonia). (B) Axial chest CT image at the lower lobe level (obtained on the same day) showing negatively for pneumonia; CT extent of pneumonia was scored as 0 (no evidence of pneumonia). (C and D) A 48-year-old male with 1 month after a first dose of the AstraZeneca vaccine (partially vaccinated). The patient had no history of comorbidity. (C) CXR obtained at admission showing no abnormal opacification in both lung zones. The CXR extent of pneumonia was scored as 0 (no evidence of pneumonia). (D) Axial chest CT image obtained on the same day showing unilateral ground-glass opacity with a non-rounded morphology in the left lower lobe (arrows). CT extent of pneumonia was scored as 1 (1-25% involvement) and this case was classified as indeterminate appearance of COVID-19 according to the RSNA chest CT classification system.
High-res (TIF) version
(Right-click and Save As)
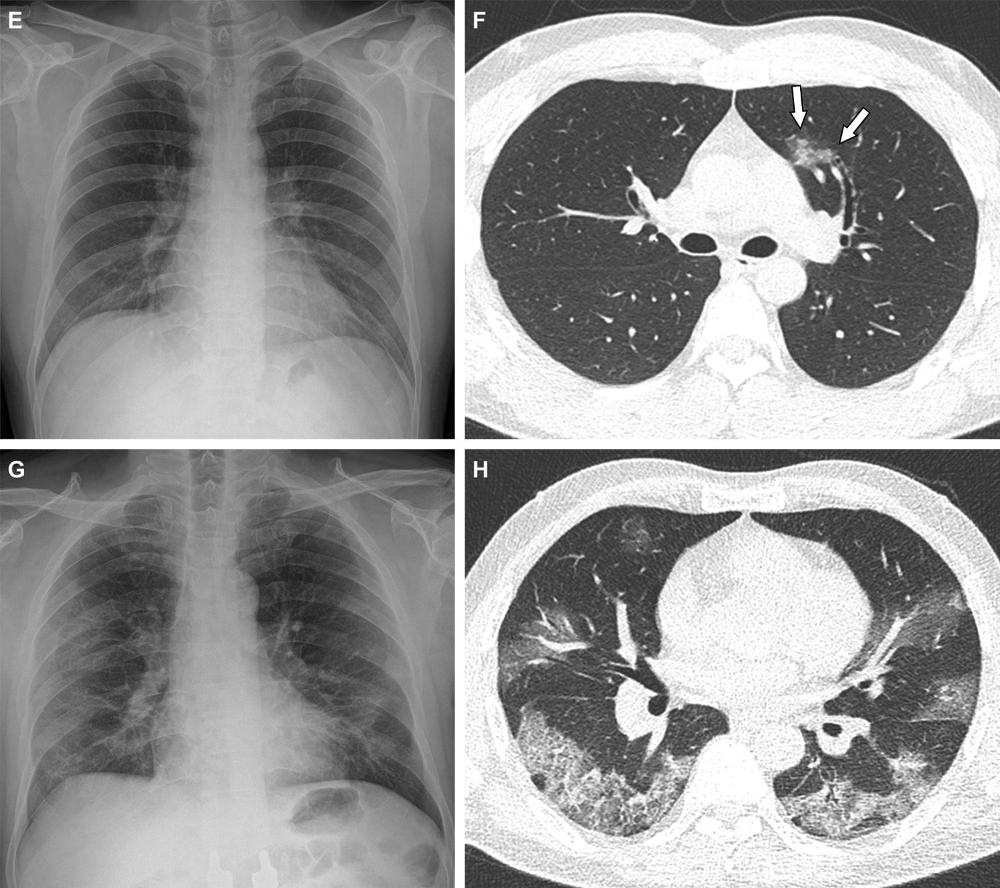
Figure 3. Representative cases showing pneumonia extents and patterns on chest X-ray (CXRs) and CT images. (E and F) A 36-year-old male with no history of vaccination for COVID- 19. The patient had no history of comorbidity. (E) CXR obtained at admission showing no abnormal opacification in either lung zone. CXR extent of pneumonia was scored as 0 (no evidence of pneumonia). (F) Axial chest CT image obtained on the same day showing unilateral ground-glass opacity with a nonrounded morphology and non-peripheral distribution in the left upper lobe (arrows). CT extent of pneumonia was scored as 1 (1-25% involvement) and this case was classified as indeterminate appearance of COVID-19 according to the RSNA chest CT classification system. (G and H) A 58-year-old male with no history of COVID-19 vaccination. The patient had a history of hypertension and diabetes. He required supplemental oxygen on admission and was admitted to intensive care unit one day later. (G) CXR at admission showing patchy ground-glass opacities in both middle- to lower-lung zones. CXR extent of pneumonia was scored as 2 (>25% involvement). (H) Axial chest CT image obtained on the same day showing multifocal ground-glass opacities with a crazy-paving appearance in bilateral lungs. CT extent of pneumonia was scored as 2 (>25% involvement) and was classified as typical appearance of COVID-19 according to the RSNA chest CT classification system.
High-res (TIF) version
(Right-click and Save As)
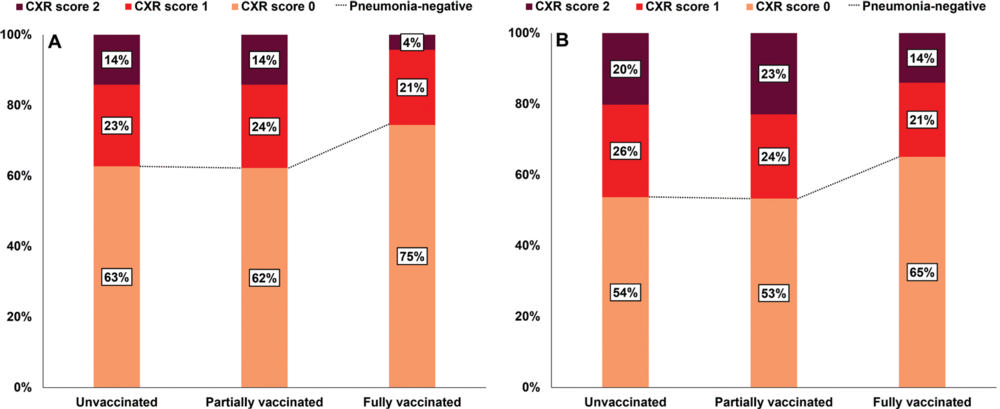
Figure 4. Initial and follow-up CXR scores in the 761 patients by vaccination status. (A) The proportion with an initial CXR score of 0 was highest in the fully vaccinated group than in the partially vaccinated or unvaccinated groups, but not significantly so (P = .37). (B) The proportion of patients with CXR score of 0 during follow-up was also highest in the fully vaccinated group, but not significantly so (P = .78).
High-res (TIF) version
(Right-click and Save As)
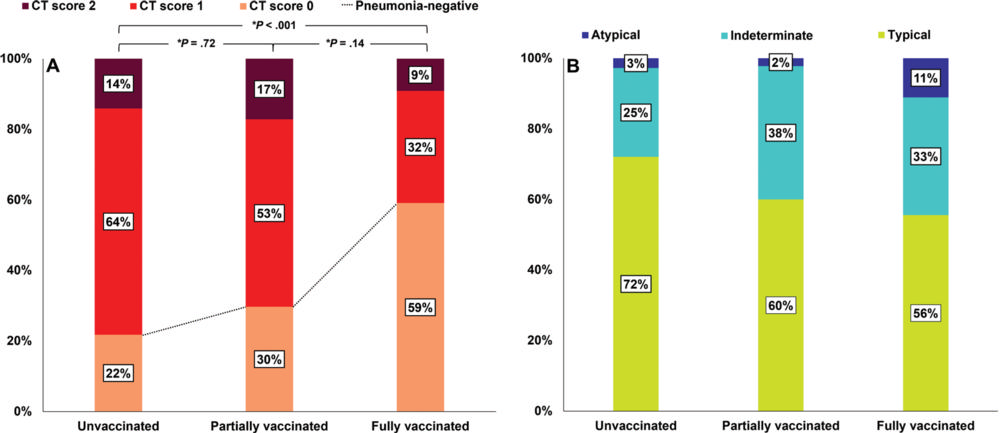
Figure 5. CT scores and patterns of the 412 patients that underwent chest CT during hospitalization by vaccination status. (A) The proportion with a CT score of 0 was significantly greater in the fully vaccinated group than in the unvaccinated groups (*P < .001). *P indicates Bonferroni adjusted P value which determined by multiplying the raw P value by 3. (B) Among patients with pneumonia, CT patterns were not significantly different between the groups (P = .22).
High-res (TIF) version
(Right-click and Save As)
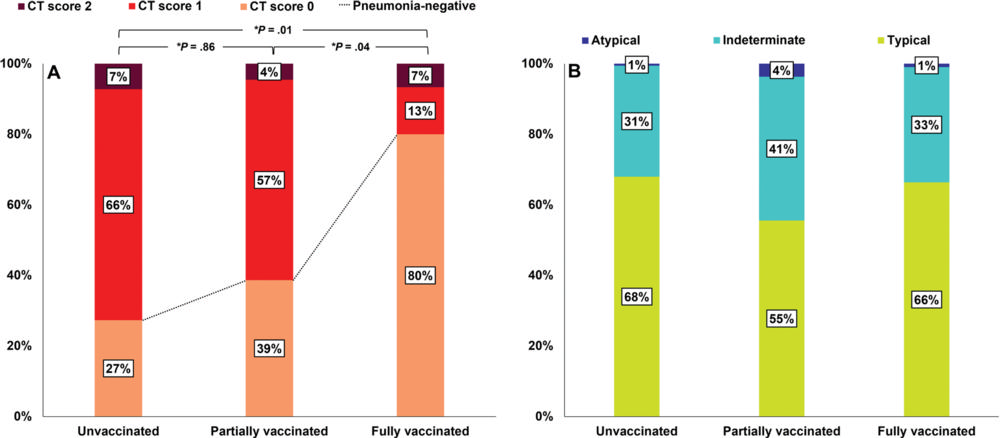
Figure 6. CT scores and patterns of the 308 patients in Center 1 by vaccination status. In Center 1, patients with asymptomatic or mild symptoms were hospitalized and all patients underwent initial chest CT scans. (A) The proportion with a CT score of 0 was significantly higher in the fully vaccinated group than in the partially or unvaccinated groups (*P = .04 and .01, respectively). *P indicates Bonferroni adjusted P value which determined by multiplying the raw P value by 3. (B) Among patients with pneumonia, CT patterns are not significantly different between the groups (P = .46).
High-res (TIF) version
(Right-click and Save As)