Large International Study Reveals Spectrum of COVID-19 Brain Complications
Released: November 29, 2021
At A Glance
- Central nervous system disorders are important complications in COVID-19, affecting more than one in 100 hospitalized patients.
- Researchers looked at almost 40,000 cases of hospitalized COVID-19 positive patients from seven U.S. and four western European university hospitals.
- There were 442 acute neuroimaging findings that were most likely associated with the viral infection, the most common being ischemic stroke.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - RSNA 2021 Newsroom
(Nov. 27-Dec. 2, 2021)
1-312-791-6610 - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Imani Harris
1-630-481-1009
iharris@rsna.org
CHICAGO — The largest multi-institutional international study to date on brain complications of COVID-19 has found that approximately one in 100 patients hospitalized with COVID-19 will likely develop complications of the central nervous system. These can include stroke, hemorrhage, and other potentially fatal complications. The study is being presented tomorrow at the annual meeting of the Radiological Society of North America (RSNA).
“Much has been written about the overall pulmonary problems related to COVID-19, but we do not often talk about the other organs that can be affected,” said study lead author Scott H. Faro, M.D., FASFNR, professor of radiology and neurology and director of the Division of Neuroradiology/Head & Neck Imaging at Thomas Jefferson University in Philadelphia. “Our study shows that central nervous system complications represent a significant cause of morbidity and mortality in this devastating pandemic.”
Dr. Faro initiated the study after discovering that existing literature on central nervous system complications in hospitalized COVID-19 infected patients was based on a relatively small number of cases.
To derive a more complete picture, he and his colleagues analyzed nearly 40,000 cases of hospitalized COVID-19 positive patients from seven U.S. and four western European university hospitals. The patients had been admitted between September 2019 and June 2020. Their average age was 66 years old, and there were twice as many men as women.
The most common cause of admission was confusion and altered mental status, followed by fever. Many of the patients had comorbidities like hypertension, cardiac disease and diabetes.
There were 442 acute neuroimaging findings that were most likely associated with the viral infection. The overall incidence of central nervous system complications in this large patient group was 1.2%.
“Of all the inpatients who had imaging such as MRI or a CT scan of brain, the exam was positive approximately 10% of the time,” Dr. Faro said. “The incidence of 1.2% means that a little more than one in 100 patients admitted to the hospital with COVID-19 are going to have a brain problem of some sort.”
The most common complication was ischemic stroke, with an incidence of 6.2%, followed by intracranial hemorrhage (3.72%) and encephalitis (0.47%), an inflammation of the brain.
The researchers also discovered a small percentage of unusual findings, such as acute disseminating encephalomyelitis, an inflammation of the brain and spinal cord, and posterior reversible encephalopathy syndrome, a syndrome that mimics many of the symptoms of a stroke.
“It is important to know an accurate incidence of all the major central nervous system complications,” Dr. Faro said. “There should probably be a low threshold to order brain imaging for patients with COVID-19.”
Co-authors are Arichena Manmatharayan, M.B.B.S., Benjamin Leiby, Ph.D., Neelu Jain, M.D., Feroze B. Mohamed, Ph.D., Kiran S. Talekar, M.D., Amish Doshi, M.D., M.B.B.S., Ivan Jambor, M.D., Ph.D., Chang Sanders, M.D., Mark Finkelstein, M.D., Stephane Kremer, M.D., Ph.D., Francois Lercy, M.D., Brenden Lindgren, D.O., Nathalia M. Figueidero, M.D., Varun Sethi, M.D., Simonetta Gerevini, M.D., Angela Napolitano, M.D., Rajan Jain, M.D., Siddhanth Dogra, B.S., Jay Pillai, M.D., Dan Ryan, M.D., Rolf Jager, FRCR, Francesco Carletti, M.D., Ph.D., Asim Mian, M.D., Artem Kaliev, Priya Anand, M.D., Courtney Takahashi, M.D., AK Murat, M.D., Rivka Colen, M.D., and Francesca Pizzini, M.D., Ph.D.
Note: Copies of RSNA 2021 news releases and electronic images will be available online at RSNA.org/press21.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
Editor’s note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA Newsroom at 1-312-791-6610.
For patient-friendly information on brain imaging, visit RadiologyInfo.org.
Images (JPG, TIF):

Figure 1. Stroke seen in a 41-year-old male patient with COVID-19 infection.
High-res (TIF) version
(Right-click and Save As)
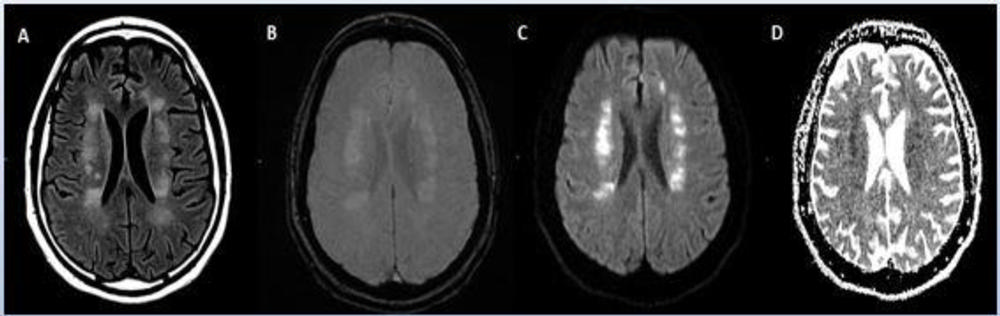
Figure 2. Acute anterior cerebral artery/middle cerebral artery watershed infarction seen in a 47-year-old male patient who presented with COVID-19 pneumonia. Watershed infarctions occur at the border between cerebral vascular territories where the tissue is furthest from arterial supply and thus most vulnerable to reductions in perfusion, or passage of fluid.
High-res (TIF) version
(Right-click and Save As)
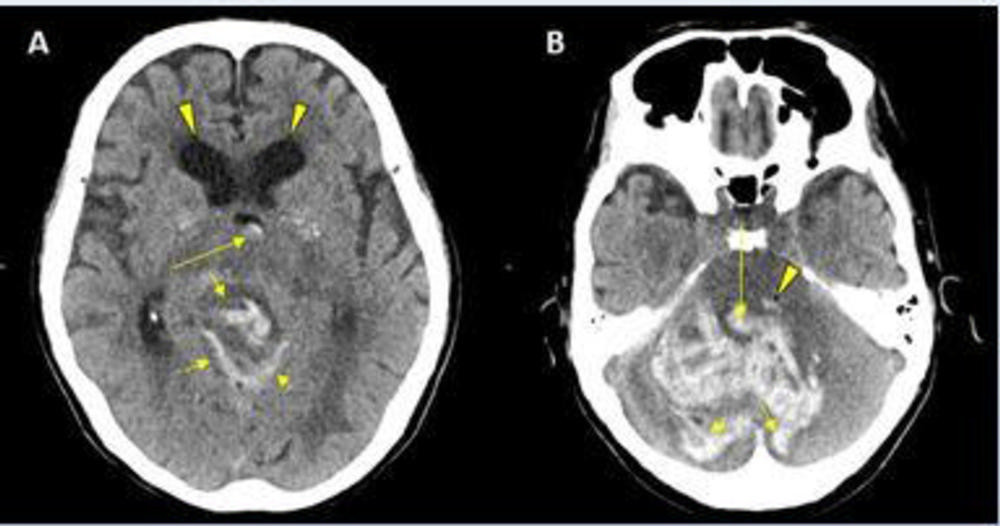
Figure 3. CT showing hemorrhage in a 68-year-old male patient with COVID-19 infection.
High-res (TIF) version
(Right-click and Save As)
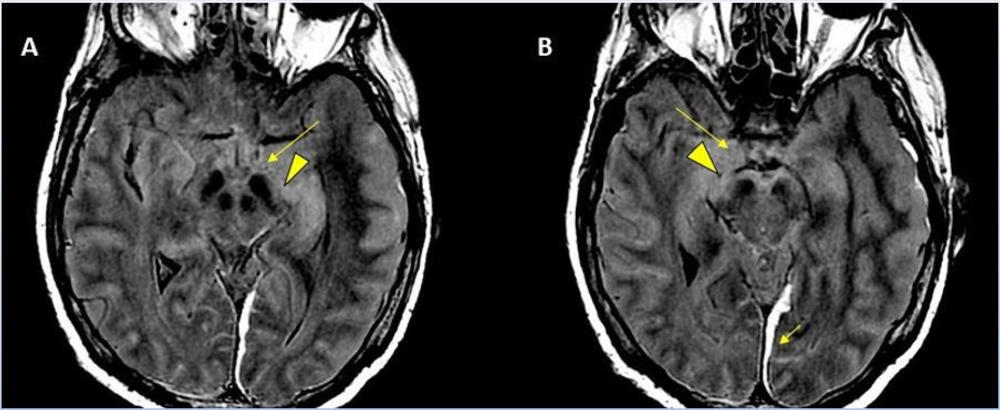
Figure 4. 62-year-old male with a past medical history of hypertension presenting with seizures.
High-res (TIF) version
(Right-click and Save As)

Figure 5. 56-year-old male patient with diabetes and hypertension who presented with complaints of confusion.
High-res (TIF) version
(Right-click and Save As)
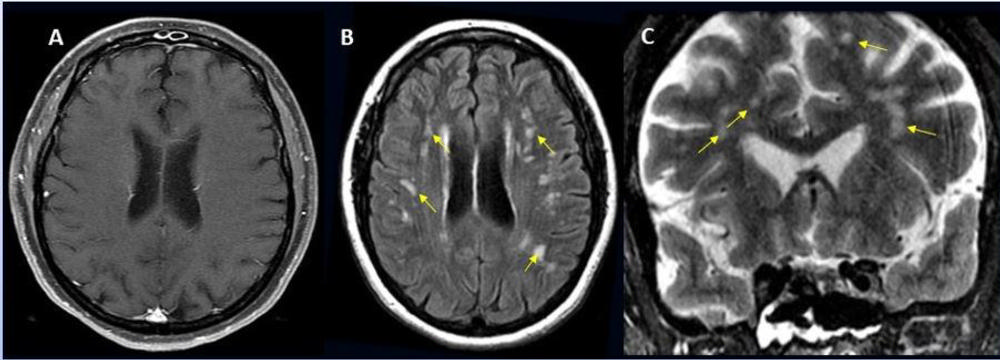
Figure 6. 49-year-old female with past medical history of mitral valve disease and tricuspid valve regurgitation who developed headache followed by cough and fever presented to the ER with right upper eyelid ptosis (drooping).
High-res (TIF) version
(Right-click and Save As)

Figure 7. Hemorrhage seen in 56-year-old female with COVID-19 infection and no other significant past medical history.
High-res (TIF) version
(Right-click and Save As)
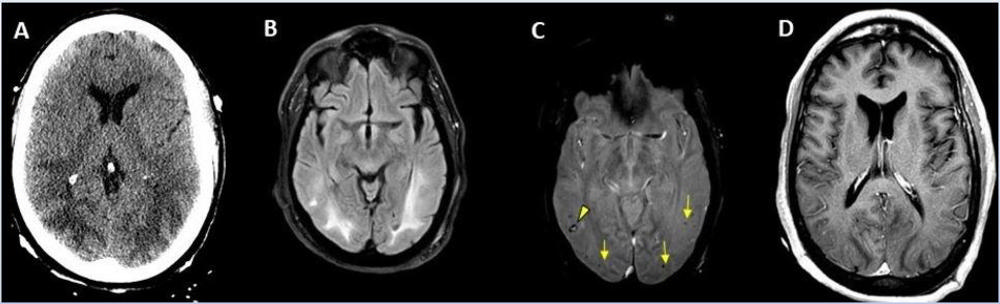
Figure 8. 65-year-old male smoker, presented with acute hypoxic respiratory failure secondary to COVID-19 pneumonia, requiring intubation. Hospitalization was complicated by seizures relating to cerebral edema and hemorrhagic posterior reversible encephalopathy syndrome.
High-res (TIF) version
(Right-click and Save As)
Powerpoint: