AI Helps Rule Out Cancer in Dense Breasts
Released: October 05, 2021
At A Glance
- AI can quickly and accurately sift through breast MRIs in women with dense breasts to eliminate those without cancer.
- More than 4,500 MRI datasets of extremely dense breasts were used to develop and train a deep learning model to distinguish between breasts with and without lesions.
- The deep learning model dismissed about 40% of the lesion-free MRIs without missing any cancers.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Katherine Anderson
1-630-491-1009
kanderson@rsna.org
OAK BROOK, Ill. — An automated system that uses artificial intelligence (AI) can quickly and accurately sift through breast MRIs in women with dense breasts to eliminate those without cancer, freeing up radiologists to focus on more complex cases, according to a study published in Radiology
Mammography has helped reduce deaths from breast cancer by providing early detection when the cancer is most treatable. However, it is less sensitive in women with extremely dense breasts than in women with fatty breasts. In addition, women with extremely dense breasts have a three- to six-times higher risk of developing breast cancer than women with almost entirely fatty breasts and a twofold higher risk than the average woman.
Supplemental screening in women with extremely dense breasts increases the sensitivity of cancer detection. Research from the Dense Tissue and Early Breast Neoplasm Screening (DENSE) Trial, a large study based in the Netherlands, supported the use of supplemental screening with MRI.
“The DENSE trial showed that additional MRI screening for women with extremely dense breasts was beneficial,” said study lead author Erik Verburg, M.Sc., from the Image Sciences Institute at the University Medical Center Utrecht in the Netherlands. “On the other hand, the DENSE trial confirmed that the vast majority of screened women do not have any suspicious findings on MRI.”
Since most MRIs show normal anatomical and physiological variation that may not require radiological review, ways to triage these normal MRIs to reduce radiologist workload are needed.
In the first study of its kind, Verburg and colleagues set out to determine the feasibility of an automated triaging method based on deep learning, a sophisticated type of AI. They used breast MRI data from the DENSE trial to develop and train the deep learning model to distinguish between breasts with and without lesions. The model was trained on data from seven hospitals and tested on data from an eighth hospital.
More than 4,500 MRI datasets of extremely dense breasts were included. Of the 9,162 breasts, 838 had at least one lesion, of which 77 were malignant, and 8,324 had no lesions.
The deep learning model considered 90.7% of the MRIs with lesions to be non-normal and triaged them to radiological review. It dismissed about 40% of the lesion-free MRIs without missing any cancers.
“We showed that it is possible to safely use artificial intelligence to dismiss breast screening MRIs without missing any malignant disease,” Verburg said. “The results were better than expected. Forty percent is a good start. However, we have still 60% to improve.”
The AI-based triaging system has the potential to significantly reduce radiologist workload, Verburg said. In the Netherlands alone, nearly 82,000 women may be eligible for biennial MRI breast screening based on breast density.
“The approach can first be used to assist radiologists to reduce overall reading time,” Verburg said. “Consequently, more time could become available to focus on the really complex breast MRI examinations.”
The researchers plan to validate the model in other datasets and deploy it in subsequent screening rounds of the DENSE trial.
“Deep Learning for Automated Triaging of 4581 breast MRI Examinations from the DENSE Trial.” Collaborating with Erik Verburg were Carla H. van Gils, Ph.D., Bas H.M. van der Velden, Ph.D., Marije F. Bakker, Ph.D., Ruud M. Pijnappel, M.D., Ph.D., Wouter B. Veldhuis, M.D., Ph.D., and Kenneth G. A. Gilhuijs, Ph.D.
Radiology is edited by David >A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast imaging, visit RadiologyInfo.org.
Images (JPG, TIF):
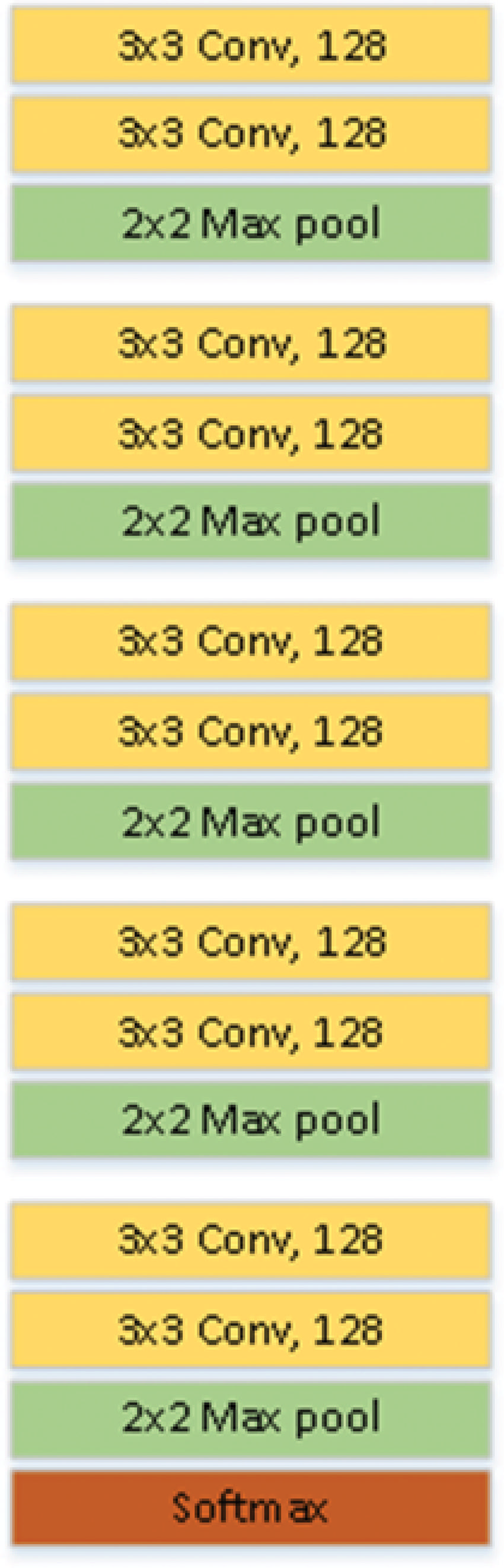
Figure 1. Schematic illustration of model architecture. Convolutional layers are indicated by “Conv,” and the final layer is the softmax activation function.
High-res (TIF) version
(Right-click and Save As)
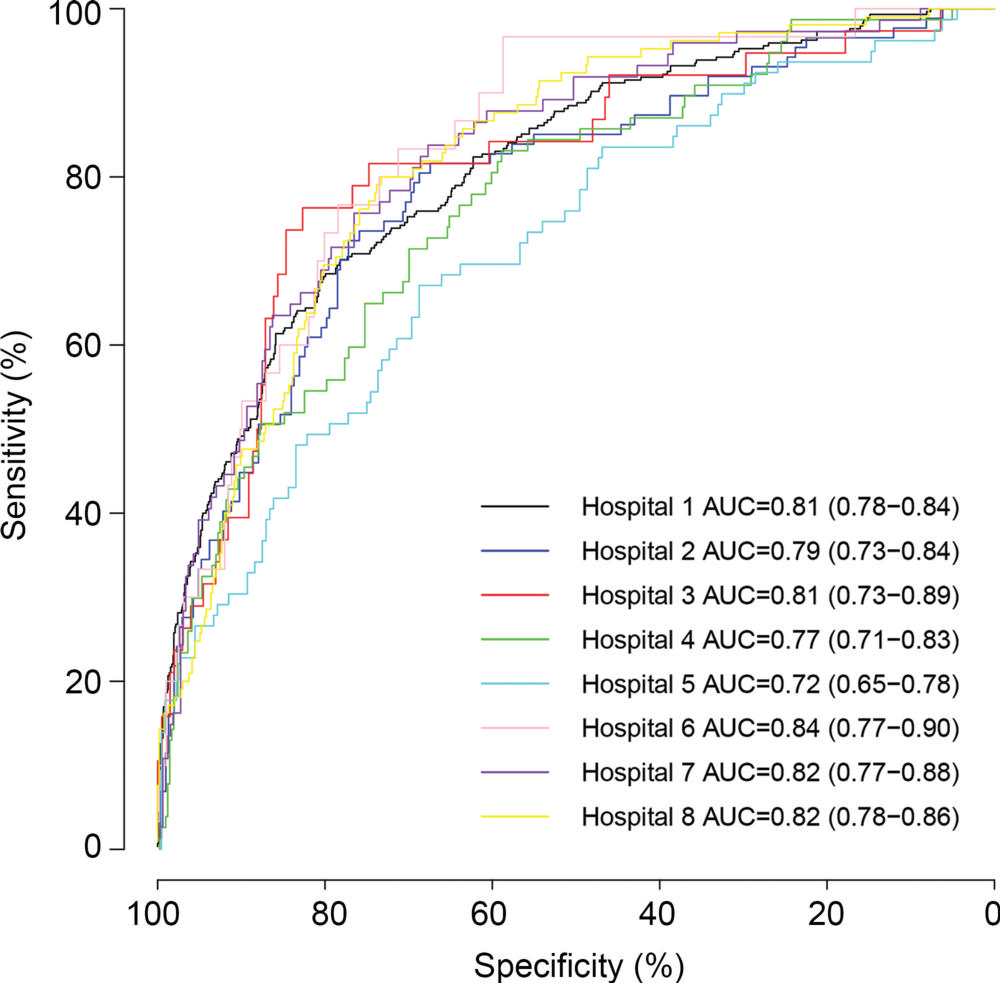
Figure 2. Receiver operating characteristics curves of data sets from eight hospitals. Each curve is the result of testing on one of the participating hospitals in the Dense Tissue and Early Breast Neoplasm Screening, or DENSE, trial using internal-external validation. Curves show the sensitivity and specificity of the method in the differentiation between MRI scans with lesions and those without lesions. Numbers in parentheses are the 95% CI. AUC = area under the receiver operating characteristic curve.
High-res (TIF) version
(Right-click and Save As)
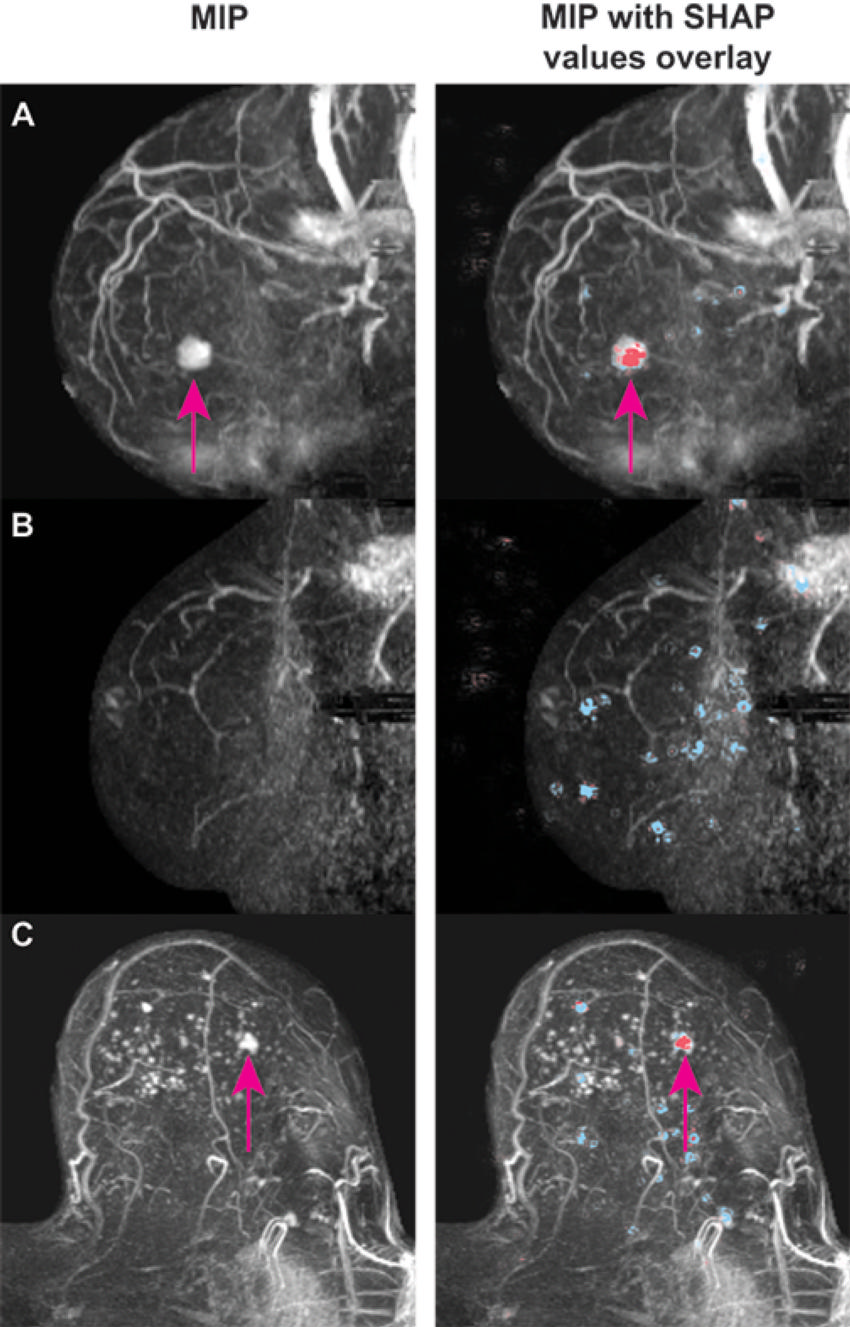
Figure 3. Examples of deep Shapley additive explanations (SHAP) overlay images. Maximum intensity projection (MIP) images are on left, and MIP images with the SHAP overlay are on right. Positive SHAP values (red) show areas that contribute to a high probability of lesion presence, negative SHAP values (blue) show locations with reduced probability. (A) Sagittal MIP images of contrast-enhanced breast MRI scan of an invasive ductal carcinoma in a 57-year-old woman with Breast Imaging Reporting and Data System (BI-RADS) category 4. The deep learning (DL) model yielded a probability of lesion presence of 90%. Positive SHAP values (red) are shown to coincide with the location of the lesion (arrows). (B) Sagittal MIP images of contrast-enhanced breast MRI scan of a breast without lesions in a 53-year-old woman with BI-RADS 1 score. The DL model yielded a probability of lesion presence of 11%. Negative SHAP values (blue) are diffusely distributed in the breast region. (C) Transverse MIP images of contrast-enhanced breast MRI scan of a ductal carcinoma in situ in a 65-year-old woman with BI-RADS 4 score. The DL model yielded a probability of lesion presence of 32%—the lowest probability value among all breasts with malignant disease in our study. Positive SHAP values (red) are shown to coincide with the location of the lesion (arrows).
High-res (TIF) version
(Right-click and Save As)