Prediction Models May Reduce False-Positives in MRI Breast Cancer Screening
Released: August 17, 2021
At A Glance
- Prediction models may help reduce the false-positive rate in women being screened for breast cancer with MRI.
- Researchers combined clinical characteristics—like body mass index and family history of breast cancer—and MRI findings to create the models.
- The prediction model could have prevented 45.5% of false-positive recalls and 21.3% of benign biopsies, without missing any cancers.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Katherine Anderson
1-630-491-1009
kanderson@rsna.org
OAK BROOK, Ill. — Prediction models based on clinical characteristics and imaging findings may help reduce the false-positive rate in women with dense breasts who undergo supplemental breast cancer screening with MRI, according to a new study in the journal Radiology.
Women with dense breast tissue have a much higher risk of breast cancer compared to those with average breast density. High breast density also markedly reduces the sensitivity of mammography due to the masking effect of the fibroglandular tissue, meaning that cancers can be hidden within dense breast tissue.
For these reasons, breast MRI is considered a potentially useful supplement to mammography screening in women with dense breast tissue. It is the most sensitive imaging technique for diagnosing breast cancer and can differentiate well between lesions and abnormalities of the breast. Research has confirmed its substantial added value as a screening tool for women at high risk of breast cancer.
However, the high sensitivity that makes MRI an excellent screening tool also means it often detects benign lesions that otherwise would have gone unnoticed. Women who get recalled for additional work-up based on these findings potentially face repeat MRI scans, targeted ultrasound and biopsy. The need for additional investigations may cause anxiety in the patient, increase health care costs or lead to biopsy-related complications.
"The reduction of the false-positive recall rate is an important issue when considering the use of breast MRI as a screening tool," said study lead author Bianca M. den Dekker, M.D., from the University Medical Center Utrecht in Utrecht, the Netherlands.
In the new study, Dr. den Dekker and colleagues developed prediction models to distinguish true-positive MRI screening from false-positives. To create the models, they combined MRI findings with clinical characteristics like body mass index, family history of breast cancer and use of hormone replacement therapy.
They used data from the Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial, which evaluated the effectiveness of screening with mammography plus MRI compared to mammography alone in Dutch breast cancer screening participants aged 50 to 75 years, with extremely dense breasts.
Of the 454 women who had a positive MRI result in a first supplemental MRI screening round, 79 were diagnosed with breast cancer, meaning that 375 women had false-positive MRI examinations. The full prediction model, based on all collected clinical characteristics and MRI findings, could have prevented 45.5% of false-positive recalls and 21.3% of benign biopsies, without missing any cancers. The model solely based on readily available MRI findings and age had a comparable performance and could have prevented 35.5% of false-positive MRI screenings and 13.0% of benign biopsies.
"Our prediction models may identify a substantial number of false-positives after first-round supplemental MRI screenings, reducing false-positive recalls and benign biopsies without missing any cancers," Dr. den Dekker said. "This brings supplemental screening MRI for women with dense breasts one step closer to implementation."
The researchers intend to perform validation studies using data from different populations. They also want to study the performance of prediction models in subsequent screening rounds. Dr. den Dekker noted that the false-positive rate in the study group fell from 79.8 per 1,000 screenings in the first round to 26.3 per 1,000 in the second.
"This can be partly explained by the availability of prior MRI examinations, which allows comparison for interval change," she said. "As incident screening rounds have a much lower false-positive rate, separate models may have to be created."
"Reducing False-Positive Screening MRI Rate in Women with Extremely Dense Breasts Using Prediction Models Based on Data from the DENSE Trial." Collaborating with Dr. den Dekker were Marije F. Bakker, Ph.D., Stéphanie V. de Lange, M.D., Ph.D., Wouter B. Veldhuis, M.D., Ph.D., Paul J. van Diest, M.D., Ph.D., Katya M. Duvivier, M.D., Marc B.I. Lobbes, M.D., Ph.D., Claudette E. Loo, M.D., Ph.D., Ritse M. Mann, M.D., Ph.D., Evelyn M. Monninkhof, Ph.D., Jeroen Veltman, M.D., Ph.D., Ruud M. Pijnappel, M.D., Ph.D., and Carla H. van Gils, Ph.D., for the DENSE trial study group.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on breast cancer screening, visit RadiologyInfo.org.
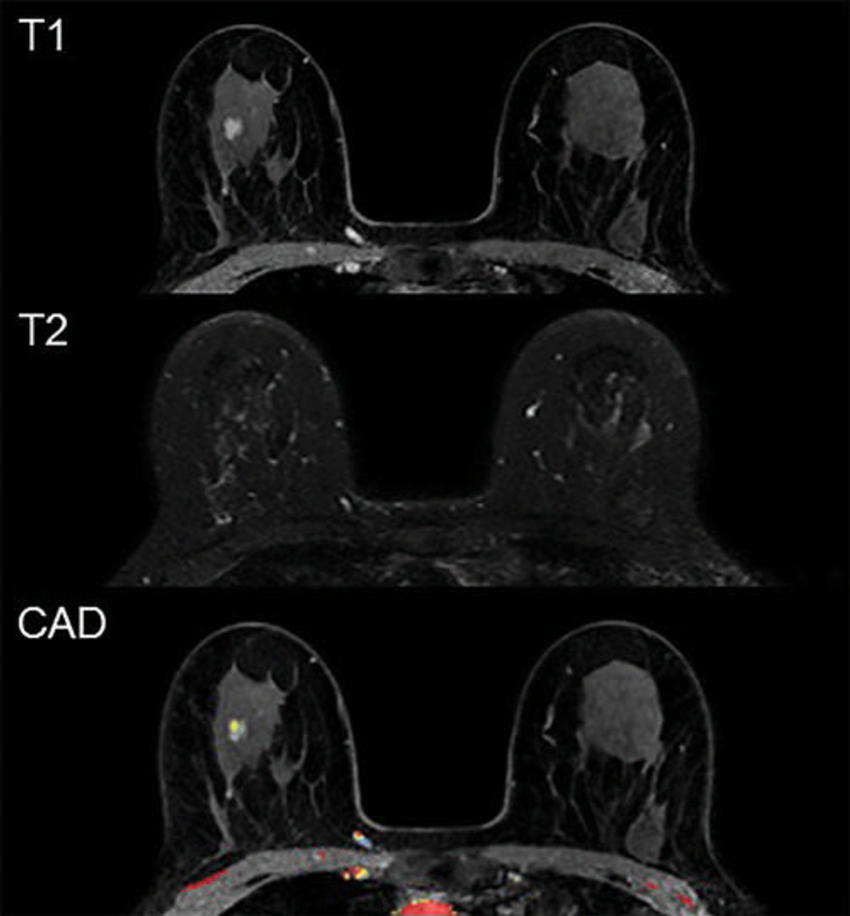
Figure 1. Example of a false-positive MRI. In a 59-year-old participant, first-round screening MRI showed an 8-mm irregular mass in the right breast. The lesion shows rapid heterogeneous type 2 enhancement, low T2 signal intensity, and no evident diffusion restriction. Histopathologic findings showed sclerotic stroma and apocrine metaplasia.
High-res (TIF) version
(Right-click and Save As)
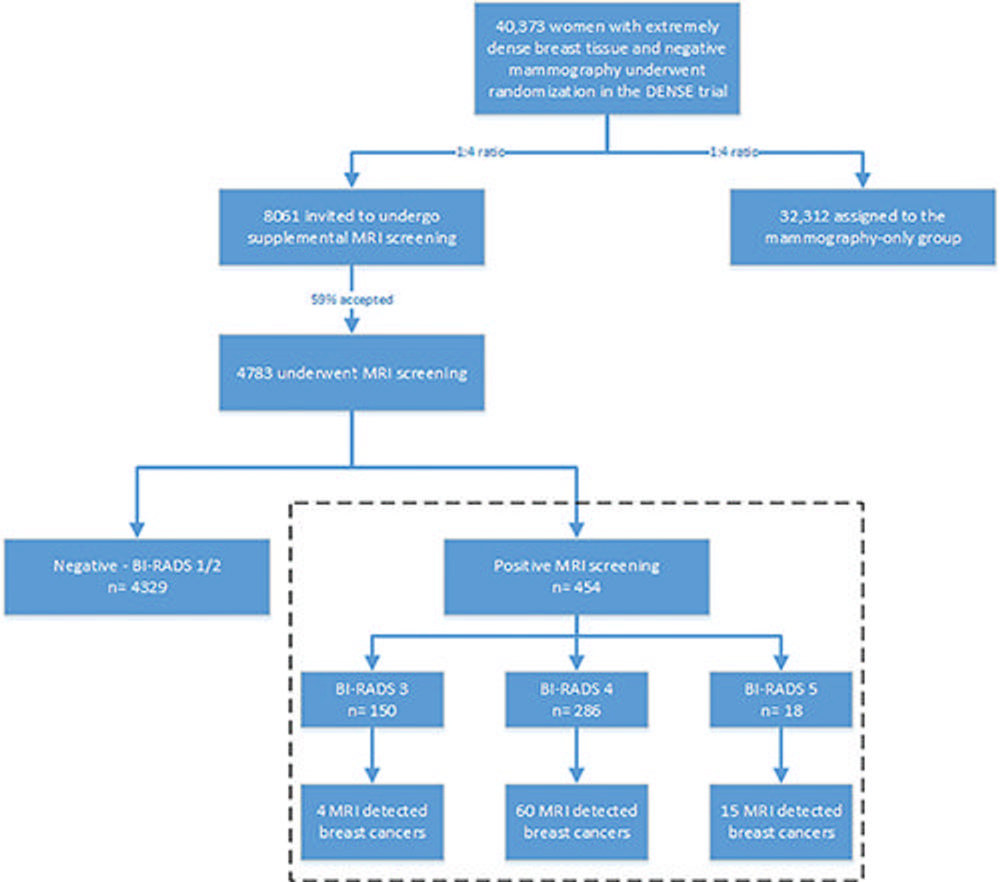
Figure 2. Flowchart shows enrollment in the Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial and selection of participants for the present analysis. Breast cancer screening participants (aged 50–75 years) with extremely dense breast tissue were assigned in a 1:4 ratio to a group that was invited to undergo supplemental MRI screening or to a group that underwent mammographic screening only. Approximately 59% of the participants in the MRI-invitation group actually underwent MRI. A total of 454 participants had a positive MRI screening result and constituted the study sample for the present analysis (dashed box).
High-res (TIF) version
(Right-click and Save As)
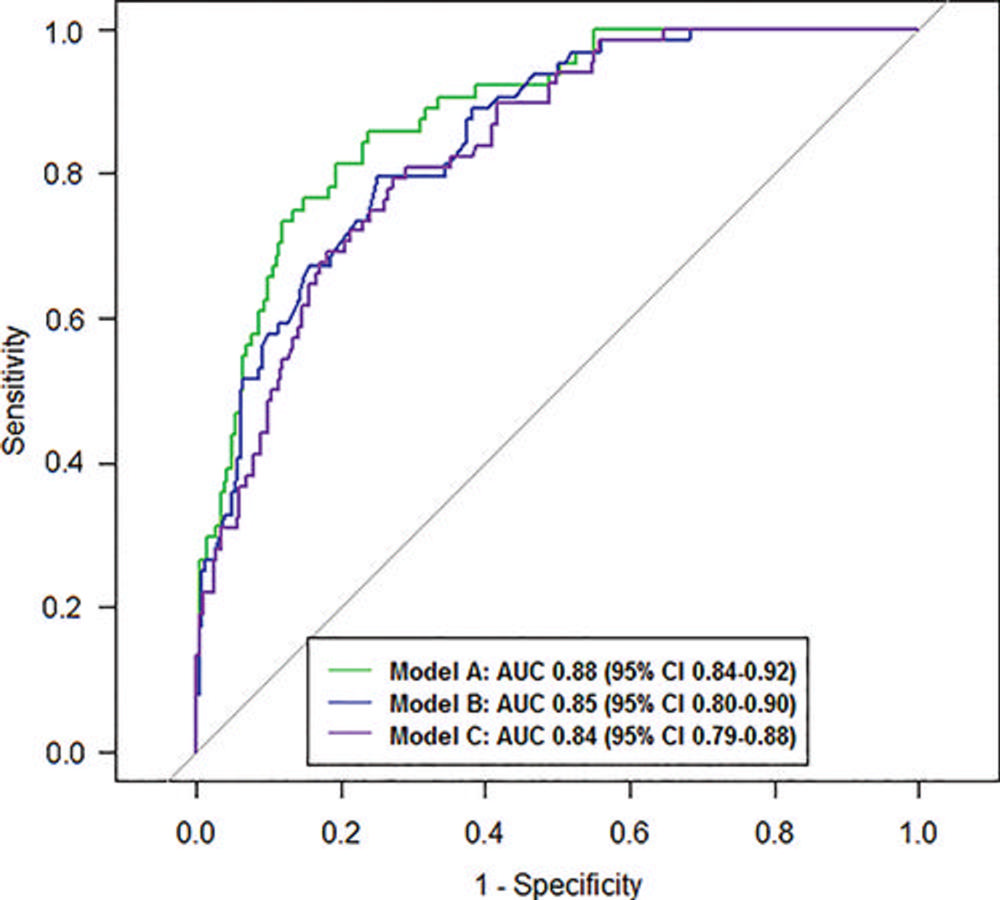
Figure 3. Graph shows areas under the receiver operating characteristic curves (AUCs) of three prediction models for true-positive MRI screening. Model A (green): The full model, including all clinical characteristics and MRI findings based on 328 participants. Model B (blue): The reduced model, including the variables age, menopausal status, number of first-degree relatives with breast cancer, history of breast biopsy, MRI Breast Imaging Reporting and Data System classification, and initial phase kinetics. Model C (purple): The model based on readily available data, including all MRI findings based on 369 participants.
High-res (TIF) version
(Right-click and Save As)
