COVID-19 Linked to Potentially Dangerous Eye Abnormalities
Released: February 16, 2021
At A Glance
- Researchers have found significant abnormalities in the eyes of some people with severe COVID-19.
- Of 129 COVID-19 patients in the study, nine had nodules in the macular region, the area in the back of the eye responsible for our central vision, with eight of them having nodules in both eyes.
- This is the first time these findings have been described using MRI.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Katherine Anderson
1-630-491-1009
kanderson@rsna.org
OAK BROOK, Ill. — Researchers using MRI have found significant abnormalities in the eyes of some people with severe COVID-19, according to a study published in the journal Radiology. The study results support the need for eye screening in these patients to provide appropriate treatment and management of potentially severe ophthalmological manifestations of COVID-19.
The COVID-19 pandemic has affected more than 100 million people since it began early in 2020. While the virus primarily attacks the lungs, it has been linked with eye abnormalities like conjunctivitis, also known as pink eye, and retinopathy, a disease of the retina that can result in a loss of vision. Eye abnormalities visible on MRI exams have been reported but there is limited research on the nature and frequency of these abnormalities.
To find out more, the French Society of Neuroradiology (SFNR) initiated a study of 129 patients with severe COVID-19 who underwent brain MRI.
Of the 129 patients, nine (7%) had abnormal MRI findings of the globe, or eyeball. The MRI scans showed one or more nodules in the back part, or posterior pole, of the eyeball. Eight of the nine patients had spent time in the intensive care unit (ICU) for COVID-19.
“We showed that a few patients with severe COVID-19 from the French COVID-19 cohort had one or several nodules of the posterior pole of the globe,” said study lead author Augustin Lecler, M.D., Ph.D., associate professor at the University of Paris and neuroradiologist from the Department of Neuroradiology at the Foundation Adolphe de Rothschild Hospital in Paris. “This is the first time these findings have been described using MRI.”
All nine patients had nodules in the macular region, the area in the back of the eye responsible for our central vision. Eight had nodules in both eyes.
The results suggest that screening should be considered in all patients with severe COVID-19 to detect these nodules. In clinical practice, this screening could include dedicated exploration of the eyes with high-resolution MRI, the researchers said. Additional recommended exams include fundoscopy, which uses a magnifying lens and a light to check the back of the inside of the eye, and optical coherence tomography, a noninvasive test that provides a 3D picture of the structure of the eye.
Dr. Lecler noted that severe eye problems might largely go unnoticed in the clinic, as COVID-19 patients hospitalized in the ICU are often being treated for much more severe, life-threatening conditions.
“Our study advocates for screening of all patients hospitalized in the ICU for severe COVID-19,” Dr. Lecler said. “We believe those patients should receive specific eye-protective treatments.”
The mechanism behind nodule formation remains unknown, the researchers said, although it could be related to inflammation triggered by the virus. Inadequate drainage of the veins of the eyes, a problem found in patients who spend time in the ICU in the prone position or intubated, may also be a factor. Seven of the nine patients with eye abnormalities in the study had been placed in a prone position in the ICU for an extended time.
The researchers are performing follow-up clinical and MRI examinations in the survivors to monitor the nodules and see if they carry any clinical consequences such as vision loss or visual field impairment.
They are also performing MRI examinations in new patients with severe COVID-19 from the second and third waves of the pandemic, using more comprehensive ophthalmological tests to correlate with the MRI results.
The effects on patients with moderate COVID-19 are currently under investigation.
“We have launched a prospective study with dedicated high-resolution MR images for exploring the eye and orbit in patients with light to moderate COVID,” Dr. Lecler said. “Therefore, we will be able to know whether our findings were specific to severe COVID patients or not.”
The findings support previous research that showed COVID-19 exacts a greater toll in people with existing health problems. Of the nine patients with eye nodules, two had diabetes, six were obese and two had hypertension.
“Ocular MRI Findings in Patients with Severe COVID-19: A Retrospective Multicenter Observational Study.” Collaborating with Dr. Lecler were François Cotton, M.D., Ph.D., François Lersy, M.D., Stéphane Kremer, M.D., Ph.D., and Françoise Héran, M.D., on behalf of the SFNR’s COVID study group.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on MRI, visit RadiologyInfo.org.
Images (JPG, TIF):
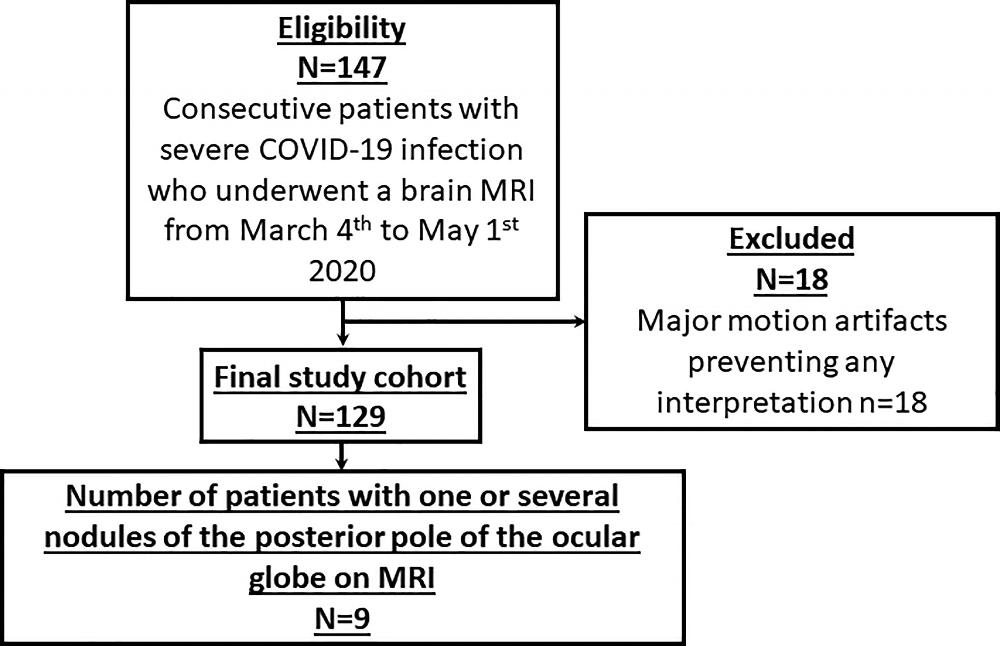
Figure 1. Flow chart. MRI=Magnetic Resonance Imaging.
High-res (TIF) version
(Right-click and Save As)
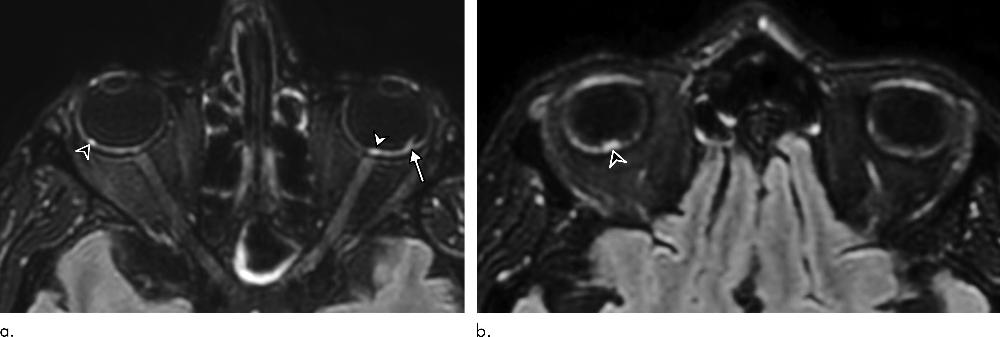
Figure 2. 56-year-old man presenting with severe COVID-19. Diagnosis of SARS-CoV-2 infection was based on a positive quantitative real-time RT-PCR test for SARS-CoV-2 nucleic acid performed on nasopharyngeal and lower respiratory tract swabs. The patient had been hospitalized in intensive care unit for 20 days when an MRI was performed due to delayed awakening despite discontinuation of sedation. He presented with acute respiratory distress syndrome, with a median Simplified Acute Physiology Score (SAPS II) of 45. He was intubated on high-flow supplementary oxygen and placed in the prone position. A, B, 3D FLAIR-weighted MRI reformatted in the axial plane showing several hyperintense nodules of the posterior pole of the globe located in the macular region (white arrowhead) and the extramacular region (black arrowheads). Note the presence of a focal temporal retinal detachment of the left eye (arrow).
High-res (TIF) version
(Right-click and Save As)
