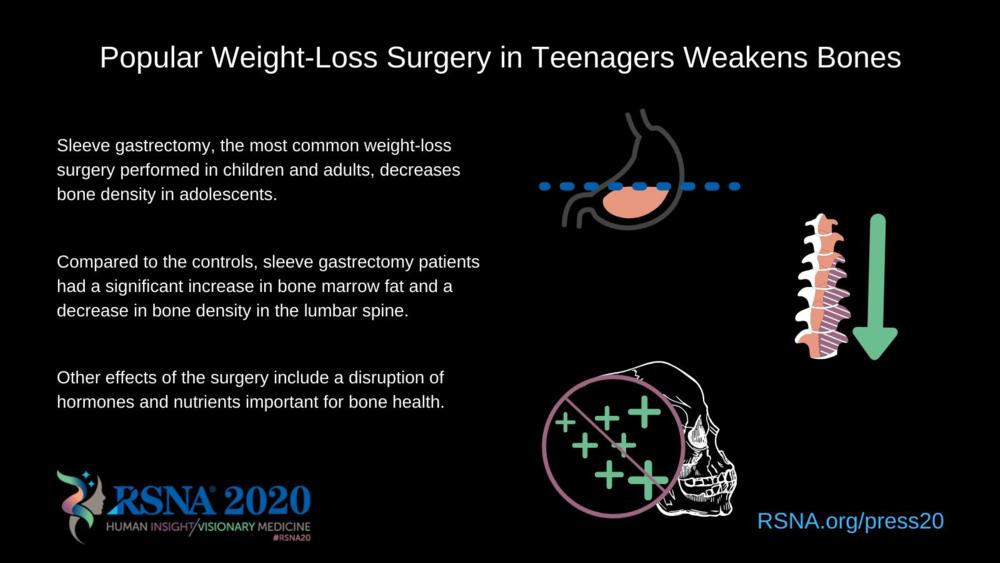
Popular Weight-Loss Surgery in Teenagers Weakens Bones
Released: November 24, 2020
At A Glance
- Sleeve gastrectomy, the most common weight-loss surgery performed in children and adults, decreases bone density in adolescents.
- Compared to the controls, sleeve gastrectomy patients had a significant increase in bone marrow fat and a decrease in bone density in the lumbar spine.
- Other effects of the surgery include a disruption of hormones and nutrients important for bone health.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — A common weight loss surgery for adolescents with obesity called sleeve gastrectomy has harmful effects on bones, according to a study being presented at the annual meeting of the Radiological Society of North America (RSNA).
“Childhood obesity is a major public health issue that has increased over the last 10 years,” said lead investigator Miriam A. Bredella, M.D., professor of radiology at Harvard Medical School in Boston, Massachusetts, and vice chair of the Department of Radiology at Massachusetts General Hospital in Boston. “Sleeve gastrectomy is the most common bariatric surgery procedure performed in children and adults.”
In a sleeve gastrectomy, approximately 75% of the stomach is removed to restrict food intake and induce weight loss. It results in a typically round stomach taking on the shape of a tube or sleeve. The number of sleeve gastrectomy procedures performed on adolescents increased 100-fold from 2005 to 2014.
“In adults, bariatric surgery can have long-term effects on bone, leading to higher fracture risk,” Dr. Bredella said. “We wanted to determine the effects of sleeve gastrectomy performed on adolescents during the crucial years when bone mass is being accrued.”
The study examined 52 adolescents with moderate to severe obesity, 26 of whom underwent sleeve gastrectomy. The other 26 were in the control group. Mean age was 17.5 years, and mean body mass index (BMI) was 45. BMI of 30 or above is considered obese. Thirty-eight of study participants were girls. Before and 12 months after sleeve gastrectomy (or no surgery), the patients underwent quantitative CT of the lumbar spine, to quantify volumetric bone mineral density. Quantitative CT is a highly accurate technique for detecting changes in volumetric bone mineral density after extreme weight loss.
Recent studies have shown that bone marrow fat responds to changes in nutrition and may serve as a biomarker for bone quality. Therefore, patients underwent proton MR spectroscopy to quantify bone marrow fat of the lumbar spine.
One year following surgery, the adolescents who underwent sleeve gastrectomy lost 34 (+/-13) kg, or 75 (+/-28) pounds, while there was no significant change in weight in the control group. Compared to the controls, sleeve gastrectomy patients had a significant increase in bone marrow fat and a decrease in bone density in the lumbar spine.
“Adolescents who underwent sleeve gastrectomy had bone loss and an increase in bone marrow fat, despite marked loss of body fat,” Dr. Bredella said. “While weight-loss surgery is successful for weight loss and improving metabolic disorders, it has negative effects on bone.”
Dr. Bredella said the loss of bone density following sleeve gastrectomy was expected because greater weight-bearing strengthens bones. In addition to a loss of bone density, other effects of weight-loss surgery include a disruption of hormones and nutrients important for bone health.
“We need to identify mechanisms that will help prevent bone loss in these patients and to make adolescents with obesity more aware of bone health,” she said. “Adolescence is the critical time for bone mass accrual, and any process that interferes with bone accrual during this time can have dire consequences later in life.”
Co-authors are Vibha Singhal, M.D., Nazanin Hazhir Karzar, M.D., Abisayo Animashaun, B.S., Amita Bose, B.S., and Madhusmita Misra, M.D., M.P.H.
For more information and images, visit RSNA.org/press20. Press account required to view embargoed materials.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
Editor’s note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA media relations team at Newsroom at 1-630-590-7762.
For patient-friendly information on bone scans, visit RadiologyInfo.org.
Video (MP4):
Video 2. Dr. Miriam Bredella discusses the results of her research.
Download MP4
(Right-click and Save As)
Video 3. Dr. Miriam Bredella gives background to her research.
Download MP4
(Right-click and Save As)
Images (JPG, TIF):
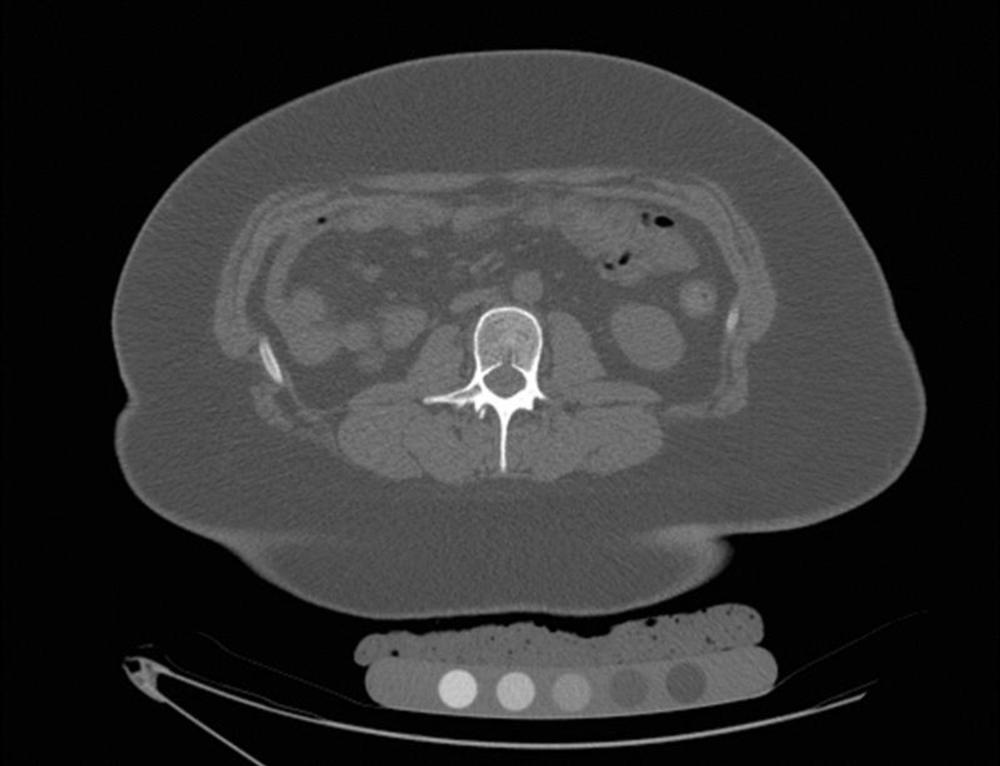
Figure 1. CT in a 17-year-old female prior to sleeve gastrectomy. Volumetric bone mineral density pre-surgery was 183 mg/cm3.
High-res (TIF) version
(Right-click and Save As)
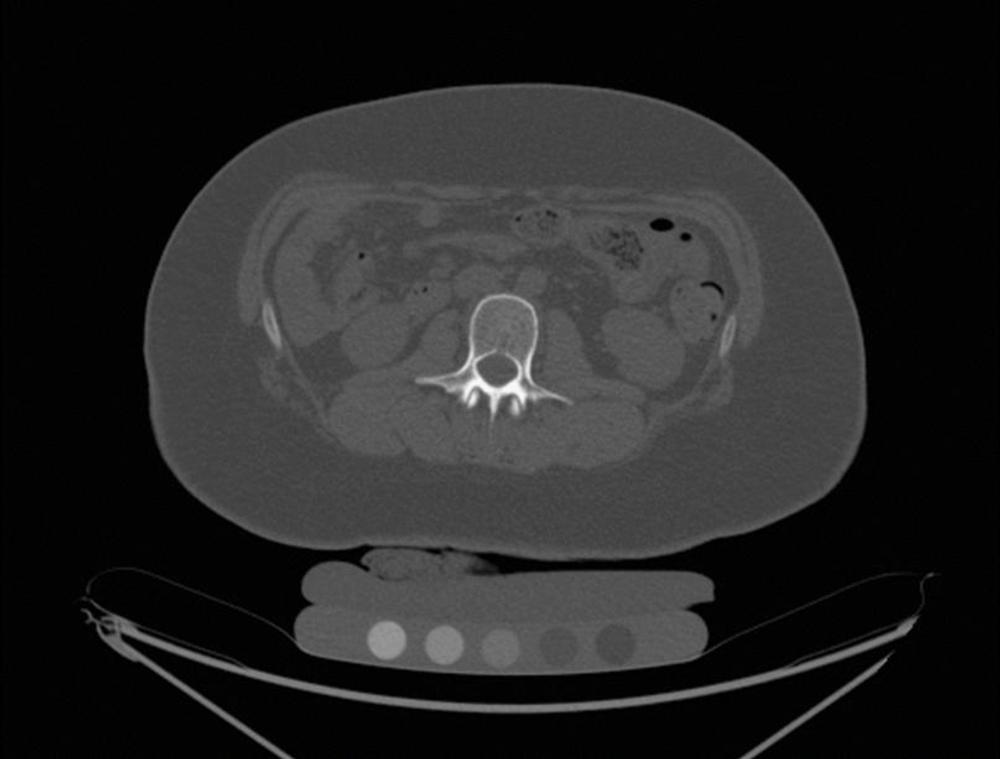
Figure 2. Children lost bone mineral density one year after sleeve gastrectomy. CT in a 17-year-old female one year after surgery. Volumetric bone mineral density post-surgery was 146 mg/cm3 from 183 mg/cm3.
High-res (TIF) version
(Right-click and Save As)
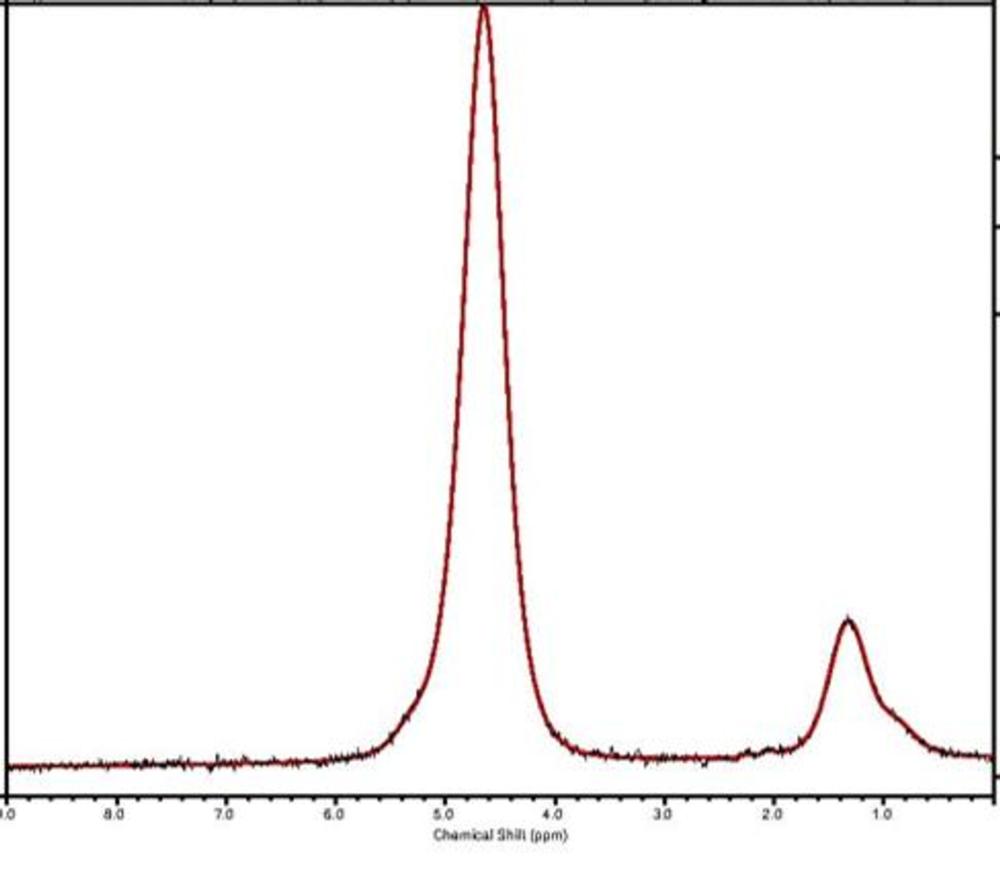
Figure 3. Results from MR spectroscopy of the first lumbar vertebral body in an 18-year-old female prior to sleeve gastrectomy showing marrow fat. Pre-surgery: marrow fat 0.20 lipid to water ratio.
High-res (TIF) version
(Right-click and Save As)
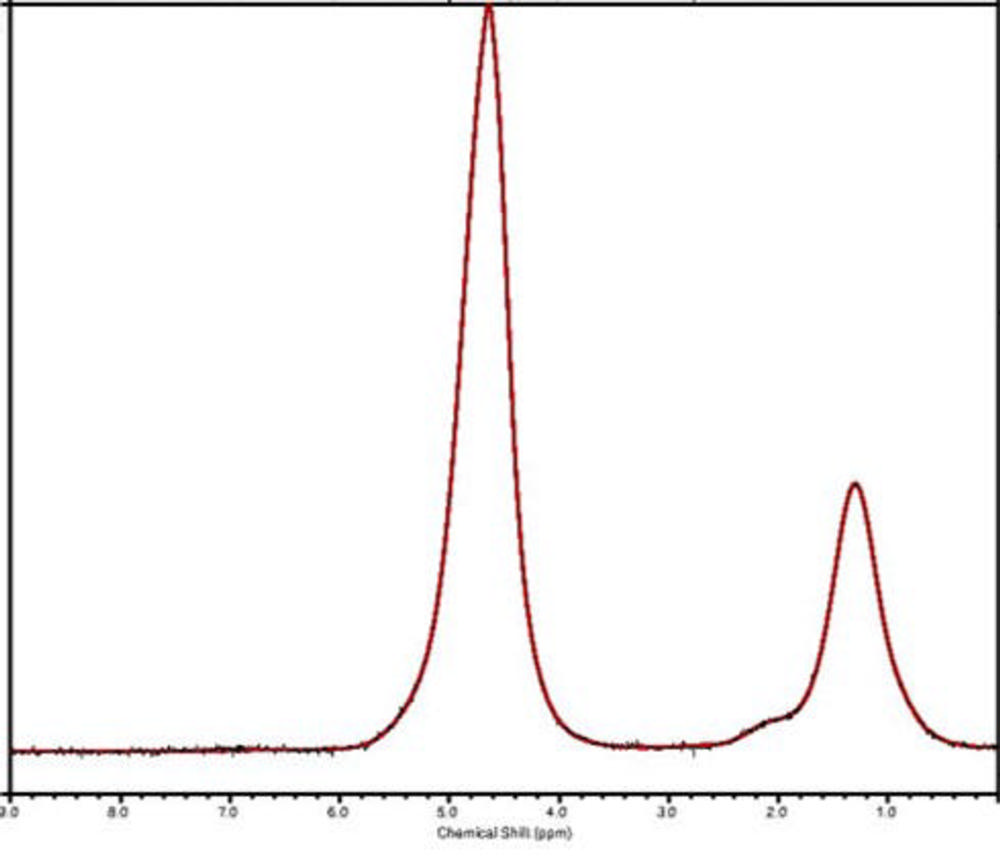
Figure 4. Results from MR spectroscopy of the first lumbar vertebral body in an 18-year-old female one year after sleeve gastrectomy showing marrow fat. Post-surgery: marrow fat 0.41 lipid to water ratio.
High-res (TIF) version
(Right-click and Save As)
Powerpoint: