Dangerous Blood Clots Form in Leg Arteries of COVID-19 Patients
Released: July 16, 2020
At A Glance
- Arterial thrombosis—life-threatening blood clots in the arteries of the legs—is associated with COVID-19.
- Blood clots in the legs of COVID-19 patients were significantly larger and of greater frequency than those found in controls.
- Arterial thrombosis associated with COVID-19 was characterized by strikingly increased rates of amputation and death.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. (July 16, 2020) — COVID-19 is associated with life-threatening blood clots in the arteries of the legs, according to a study published in Radiology. Researchers said COVID-19 patients with symptoms of inadequate blood supply to the lower extremities tend to have larger clots and a significantly higher rate of amputation and death than uninfected people with the same condition.
COVID-19’s association with blood clots in the pulmonary arteries is well-established. Less is known about the virus’ connection to lower extremity arterial thrombosis, a condition characterized by blood clots in the arteries that impede the flow of oxygenated blood to the lower extremities.
During the peak of the COVID-19 pandemic in New York City, radiologists at the city’s Montefiore Medical Center observed an increase in patients testing positive for lower extremity arterial thrombosis on CT angiography exams. The patients had arrived at hospitals with coldness, pain or discoloration of their legs. Frequently these symptoms of leg ischemia, a condition in which blood flow to the lower extremities is restricted, were accompanied by respiratory distress, cough, fever and altered mental status.
The alarming trend prompted the researchers to look more closely at a possible connection between COVID-19 and lower extremity arterial thrombosis and whether people with the virus had a worse prognosis.
In March and April 2020, they identified 16 COVID-19-positive patients, average age 70, who underwent CT angiography of the lower extremities for symptoms of leg ischemia. These patients were compared with 32 COVID-19-negative patients, average age 71, who underwent CT angiography with similar symptoms in previous years and who were well matched with COVID-19 cohort for demographic and clinical characteristics.
All patients with COVID-19 infection undergoing lower extremity CT angiography had at least one clot in the leg, compared with only 69% of controls. The clots in the COVID-19 patients were significantly larger and affected arteries higher up in the leg with greater frequency than those in controls. Death or limb amputation was more common in the COVID-19 patients.
“We found that arterial thrombosis associated with COVID-19 infection was characterized by dire outcomes, namely strikingly increased rates of amputation and death, which in our series were 25% and 38%, respectively,” said study lead author Inessa A. Goldman, M.D., a radiologist at Montefiore and assistant professor at Albert Einstein College of Medicine in New York City. “For comparison, the rate of both amputation and death was only 3% among controls. It is unclear whether the patients’ concurrent COVID-19-related pneumonia, the virulence of the COVID-19-related clotting disorder or delayed initial arrival to the hospital contributed to these outcomes.”
COVID-19 patients presenting with symptoms of leg ischemia only were more likely to avoid amputation or death than patients who had symptoms of ischemia and systemic symptoms including cough, respiratory distress or failure, hypoxia, fever, or altered mental status.
“In our cohort none of the five patients presenting with complaints pertaining to leg symptoms only, such as pain or discoloration, without systemic symptoms sustained amputation or died,” Dr. Goldman said.
Dr. Goldman noted that with infection rates rising in many parts of the country, it is important that physicians be mindful of the connection between COVID-19 and lower extremity arterial thrombosis.
“Awareness of lower extremity arterial thrombosis as a possible complication of COVID-19 infection is important for all providers who take care of these patients, because early diagnosis is usually crucial for limb preservation in lower extremity ischemia,” she said.
COVID-19’s association with lower extremity arterial thrombosis is likely related to a combination of factors, Dr. Goldman said, including an increased tendency of the blood to clot, damage to the lining of the arteries, and immune reactions tied to the SARS-CoV-2 virus and COVID-19 infection.
“This continues to be an area of intense study around the world,” she said.
“Lower Extremity Arterial Thrombosis Associated with COVID-19 is Characterized by Greater Thrombus Burden and Increased Rate of Amputation and Death.” Collaborating with Dr. Goldman were Kenny Yee, Ph.D., and Meir H. Scheinfeld, M.D., Ph.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wis., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on CT angiography, visit RadiologyInfo.org.
Images (JPG, TIF):
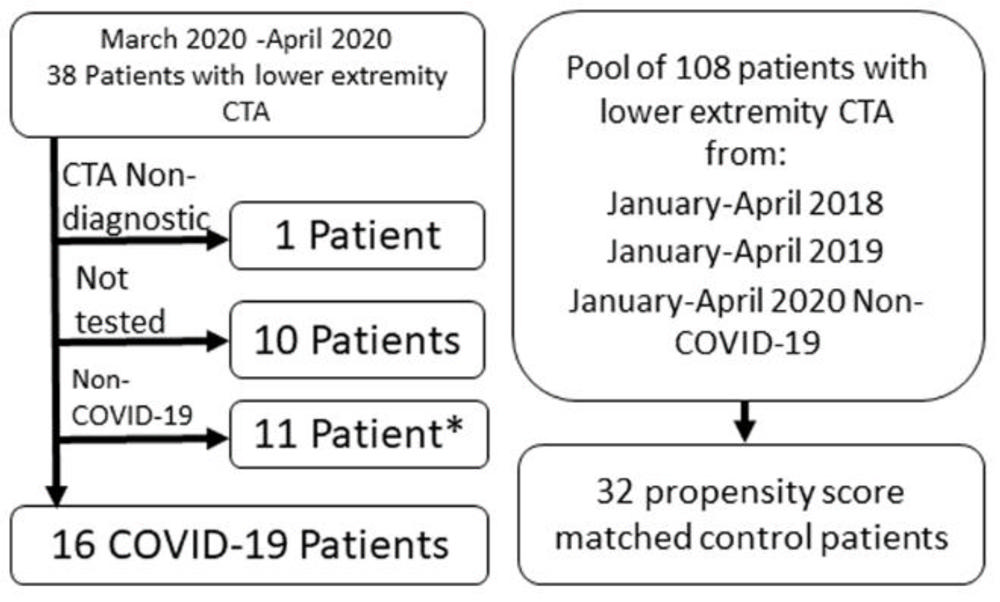
Figure 1. Patient flow for the study. Non-COVID-19 means that the patient tested negative for SARS CoV- 2. *Two of these patients which tested negative were used as controls as described in the methods section.
High-res (TIF) version
(Right-click and Save As)
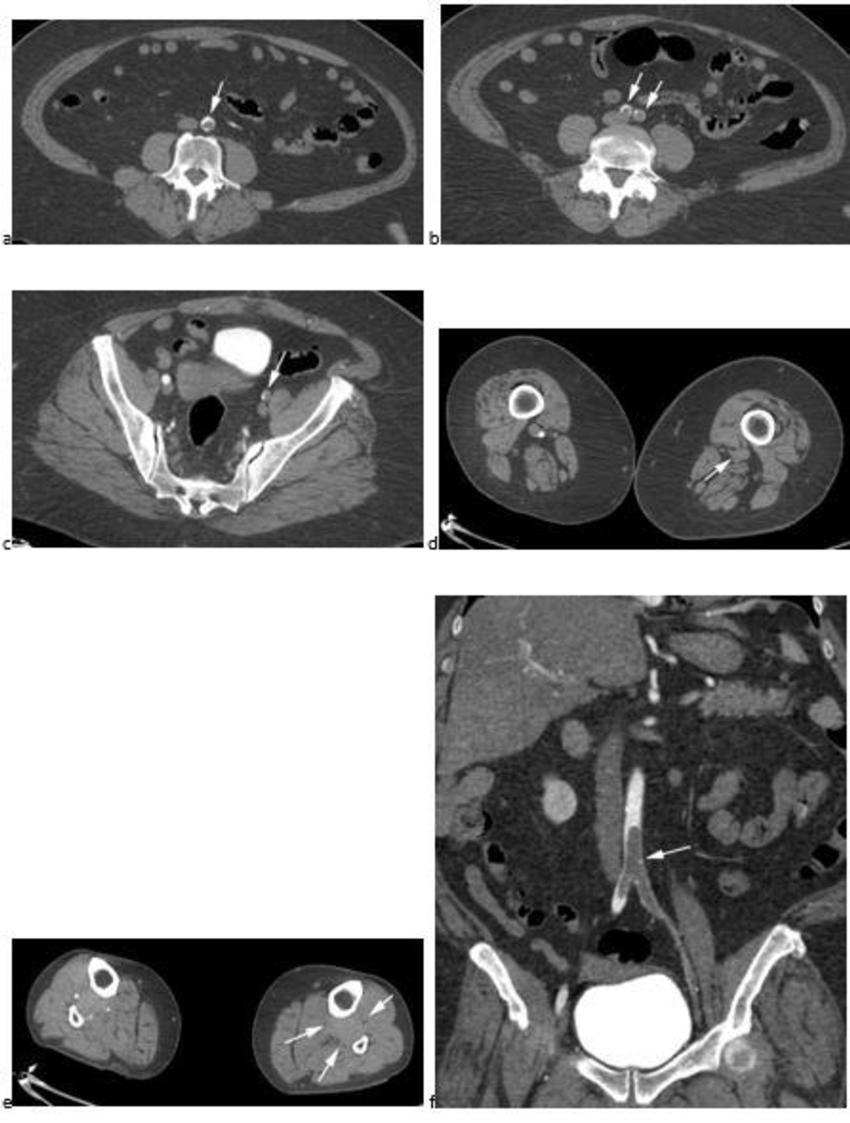
Figure 2. CTA images from a 63-year-old woman with COVID-19. Images through the (a) distal abdominal aorta, (b) proximal common iliac arteries, (c) external iliac arteries, (d) popliteal arteries, and (e) anterior tibial, posterior tibial, and peroneal arteries demonstrate lack of contrast opacification on the left (arrows). Hyperdensity along the periphery of the vessels in a and b corresponds to contrast rather than calcium. Note that the arrows in e point to the expected location of the vessels. (f) Oblique coronal reformatted CT image demonstrates clot at the aortic bifurcation (arrow).
High-res (TIF) version
(Right-click and Save As)
