New Study Looks at Post-COVID-19 Emerging Disease in Children
Released: June 24, 2020
At A Glance
- The study reports the spectrum of findings in children with multisystem inflammatory syndrome post-COVID-19.
- Clinical features of the syndrome are similar to atypical Kawasaki disease and toxic shock syndrome.
- Imaging findings include airway inflammation, pulmonary edema, coronary artery aneurysms and intra-abdominal inflammation.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. (June 25, 2020) – In recent weeks, a multisystem hyperinflammatory condition has emerged in children in association with prior exposure or infection to SARS-CoV-2. A new case series published in the journal Radiology examines the spectrum of imaging findings in children with the post-COVID-19 inflammatory condition known in the U.S. as Multisystem Inflammatory Syndrome in Children (MIS-C).
The array of findings includes airway inflammation and rapid development of pulmonary edema, coronary artery aneurysms, and extensive intra-abdominal inflammatory changes.
In April 2020, Evelina London Children’s Hospital in London, U.K., experienced a surge of children with a multi-system hyperinflammatory syndrome. The children had a variety of symptoms, including fever, headaches, abdominal pain, rash and conjunctivitis. Clinical features and lab findings shared some similarities to those of Kawasaki disease—which causes inflammation in the walls of blood vessels—Kawasaki-disease shock syndrome or toxic-shock syndrome, although atypical and more severe.
“Our hospital saw an unprecedented cluster of children presenting with MIS-C, a new hyperinflammatory syndrome in children related to the current COVID-19 pandemic—the recognition of which led to a national alert,” said the study’s lead author, Shema Hameed, M.B.B.S., consultant pediatric radiologist at Evelina London Children’s Hospital.
For the study, researchers performed a retrospective review of clinical, laboratory and imaging findings of the first 35 children under age 17 who were admitted to the pediatric hospital that met the case definition for MIS-C. The children were admitted from April 14 to May 9, 2020, and included 27 boys and eight girls, with a median age of 11 years old.
The most common clinical presentation was fever, found in 33 (94%) of the children, gastrointestinal symptoms including abdominal pain, vomiting and diarrhea in 30 (86%) of the children, rash (13 or 37%) and conjunctivitis (9 or 26%). Twenty-one children (60%) were in shock. Clinical status was severe enough to warrant management in the pediatric intensive care unit in 24 of 35 children (69%), of which 7 (20%) required mechanical ventilation and 20 (57%) inotropic support.
Two children required extracorporeal membrane oxygenation (ECMO) due to severe myocardial dysfunction. Lab tests revealed that all of the children had abnormal white blood cell counts.
The study identified a pattern of imaging findings in post COVID-19 MIS-C, including airway inflammation, rapidly progressive pulmonary edema, coronary artery aneurysms and extensive abdominal inflammatory changes within the right iliac fossa.
All 35 children underwent chest X-ray due to fever, sepsis or features of multisystem inflammation. Nineteen X-rays were abnormal, the most common finding being that of bronchial wall thickening.
The predominant findings on chest CT were basal consolidation, or part of the lung filling with fluid; and collapsed lung with pleural effusions, or build-up of fluid in the outer membranes of the lungs.
Abdominal ultrasound findings included inflammatory changes within the right iliac fossa, with mesenteric fat stranding, lymphadenopathy and bowel wall thickening, as well as free fluid in the pelvis.
“As pediatric radiologists, we were interested in the emerging pattern of imaging findings that we observed in these children,” Dr. Hameed said. “Our intention is to bring these findings to the attention of the wider radiological community.”
The authors advise that future studies should include a larger group of patients, ideally utilizing multi-center databases to assess the radiological findings alongside the complex clinical course of these young patients.
“Spectrum of Imaging Findings on Chest Radiograph, US, CT, and MRI Images in Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with COVID-19.” Collaborating with Dr. Hameed were Heba Elbaaly, Catriona E. L. Reid, Rui M. F. Santos, Vinay Shivamurthy, James Wong and K. Haran Jogeesvaran.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wis., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on pediatric imaging, visit RadiologyInfo.org.
Images (JPG, TIF):
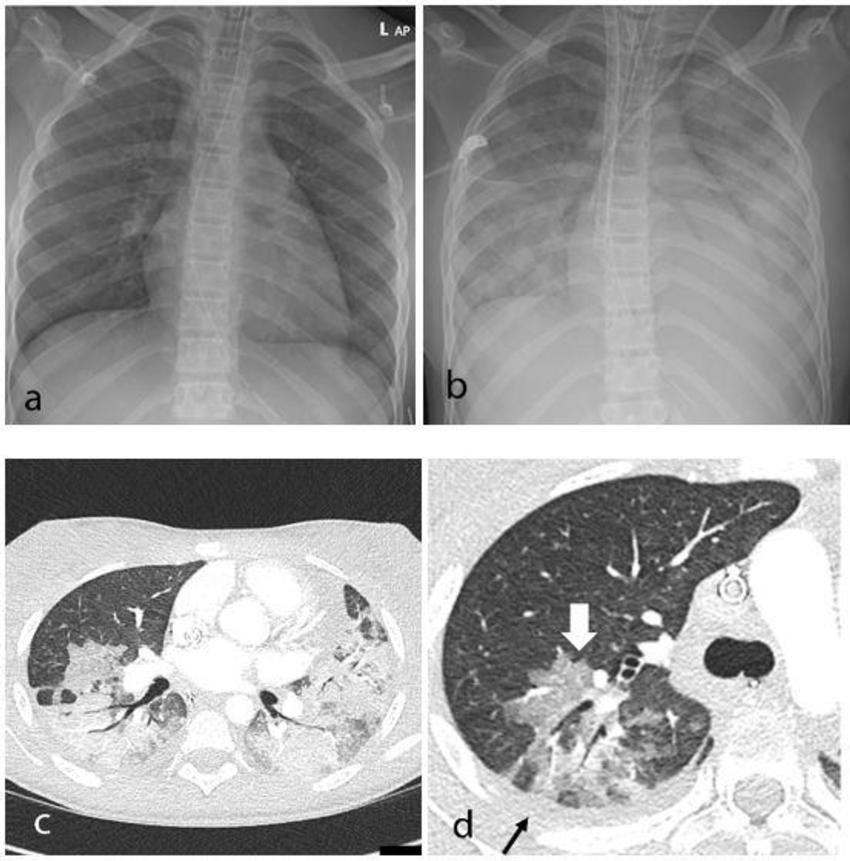
Figure 1. Thoracic findings in a 15-year-old girl with Multisystem Inflammatory Syndrome in Children (MIS-C). (a) Chest radiograph on admission shows mild perihilar bronchial wall cuffing. (b) Chest radiograph on the third day of admission demonstrates extensive airspace opacification with a mid and lower zone predominance. (c, d) Contrast-enhanced axial CT chest of the thorax at day 3 shows areas of ground-glass opacification (GGO) and dense airspace consolidation with air bronchograms. (c) This conformed to a mosaic pattern with a bronchocentric distribution to the GGO (white arrow, d) involving both central and peripheral lung parenchyma with pleural effusions (black small arrow, d).
High-res (TIF) version
(Right-click and Save As)
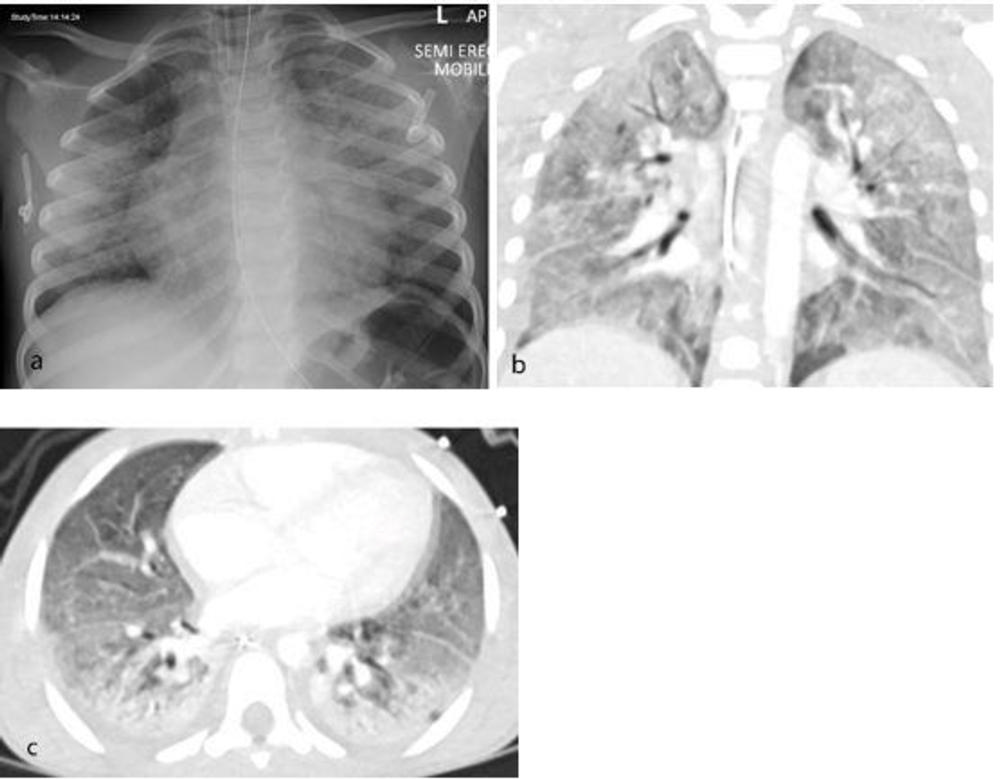
Figure 2. Thoracic findings in a 5-year-old boy with Multisystem Inflammatory Syndrome in Children (MIS-C). (a) Chest radiograph 4 days after admission shows perihilar bronchial wall cuffing and interstitial thickening with hazy surrounding airspace consolidation extending towards the peripheries. (b, c) Coronal and axial contrast-enhanced CT chest 1 day after the radiograph shows diffuse bilateral airspace consolidation with an anteroposterior gradient suggestive of acute respiratory distress syndrome (ARDS).
High-res (TIF) version
(Right-click and Save As)

Figure 3. Range of cardiothoracic imaging findings in Multisystem Inflammatory Syndrome in Children (MIS-C). (a) Chest radiograph and (b) axial contrast-enhanced CT chest of a 4-year-old male presenting with fever, rash, abdominal pain, and diarrhea show features of pulmonary edema including perihilar interstitial thickening (thin arrow, a), septal lines (thin arrows, b), and pleural effusions (wide arrow, b). Left lower lobe collapse and consolidation (wide arrow, a) was also confirmed on CT (b). (c) 8-year-old boy with MIS-C noted to have impaired cardiac function and coronary artery aneurysms on echocardiogram. Contrast-enhanced cardiac CT demonstrating an axial view of the left main stem (LMS) (dotted arrow) and left anterior descending (LAD) (solid arrow) coronary arteries. There is medium sized aneurysmal dilation of the LMS (5.0 x 5.1mm z-score +2) and a large aneurysm in the proximal LAD (6.5 x 7.7mm z-score +13.9).
High-res (TIF) version
(Right-click and Save As)
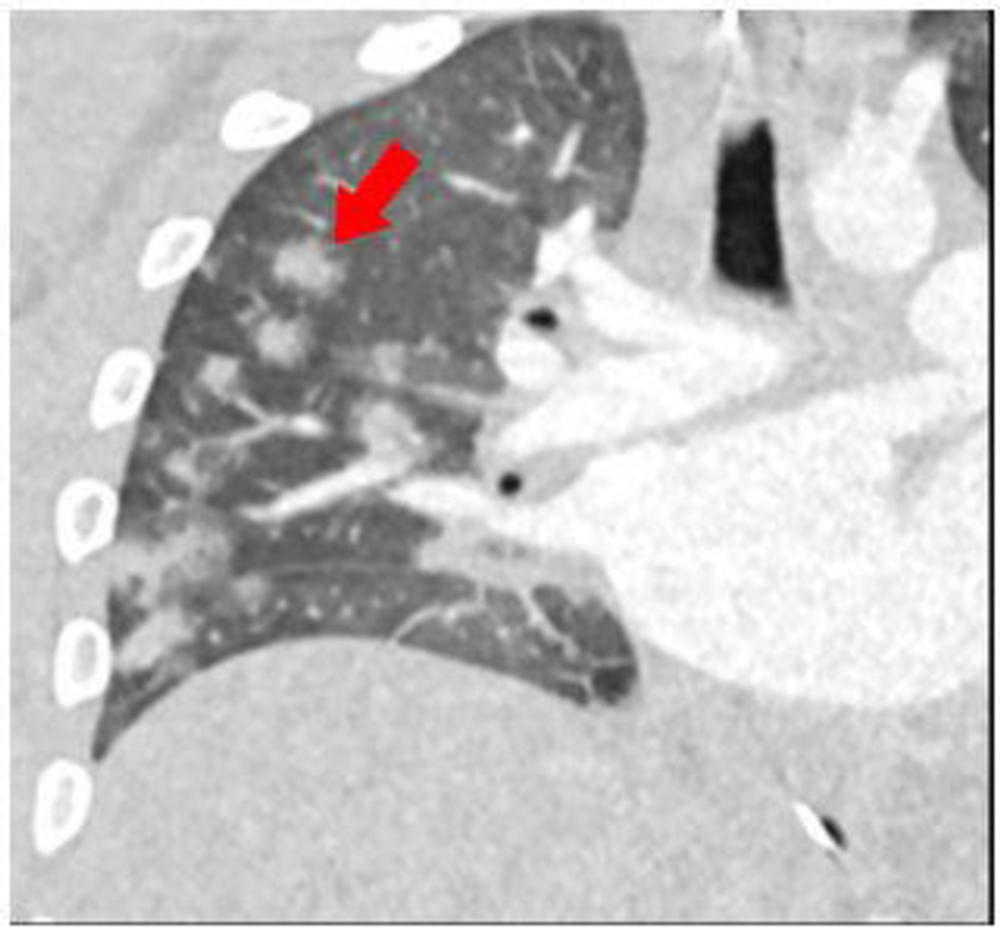
Figure 4. 15-year-old male presenting with fever, sepsis, and shock with impaired cardiac function. Coronal reconstruction of a contrast-enhanced CT chest shows multiple round consolidative foci with surrounding ground glass halos (red arrow).
High-res (TIF) version
(Right-click and Save As)
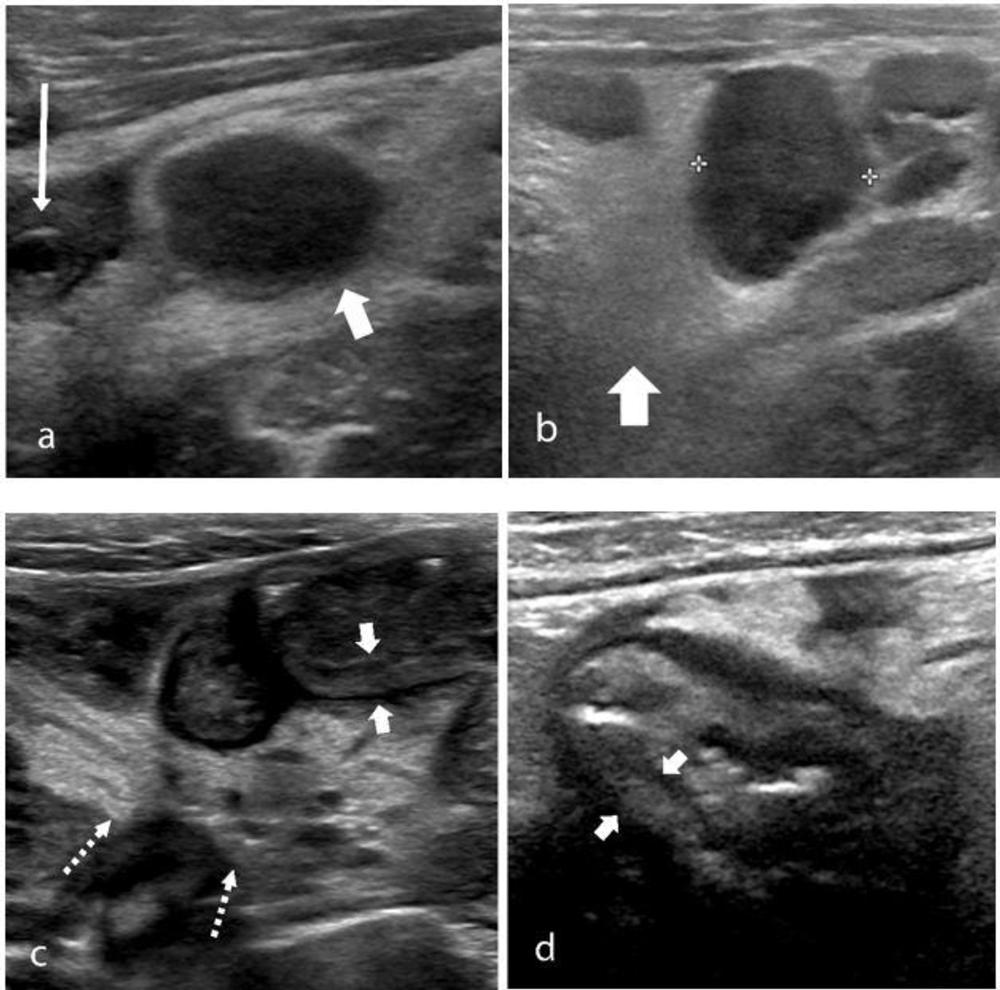
Figure 5. The ultrasound features of right iliac fossa inflammation in four children (a) 7-year-old boy with MIS-C and abdominal pain. High-frequency sonographic image depicts an enlarged mesenteric lymph node within the right iliac fossa (wide arrow), with associated hyperechoic mesenteric fat. The appendix is normal in diameter (thin arrow). (b) 15-year-old boy with MIS-C. Multiple mesenteric lymph nodes within the right iliac fossa, the short axis diameter of the largest lymph node measured 13mm (calipers), with associated hyperechoic mesenteric fat (arrow) were noted on US. (c) 9-year-old boy with MIS-C. US shows loops of thickened small bowel (between solid arrows) with associated hyperechoic mesenteric fat (dotted arrows). (d) 16-year-old boy with severe right iliac fossa pain. High-frequency sonogram shows marked cecal wall thickening (arrows).
High-res (TIF) version
(Right-click and Save As)

Figure 6. 15 year-old boy with MIS-C. US shows a well-defined subcapsular hypoechoic splenic lesion (arrow) felt to be likely an infarct as the clinical course did not conform with this being a splenic abscess, the main other differential diagnosis for this appearance.
High-res (TIF) version
(Right-click and Save As)

Figure 7. Contrast enhanced CT abdomen and pelvis of a 15-year-old male who presented with sepsis. (a) Coronal image of the abdomen demonstrates gallbladder wall edema (wide arrow). There is extensive thickening of the cecal wall thickening (thin arrow) and free-fluid within the pelvis (dotted arrow). (b) Axial slice through the lower abdomen showing the cecal wall thickening (wide arrow) with multiple adjacent mesenteric nodes (thin arrow) and surrounding fat-stranding. (c) Coronal image through the left upper quadrant shows a focal subcapsular, hypoattenuating region within the spleen in keeping with a splenic infarct (arrow).
High-res (TIF) version
(Right-click and Save As)
