Abnormal Imaging Findings Key to EVALI Diagnosis in Vapers
Released: January 28, 2020
At A Glance
- Despite ongoing investigations by public health officials, the exact cause of EVALI remains unclear.
- Patients with EVALI typically have a combination of respiratory and gastrointestinal symptoms, as well as general symptoms like fever or fatigue.
- Chest CT findings in EVALI most commonly show a pattern of diffuse lung injury with sparing of the periphery of the lungs.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. — Pulmonary imaging is important in the diagnosis of the acute lung injury associated with vaping, known as electronic cigarette or vaping product use-associated lung injury (EVALI), according to a special review article published in the journal Radiology. The report outlines what is currently known about this condition and discusses remaining questions.
Although e-cigarettes have been often marketed as a safer alternative to traditional cigarettes, EVALI has emerged as a serious and sometimes fatal complication of vaping.
Radiologists play a key role in the evaluation of suspected EVALI. Accurate identification of the condition allows for prompt medical treatment, which may decrease the severity of injury in some patients.
“Rapid clinical and/or radiologic recognition of EVALI allows clinicians to treat patients expeditiously and provide supportive care,” said Seth Kligerman, M.D., associate professor at UC San Diego School of Medicine and division chief of cardiothoracic radiology at UC San Diego Health in San Diego, California. “Although detailed clinical studies are lacking, some patients with EVALI rapidly improve after the administration of corticosteroids. Additionally, making the correct diagnosis may prevent unnecessary therapies and procedures, which themselves can lead to complications.”
Despite ongoing investigations by public health officials, the exact cause of EVALI remains unclear. What is currently known is that most patients are young adult and adolescent men. Over 80% of EVALI patients report vaping tetrahydrocannabinol (THC) or cannabidiol CBD containing compounds.
Patients with EVALI typically have a combination of respiratory and gastrointestinal symptoms, as well as general symptoms like fever or fatigue. Chest CT findings in EVALI can be variable but most commonly show a pattern of diffuse lung injury with sparing of the periphery of the lungs. EVALI is a diagnosis of exclusion. The patient must have a history of vaping within 90 days and abnormal findings on chest imaging, but other possible causes for the patient’s symptoms must be eliminated.
Dr. Kligerman also notes that some patients may present to the emergency department with relatively mild symptoms or radiologic findings.
“If EVALI is not diagnosed in a timely manner, patients may continue vaping after leaving the doctor’s office, clinic or emergency department which could lead to worsening lung injury,” he said.
The article cautions that aside from EVALI, vaping may pose long-term health risks. Nicotine and THC addiction, cardiovascular disease and chronic pulmonary injury are all potential consequences of e-cigarette use and are particularly concerning in the predominantly younger population that is associated with vaping.
“Right now, we do not know the long-term effects of vaping, as it is still a relatively new method of nicotine and THC delivery, and there are countless variables involved which further confound our understanding of what is happening on a patient-specific level,” Dr. Kligerman said.
He added that while recent studies have shown an association between vaping and the development of asthma, chronic bronchitis and chronic obstructive pulmonary disease, these studies have only shown an association and not causation.
“Although I am hesitant to speculate on specifics as we just do not have the data, I would not be surprised if vaping is directly linked to many of the chronic pulmonary and cardiovascular diseases commonly associated with traditional cigarette smoking,” Dr. Kligerman said.
“The link between vaping and lung cancer is unknown at this point,” he noted.
Studies with long-term follow up will be needed to evaluate EVALI patients for these conditions and others, including malignancies, that may require longer term vaping exposure to develop.
“Radiologic, Pathologic, Clinical, and Physiologic Findings of Electronic Cigarette or Vaping Product Use–associated Lung Injury (EVALI): Evolving Knowledge and Remaining Questions.” Collaborating with Dr. Kligerman were Costa Raptis, M.D., Brandon Larsen, M.D., Ph.D., Travis S. Henry, M.D., Alessandra Caporale, Ph.D., Henry Tazelaar, M.D., Mark L. Schiebler, M.D., Felix W. Wehrli, Ph.D., Jeffrey S. Klein, M.D., and Jeff Kanne, M.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on chest CT, visit RadiologyInfo.org.
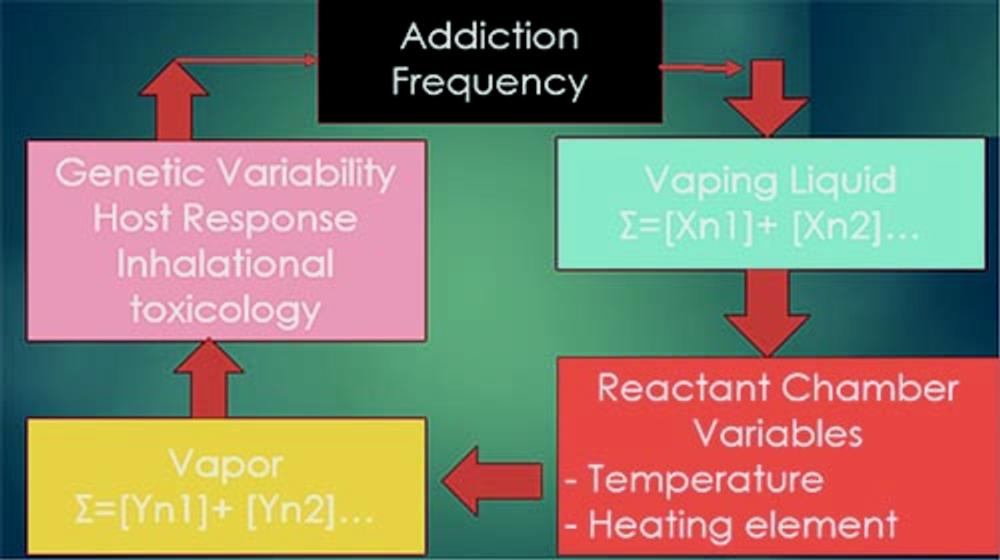
Figure 1. Diagram demonstrates host factors that influence lung injury response to vaping. Factors are dependent both on personal behavior (addiction frequency), what vaping agents (reactants) are used ([Xn1] + [Xn2]…), temperature of heating filament and temperature of walls of reactant chamber, what new chemicals (products) are made in filament chamber ([Yn1 + [Yn2]…), and host response to these chemicals.
High-res (TIF) version
(Right-click and Save As)

Figure 2. Graphs show blood flow velocity in femoral artery during reactive hyperemia before versus after nonnicotine electronic cigarette vaping. (a) Solid lines represent averages (31 subjects) of time-course data, along with standard errors. Cuff was released at time (t) of 0, after 5 minutes of occlusion (shaded area). Horizontal lines indicate baseline values of arterial blood flow velocity, acquired precuff occlusion (extended to entire time-course to facilitate visualization of hyperemic effects). Slope of curve (hyperemic index [HI]), peak velocity (VP), and time to peak (TP) are indicated. (b) Comparison of extracted parameters illustrates highly significant acute effects of vaping a single denicotinized e-cigarette.
High-res (TIF) version
(Right-click and Save As)
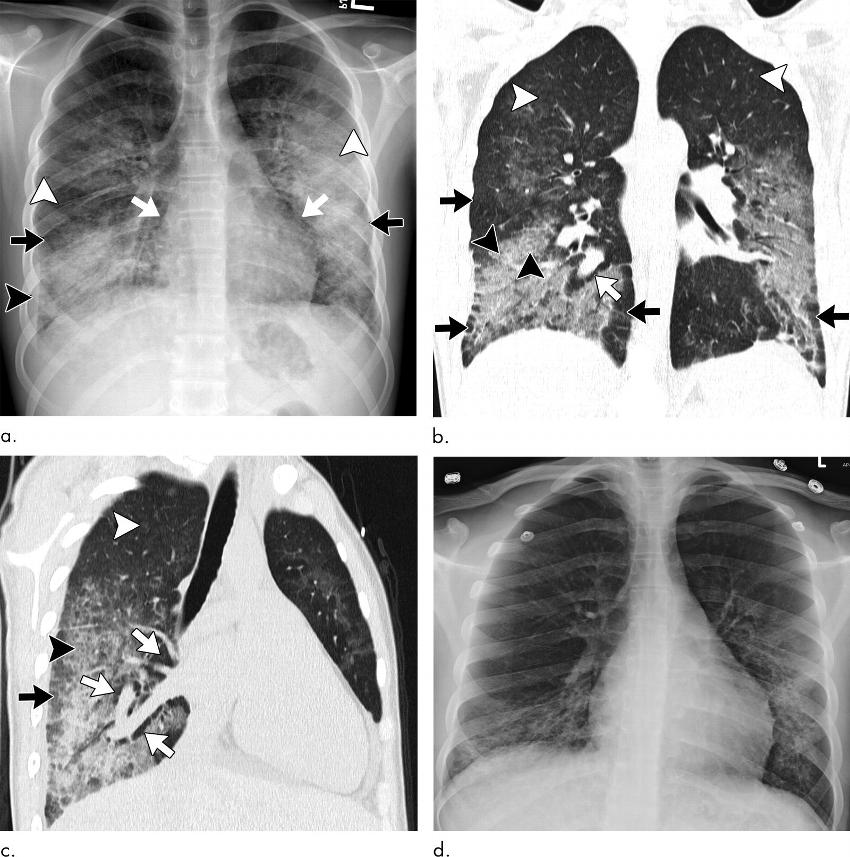
Figure 3. Images show electronic cigarette or vaping product use–associated lung injury with organizing pneumonia pattern secondary to vaping tetrahydrocannabinol in an 18-year-old man. (a) Posteroanterior radiograph shows midlung and lower lung consolidation and opacity bilaterally. Small right pleural effusion (black arrowhead) and septal thickening (white arrowhead) are seen. There is conspicuous sparing of cardiac borders (white arrows) as well as subpleural portions of lung (black arrows). (b) Coronal and (c) sagittal oblique images from CT nicely illustrate radiographic findings with mild and lower lung–predominant ground-glass opacity with few areas of consolidation. Prominent subpleural and perilobular sparing is present (black arrows). In addition, there is conspicuous sparing of peribronchovascular interstitium, best illustrated around larger pulmonary arteries and veins (white arrows). Hazy upper lobe–predominant ground-glass centrilobular nodules are present bilaterally (white arrowheads). In addition to thickening of interlobular septa, there are few areas with thickening of intralobular septa creating “crazy paving” pattern (black arrowheads). (d) Three days after initiation of steroids, patient showed dramatic clinical and radiographic improvement.
High-res (TIF) version
(Right-click and Save As)
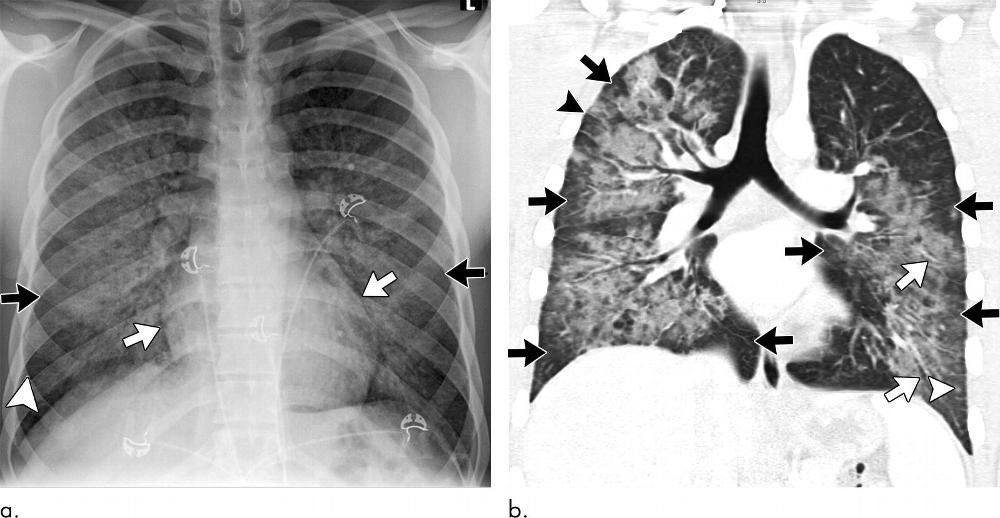
Figure 4. Images show electronic cigarette or vaping product use–associated lung injury with organizing pneumonia pattern in an 18-year-old man who vaped nicotine and tetrahydrocannabinol with fever of 103°F, vomiting for 3 days, and negative workup for infection and rheumatologic disease. (a) Posteroanterior radiograph shows perihilar predominant hazy opacity with conspicuous sparing of both heart border (white arrows) and periphery (black arrows). Septal thickening is present (arrowhead). (b) Corresponding CT image shows perihilar predominant ground-glass opacity with prominent sparing of subpleural interstitium both peripherally and centrally (black arrows) with intermixed areas of lobular sparing. In addition, there is sparing of peribronchovascular interstitium (white arrows). Septal thickening (black arrowhead) and scattered centrilobular nodules are present (white arrowhead). Patient rapidly improved after administration of steroids.
High-res (TIF) version
(Right-click and Save As)
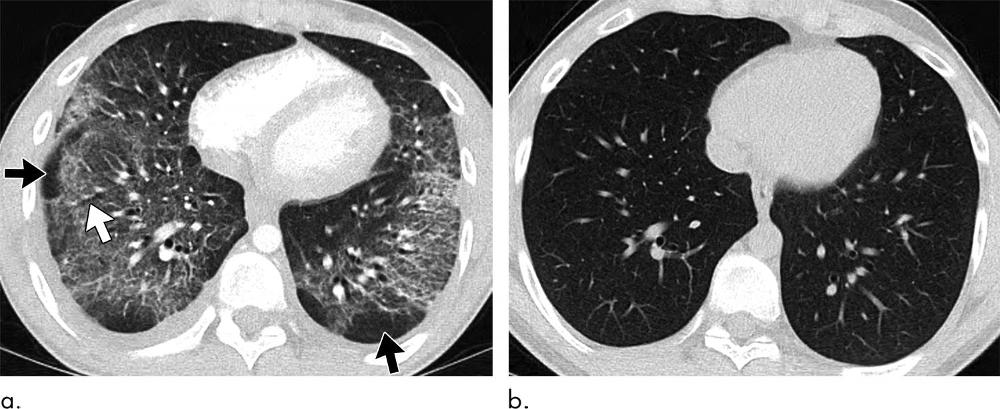
Figure 5. Images show electronic cigarette or vaping product use–associated lung injury with organizing pneumonia pattern in a 20-year-old man who vapes nicotine and tetrahydrocannabinol products daily and who presented to community health clinic with fever, weakness, and chills. He was initially diagnosed with community-acquired pneumonia, but his symptoms continued to progress despite antibiotic therapy. Extensive work-up for infection and rheumatologic disease was negative during hospital admission. (a) Axial CT image shows peribronchiolar ground-glass opacity with subpleural sparing both centrally and peripherally (black arrows). Few areas of bronchial dilation are present in areas of ground-glass opacity (white arrow). Bronchoscopic biopsy yielded result of organizing pneumonia. (b) Four weeks after initiation of steroid therapy, patient’s CT scan was normal.
High-res (TIF) version
(Right-click and Save As)
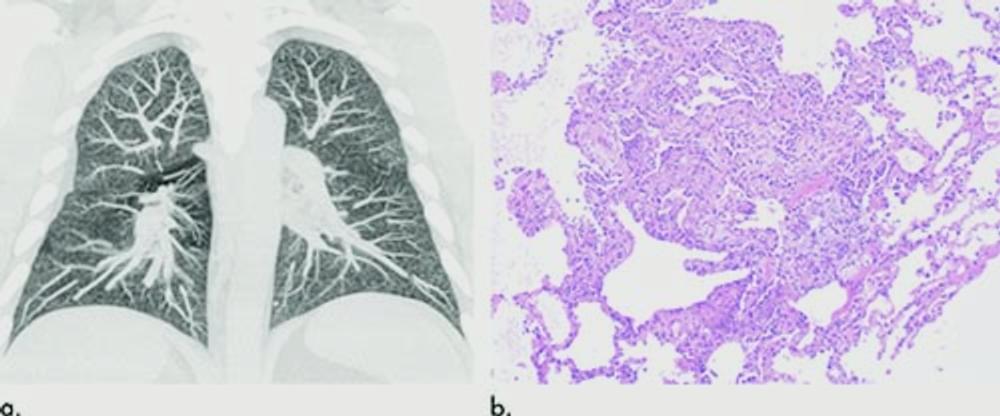
Figure 6. Images show electronic cigarette or vaping product use–associated lung injury in a 32-year-old man with history of vaping who presented with fevers and night sweats for 1 week. (a) Coronal maximum intensity projection image shows diffuse centrilobular nodularity. (b) Histologic sections of his transbronchial cryobiopsy showed distinctive micronodular pattern of airway-centered organizing pneumonia, corresponding to centrilobular nodularity seen at CT. Similar imaging and pathologic findings have been described in patients with smoke synthetic cannabinoids.
High-res (TIF) version
(Right-click and Save As)
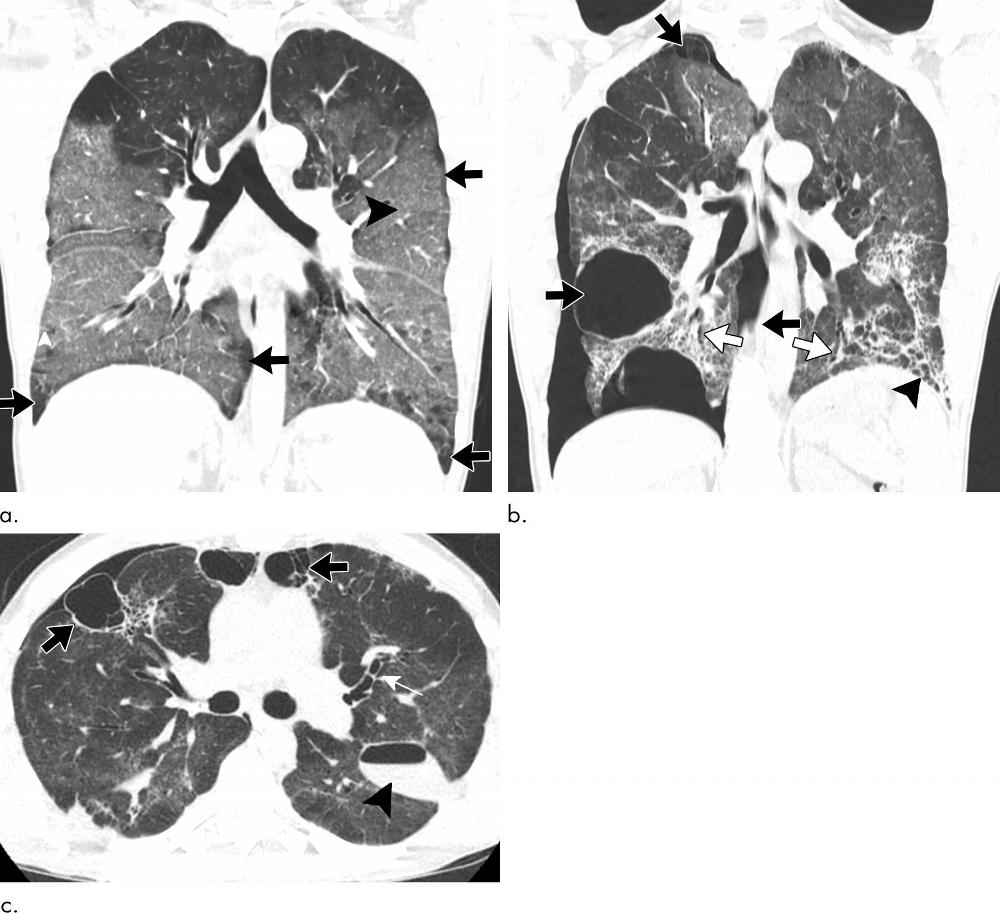
Figure 7. Images show electronic cigarette or vaping product use–associated lung injury in a 37-year-old man with history of vaping tetrahydrocannabinol products daily. (a) Coronal CT image shows diffuse ground-glass opacity with subpleural sparing (arrows) and interlobular and intralobular septal thickening creating “crazy paving” pattern (arrowhead). At initial CT, it is unclear whether this represents organizing pneumonia or early exudative phase of diffuse alveolar damage. Patient’s condition dramatically worsened with progressive consolidation and volume loss requiring intubation. (b) Coronal and (c) axial CT images 14 days after initial study show improvement of ground-glass opacity with interval development of lower lobe–predominant fibrosis with reticulation (black arrowhead in b), bronchiectasis (white arrows), and volume loss. Additionally, there has been development of numerous bullae of varying sizes bilaterally (black arrows), moderate-size right pneumothorax, and loculated hydropneumothorax along left major fissure (black arrowhead). (Images courtesy of Tan-Lucien Mohammed, MD, Professor of Radiology, University of Florida.)
High-res (TIF) version
(Right-click and Save As)
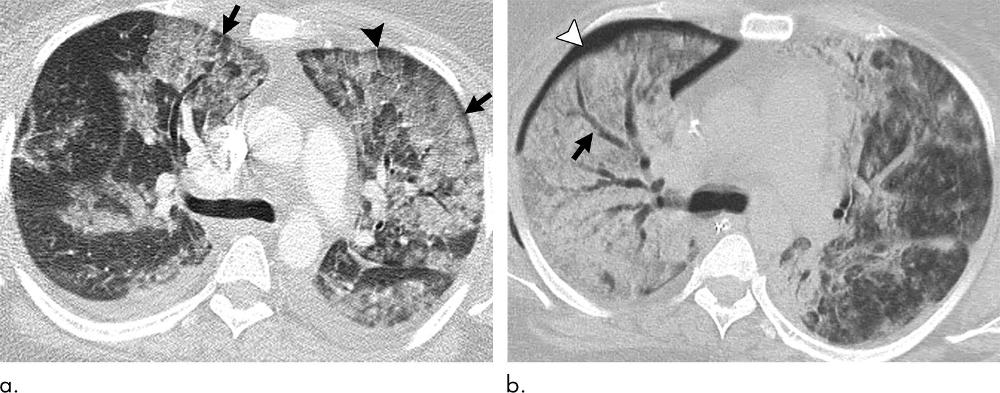
Figure 8. Images show electronic cigarette or vaping product use–associated lung injury with diffuse alveolar damage pattern in a 35-year-old woman who vaped tetrahydrocannabinol. Work-up for infection and rheumatologic disease was negative. (a) Axial CT scan shows ground-glass opacity, left greater than right, with areas of consolidation. Subpleural and perilobular sparing is present (arrows). Septal thickening is present (arrowhead). (b) CT scan 2 weeks later shows extensive right lung consolidation with areas of bronchial dilation (arrow) and internal development of right pneumothorax (arrowhead). Ground-glass opacity in left lung has improved with residual centrilobular nodularity. Patient died 5 days later.
High-res (TIF) version
(Right-click and Save As)
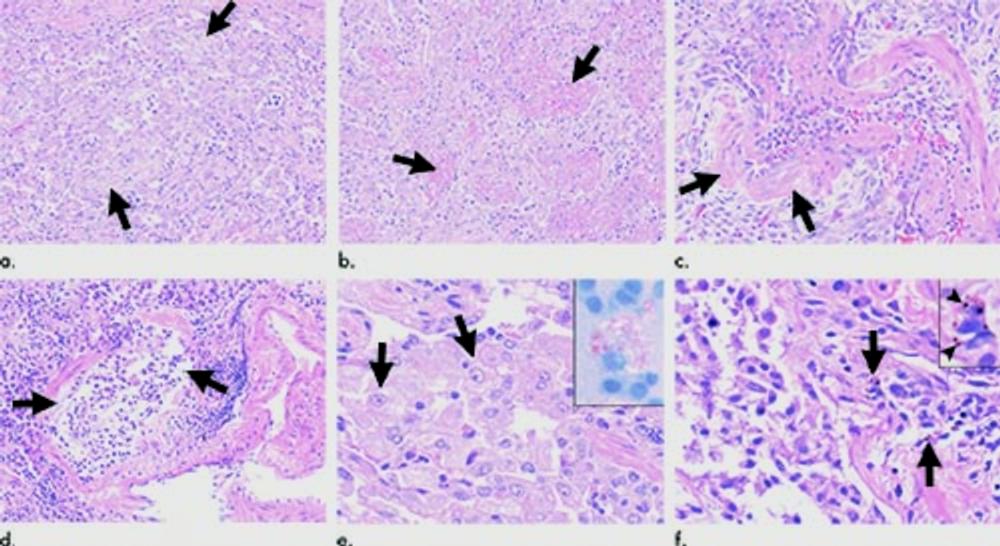
Figure 9. Images show histopathologic findings of vaping-associated lung injury. Representative photomicrographs of lung biopsies from patients with electronic cigarette or vaping product use–associated lung injury show variety of acute injury patterns including (a) organizing pneumonia (arrows), (b) acute fibrinous pneumonitis with balls of intra-alveolar fibrin (arrows), and (c) diffuse alveolar damage with hyaline membranes (arrows). Other common findings include (d) bronchiolitis with bronchiolar mucosal ulceration (arrows) and (e) accumulation of foamy lipid-laden macrophages in alveolar spaces (arrows) that can be detected in bronchoalveolar lavage fluid with Oil-Red-O lipid stain (inset image). (f) Occasional scattered macrophages (arrows) may also contain brown or black pigmented particles (arrowheads, inset image) in some cases, which can be a helpful clue particularly when patient is a nonsmoker.
High-res (TIF) version
(Right-click and Save As)
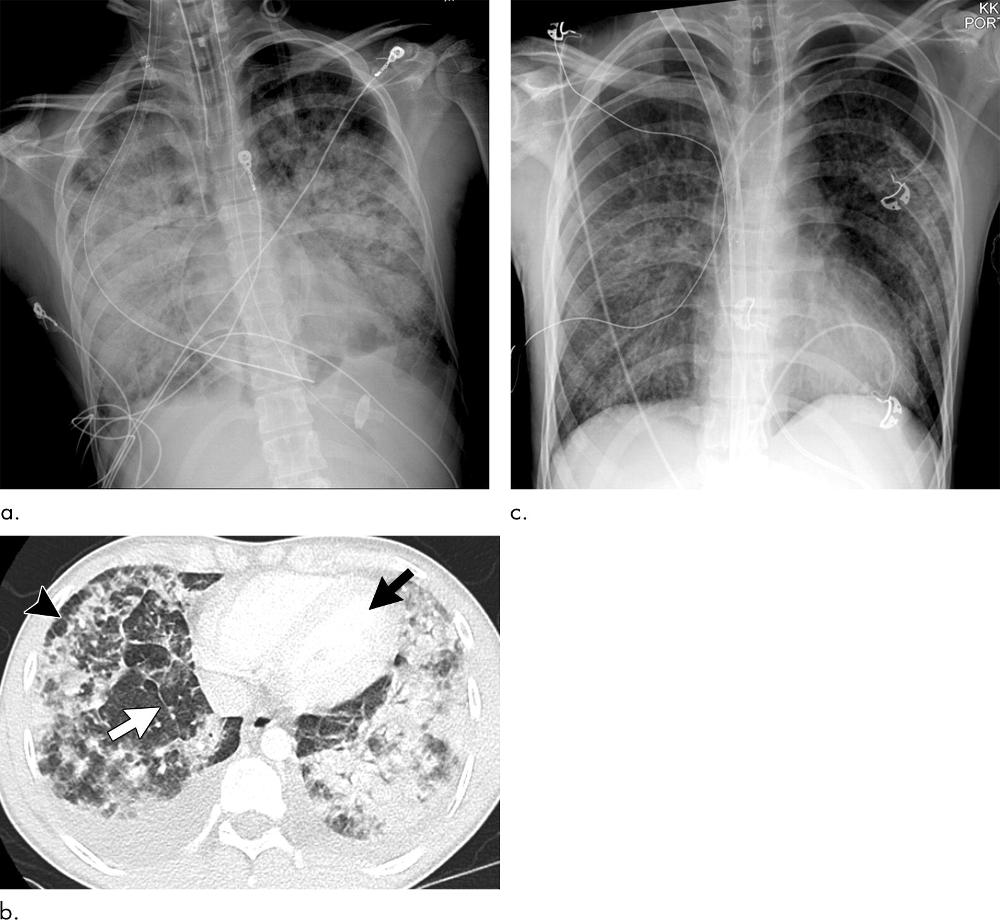
Figure 10. Images show electronic cigarette or vaping product use–associated lung injury secondary to acute eosinophilic pneumonia in a 21-year-old man who had been vaping nicotine and tetrahydrocannabinol products daily. (a) Posteroanterior radiograph 2 days after admission shows extensive consolidation. (b) Although imaging findings are often nonspecific, presence of extensive consolidation with areas of lobular and subplerual sparing (black arrowhead), such as that seen with diffuse alveolar damage, with associated prominent septal thickening (white arrow), moderate to large bilateral plerual effusions, and normal appearing left ventricle (black arrow), should raise possibility of acute eosinophilic pneumonia. Clinical diagnosis is also difficult because peripheral eosinophils are often not elevated until many days after start of symptoms. Patient’s clinical condition and radiographic imaging continued to worsen and he was subsequently started on extracorporeal membrane oxygenation. Patient subsequently underwent bronchoscopy, which showed large percentage of eosinophils. (c) Three days after initiation of steroids, chest radiograph has significantly improved. (Images courtesy of Howard Mann, MBBCh, Professor of Radiology, University of Utah.)
High-res (TIF) version
(Right-click and Save As)
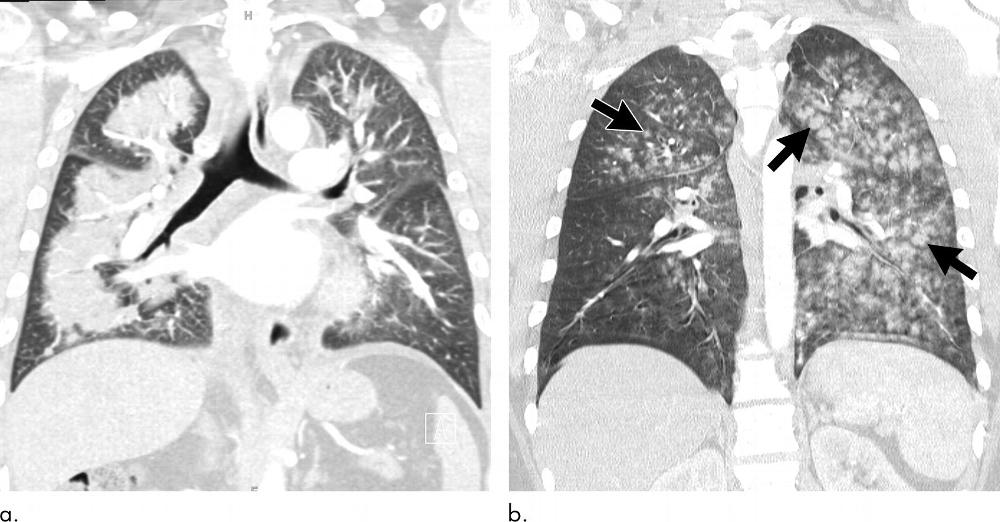
Figure 11. Images show electronic cigarette or vaping product use–associated lung injury secondary to acute eosinophilic pneumonia in a 21-year-old man who had been vaping nicotine and tetrahydrocannabinol products daily. (a) Posteroanterior radiograph 2 days after admission shows extensive consolidation. (b) Although imaging findings are often nonspecific, presence of extensive consolidation with areas of lobular and subplerual sparing (black arrowhead), such as that seen with diffuse alveolar damage, with associated prominent septal thickening (white arrow), moderate to large bilateral plerual effusions, and normal appearing left ventricle (black arrow), should raise possibility of acute eosinophilic pneumonia. Clinical diagnosis is also difficult because peripheral eosinophils are often not elevated until many days after start of symptoms. Patient’s clinical condition and radiographic imaging continued to worsen and he was subsequently started on extracorporeal membrane oxygenation. Patient subsequently underwent bronchoscopy, which showed large percentage of eosinophils. (c) Three days after initiation of steroids, chest radiograph has significantly improved. (Images courtesy of Howard Mann, MBBCh, Professor of Radiology, University of Utah.)
High-res (TIF) version
(Right-click and Save As)
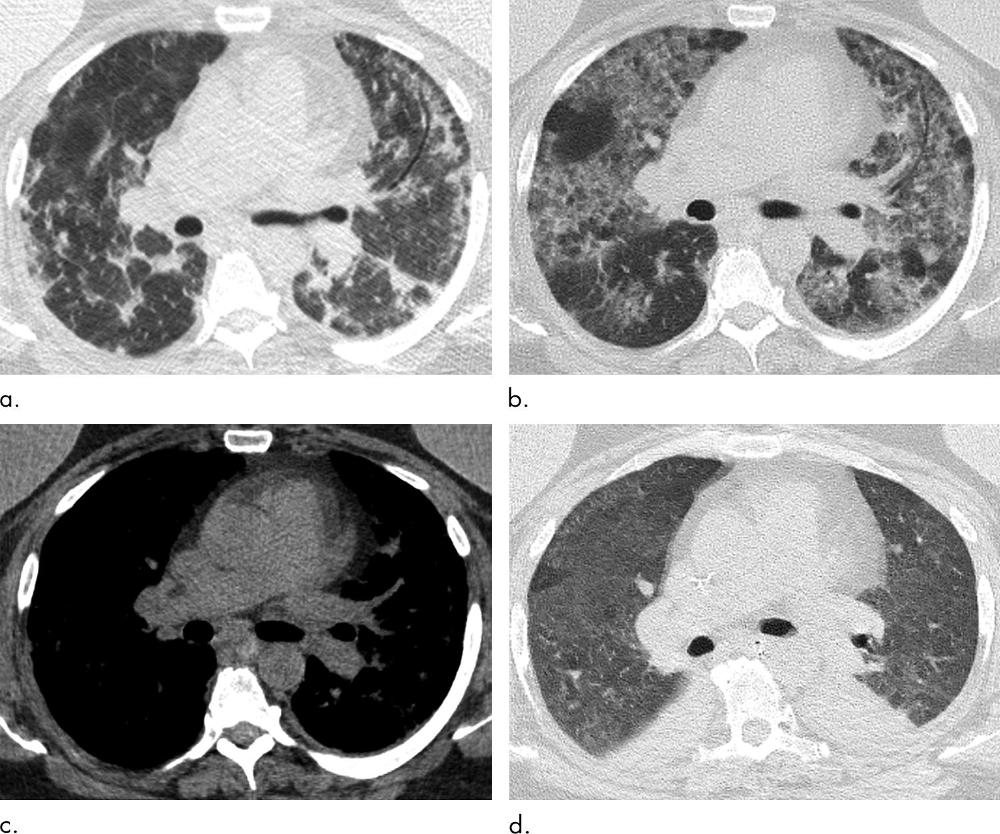
Figure 12. Images show multiple episodes of electronic cigarette or vaping product use–associated lung injury due to repeated vaping of nicotine with mint flavoring in a 51-year-old woman. Bronchoalveolar lavage (BAL) fluid showed numerous foamy lipid-laden macrophages with positive Oil-Red-O lipid staining. (a) CT in September shows organizing pneumonia pattern with scattered areas of ground-glass opacity with subpleural sparing. Workup for infection was negative, and patient was started on steroids and improved. (b) Two months later, patient returned to emergency department with dyspnea and fever. CT image shows more extensive ground-glass opacity with areas of lobular and subpleural sparing. Interlobular and intralobular septal thickening is present, creating “crazy paving” pattern. (c) Although patient’s BAL fluid showed many lipid-laden macrophages, soft-tissue image shows no evidence of intraparenchymal fat attenuation, a common finding in lipoid pneumonia. Patient’s condition deteriorated, and she was intubated and started on steroids. (d) Ten days after initiation of steroids, ground-glass opacity has improved but persists. Patient’s condition was complicated by aspiration pneumonia and bilateral lower-lobe collapse.
High-res (TIF) version
(Right-click and Save As)
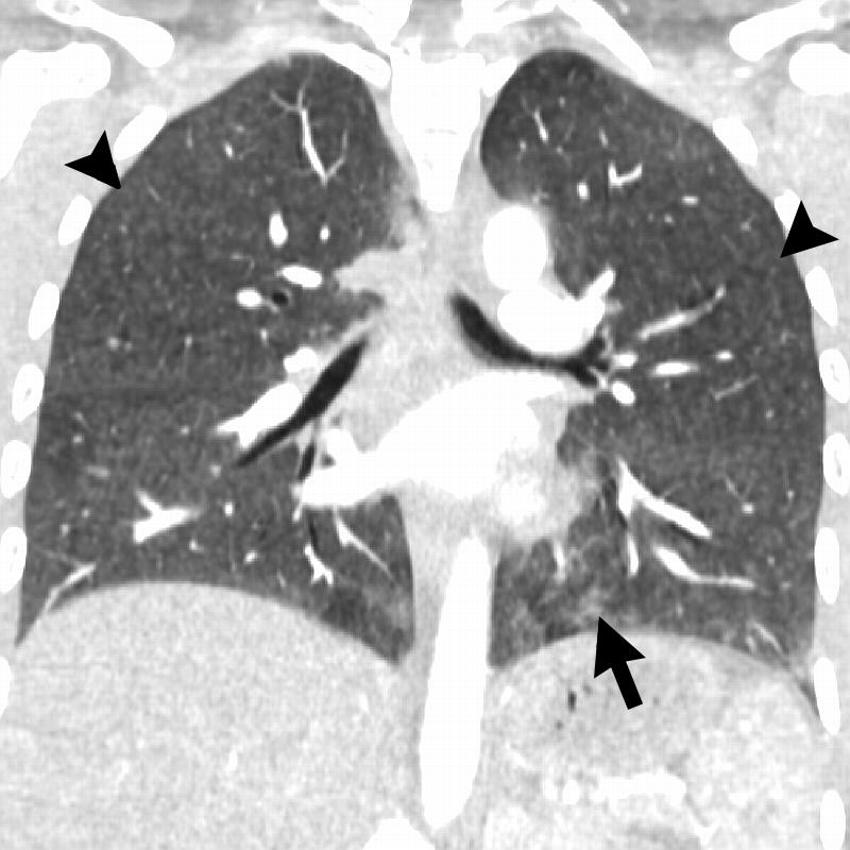
Figure 13. Coronal image shows hypersensitivity pneumonitis (HP) pattern in a 35-year-old man who vaped tetrahydrocannabinol products. Extensive hazy centrilobular nodularity (arrowheads) is most pronounced in midlung and upper lung zones consistent with inhalational injury. Mild ground-glass opacity is present as bases (arrow). This imaging pattern is commonly seen in HP. Patient’s condition rapidly improved after steroid administration and no biopsy was obtained. Although authors have seen a few cases with HP pattern, there are no cases in literature with pathologic confirmation. Other possible etiologies for diffuse pattern of centrilobular nodules in electronic cigarette or vaping product use–associated lung injury includes airway-centered foci of organizing pneumonia.
High-res (TIF) version
(Right-click and Save As)