Steroid Injections of Hip and Knee May Damage Joints
Released: October 15, 2019
At A Glance
- Steroid injections may lead to joint collapse or hasten the need for total hip or knee replacement.
- Corticosteroids are anti-inflammatory medications that can be injected into joints to treat pain and swelling associated with osteoarthritis.
- Patients with joint pain but with mild or no osteoarthritis on X-rays may be at risk of developing rapid progressive joint space loss or destructive osteoarthritis after corticosteroid injections.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. — Corticosteroid injections used to treat osteoarthritis pain in the hip and knee may be more dangerous than previously thought, according to a special report published in the journal Radiology. Researchers suggested that injection-associated risks like rapid progressive osteoarthritis, which eventually may lead to joint collapse, should be integrated into consent forms so that patients are aware of the potential risks associated with these treatments.
Osteoarthritis of the hip and knee are common and debilitating joint disorders. Physicians often inject anti-inflammatory corticosteroids into the joint to treat the pain and swelling associated with osteoarthritis. The procedure is widely viewed as safe, and patient consent forms mainly mention the risks of hemorrhage and infection among more rare side effects associated with most needle-based procedures.
However, a recent study led by Ali Guermazi, M.D., Ph.D., professor of radiology and medicine at Boston University School of Medicine, found that corticosteroid injections may be associated with complications that potentially accelerate the destruction of the joint and may hasten the need for total hip and knee replacements.
"We've been telling patients that even if these injections don't relieve your pain, they're not going to hurt you," Dr. Guermazi said. "But now we suspect that this is not necessarily the case."
In a review of existing literature on complications after treatment with corticosteroid injections, Dr. Guermazi and colleagues identified four main adverse findings: accelerated osteoarthritis progression with loss of the joint space, subchondral insufficiency fractures (stress fractures that occur beneath the cartilage), complications from osteonecrosis (death of bone tissue), and rapid joint destruction including bone loss.
The researchers recommend careful scrutiny of patients with mild or no osteoarthritis on X-rays who are referred for injections to treat joint pain, especially when the pain is disproportionate to the imaging findings. Prior research has shown that these patients are at risk of developing rapid progressive joint space loss or destructive osteoarthritis after injections. Physicians may also want to reconsider a planned injection when the patient has acute change in pain not explained by X-rays as some underlying condition affecting joint health may be ongoing, the researchers said. Most importantly, younger patients and patients earlier in the course of the disease need to be told of the potential consequences of a corticosteroid injection before they receive it.
"Physicians do not commonly tell patients about the possibility of joint collapse or subchondral insufficiency fractures that may lead to earlier total hip or knee replacement," Dr. Guermazi said. "This information should be part of the consent when you inject patients with intra-articular corticosteroids."
With corticosteroid injections so widely used, the potential implications of the study are enormous, according to Dr. Guermazi.
"Intra-articular joint injection of steroids is a very common treatment for osteoarthritis-related pain, but potential aggravation of pre-existing conditions or actual side effects in a subset of patients need to be explored further to better understand the risks associated with it," Dr. Guermazi said. "What we wanted to do with our paper is to tell physicians and patients to be careful, because these injections are likely not as safe as we thought."
"Intra-articular Corticosteroid Injections of the Hip and Knee: Perhaps Not as Safe as We Thought?" Collaborating with Dr. Guermazi were Andrew J. Kompel, M.D., Frank W. Roemer, M.D., Akira M. Murakami, M.D., Luis E. Diaz, M.D., and Michel D. Crema, M.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wis., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of over 53,400 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on radiography and arthritis, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
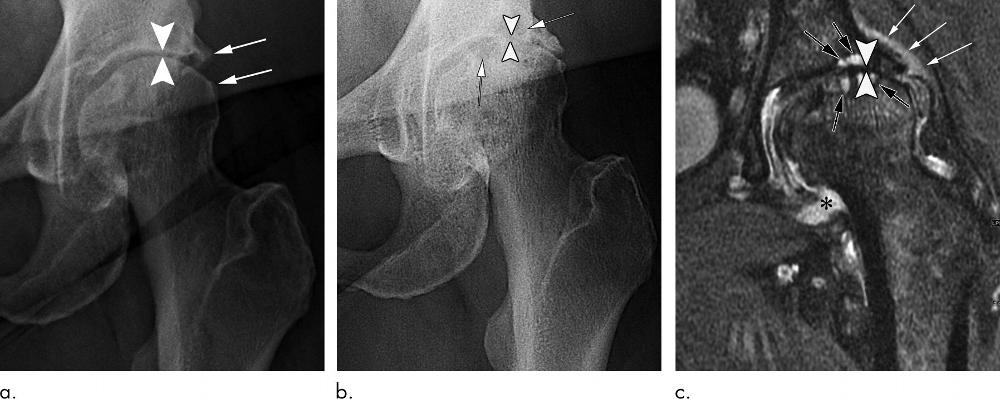
Figure 1. Rapid progressive osteoarthritis joint space loss (type 1) in a 61-year-old woman who presented with hip pain. (a) Anteroposterior left hip radiograph shows joint space narrowing (arrowheads) and femoral and acetabular osteophytic changes (arrows) consistent with Kellgren-Lawrence grade III hip osteoarthritis. She was referred for US-guided steroid injection. (b) Four months after intraarticular corticosteroid injection, she presented with worsening left hip pain. Anteroposterior hip radiograph shows severe interval joint space narrowing (arrowheads) and enlarging subchondral cysts (arrows). (c) Coronal intermediate-weighted fat-suppressed MRI obtained at the same time as b shows complete loss of the acetabular and femoral cartilage (arrowheads), with subchondral cystic changes (black arrows). In addition, there is joint effusion and synovitis (*) and periarticular soft-tissue edema (white arrows). This patient underwent total joint replacement 3 months later.
High-res (TIF) version
(Right-click and Save As)
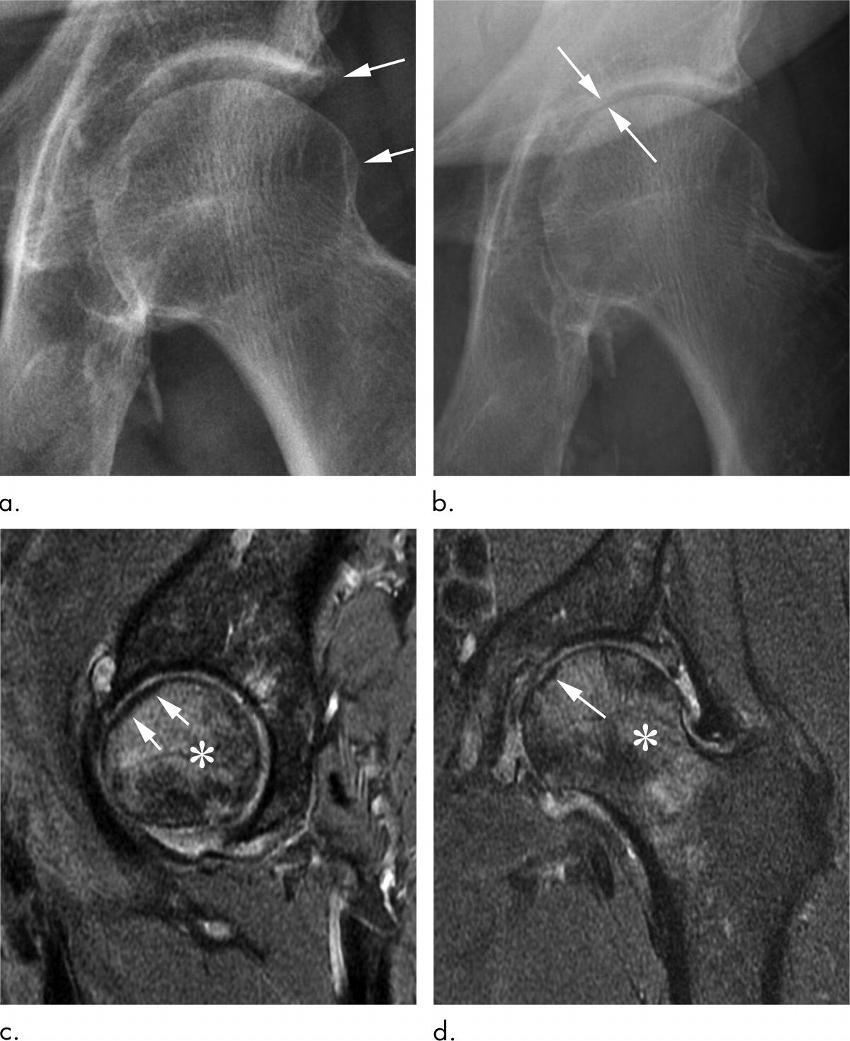
Figure 2. Rapid progressive osteoarthritis joint space loss (type 1) and subchondral insufficiency fracture in a 53-year-old man who presented with hip pain. (a) Anteroposterior left hip radiograph shows mild osteophytic changes (arrows) and no joint space loss. This patient was referred for intra-articular corticosteroid injection. (b) Seven weeks after injection, he returned with worsening hip pain. Repeat anteroposterior left hip radiograph shows accelerated loss of joint space (arrows). (c) Sagittal intermediate-weighted fat-suppressed MRI obtained at the same time as b shows a linear subchondral hypointensity representing subchondral insufficiency fracture of the anterior superior femoral head with subtle flattening of the overlying articular surface (arrows). Extensive bone marrow edema extends to the femoral neck (*). (d) Corresponding coronal intermediate-weighted fat-suppressed MRI enables us to confirm the presence of a subchondral insufficiency fracture (arrow) and depicts the true extent of bone marrow edema (*).
High-res (TIF) version
(Right-click and Save As)
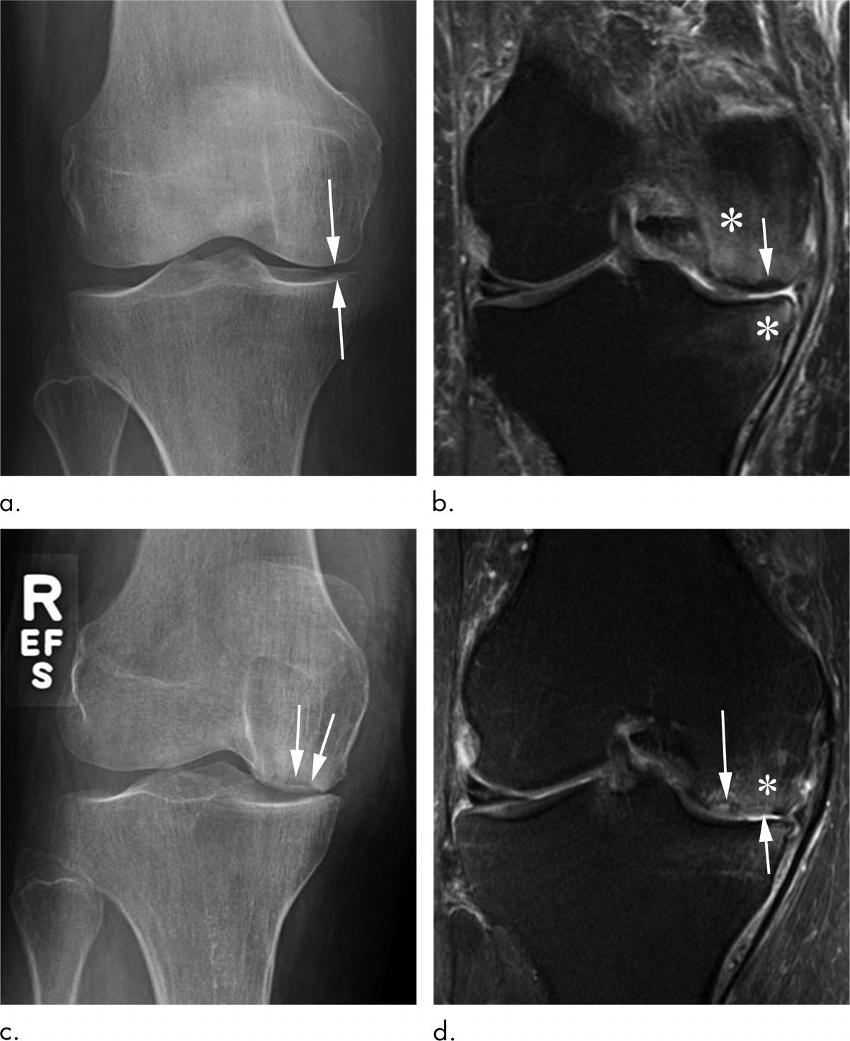
Figure 3. Subchondral insufficiency fracture in a 69-year-old woman who presented with acutely worsening knee pain without known trauma. (a) Anteroposterior radiograph of the right knee shows possible medial compartment joint space narrowing (arrows) without osteophytes. There are no signs of osteonecrosis or subchondral insufficiency fracture. (b) Coronal intermediate-weighted fat-suppressed MRI obtained at the same time as a shows a subchondral insufficiency fracture of the medial femoral condyle, without collapse of the articular surface (arrow). In addition, there is marked femoral and tibial bone marrow edema (*). This patient was not treated with conservative measures (ie, switch to non–weight-bearing activity) and received an intra-articular corticosteroid injection. (c) Eleven months later, she returned with continued right knee pain. Repeat anteroposterior radiograph of the right knee shows collapse of the medial femoral condyle articular surface (arrows). (d) Coronal intermediate-weighted MRI acquired at the same time as c demonstrates deformity of the articular surface (short arrow) of the medial femoral condyle in the area of a previously noted subchondral insufficiency fracture (long arrow). In addition, there is marked bone marrow edema (*).
High-res (TIF) version
(Right-click and Save As)
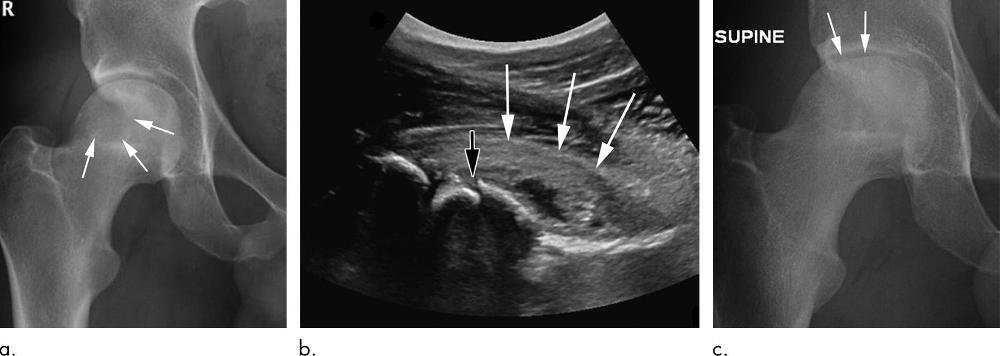
Figure 4. Osteonecrosis in a 29-year-old man who presented with right hip pain. (a) Anteroposterior radiograph of the pelvis shows osteonecrosis in the right femoral head, with preserved femoral head contours (arrows). He subsequently went to the sports medicine clinic and received a right hip joint corticosteroid injection for pain. (b) Three months later, he was referred to our institution for repeat intra-articular corticosteroid injection. The patient presented with a severe limp when walking and described the pain as worse than his original pain. Preprocedural sagittal US image shows a defect in the anterior right femoral head cortex (black arrow) and moderate joint effusion with a severely thickened anterior joint capsule (white arrows). The intra-articular corticosteroid injection was cancelled given the US findings, and the referring orthopedic physician was informed of the findings. (c) Repeat anteroposterior right hip radiograph obtained 1 week after US when the patient was seen in the orthopedic clinic for a follow-up visit enabled confirmation that the superior femoral head articular surface had collapsed (arrows), and the patient underwent right hip joint replacement.
High-res (TIF) version
(Right-click and Save As)

Figure 5. Rapid progressive osteoarthritis (RPOA) type 2 in an 81-year-old woman with right hip pain who was referred for right hip intra-articular corticosteroid injection. (a) Anteroposterior right hip radiograph shows no definite osteoarthritis. (b) Within 3 months after receiving the injection, this patient presented with worsening right hip pain. Repeat anteroposterior right hip radiograph shows subchondral insufficiency fracture, with collapse of the superior femoral head articular surface (arrows). (c) Pain increased markedly over the following month, and this repeat anteroposterior right hip radiograph shows bone loss and destruction of the femoral head with severe joint space loss, consistent with RPOA type 2 (arrows). In addition, there are extensive cystic changes at the acetabulum (arrowheads).
High-res (TIF) version
(Right-click and Save As)
