Bariatric Embolization Shows Promise in Treatment of Obesity
Released: April 02, 2019
At A Glance
- Researchers assessed the effects of bariatric embolization on 20 severely obese participants over the course of one year.
- Bariatric embolization was performed successfully for all participants with no major complications.
- Patients maintained weight loss of 11.5 percent after a year, as well as a decrease in hunger levels.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. — Bariatric embolization, a new, minimally invasive treatment for obesity produces weight loss and reduces appetite for up to one year, according to a new study published in the journal Radiology.
Obesity is a major public health epidemic that affects hundreds of millions of people worldwide and adds enormous costs to health care. The limited effectiveness of dieting among some patients has driven the development of surgical interventions such as gastric bypass, sleeve gastrectomy and gastric banding. While these treatments are effective, they also pose risks, highlighting the need for minimally invasive, cost-effective options.
Bariatric embolization has emerged in recent years as one such option. In the procedure, microscopic spheres are introduced through a catheter into the arteries that supply blood to the stomach. The blocking of the arteries with the beads produces a reduction in blood flow—enough to suppress production of hunger-stimulating hormones but not enough to cause tissue damage.
Researchers from the Bariatric Embolization of Arteries for the Treatment of Obesity (BEAT Obesity) trial recently assessed the procedure's effects on 20 severely obese participants over the course of one year.
Bariatric embolization was performed successfully for all participants with no major complications. Excess weight loss was 8.2 percent at one month, 11.5 percent at three months, 12.8 percent at six months, and 11.5 percent at 12 months. Patients showed a decrease in hunger and an increase in early satiety, or the feeling of being full when eating. The researchers also saw encouraging signs of metabolic changes in the patients, with decreases in total cholesterol and increases in levels of high-density lipoprotein, the so-called "good cholesterol." Tests given to the participants showed that their quality of life improved in the year after the procedure.
"This is a great step forward for this procedure in establishing early feasibility, safety and early efficacy," said study lead author Clifford R. Weiss, M.D., from the Johns Hopkins University School of Medicine in Baltimore. "It is fulfilling to all of us to see something that started as an idea develop through about a decade of research and then go all the way to an initial clinical trial."
Dr. Weiss credited his co-principal investigators, Aravind Arepally, M.D.—formerly of Johns Hopkins and currently at Piedmont Healthcare in Atlanta—and Aaron M. Fischman, M.D., of Mount Sinai Hospital in New York City. He also credits veterinarian Dara L. Kraitchman, V.M.D., Ph.D., from Johns Hopkins, who helped lead the animal studies that preceded the clinical trial.
"This is the result of collaborative research, of step-by-step basic and translational science to get to the point where we could do a clinical trial safely," Dr. Weiss said. "We had a multidisciplinary team, including interventional radiologists, gastroenterologists, dietitians, psychologists, hormone experts, bariatric surgeons and statisticians, looking at this from all different angles to make sure we were investigating it in a very rigorous and scientific way."
Although the one-year results are encouraging, Dr. Weiss emphasized that important research remains. The team has been tracking hormonal changes in the patients and are preparing to release results of that study shortly. They also intend to look at longer-term outcomes and the possible impact of the placebo effect.
Still, if the one-year results are any indication, bariatric embolization has a bright future as a tool in a more personalized approach to the treatment of obesity, a disease increasingly understood to differ from patient to patient.
"The reality is that obesity itself is an individualized disease that requires individualized treatments," Dr. Weiss said. "I see a day when there will be a multidisciplinary obesity clinic where six or seven different practitioners get together to treat the patient. This is already happening at some sites, but they are rare and they need to be more widespread, like multidisciplinary cancer centers."
"Bariatric Embolization of Arteries for the Treatment of Obesity (BEAT Obesity) Trial: Results at 1 Year." Collaborating with Drs. Weiss, Arepally, Fischman and Kraitchman were Godwin O. Abiola, B.A., Lawrence J. Cheskin, M.D., Jay Vairavamurthy, M.D., Brian P. Holly, M.D., Olaguoke Akinwande, M.D., Franklin Nwoke, M.D., Kalyan Paudel, M.D., Stephen Belmustakov, B.A., Kelvin Hong, M.D., Rahul S. Patel, M.D., Eun J. Shin, M.D., Kimberly E. Steele, M.D., Ph.D., Timothy H. Moran, Ph.D., Richard E. Thompson, Ph.D., Taylor Dunklin, B.A., and Harvey Ziessman, M.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wis., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of over 53,400 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on embolization, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
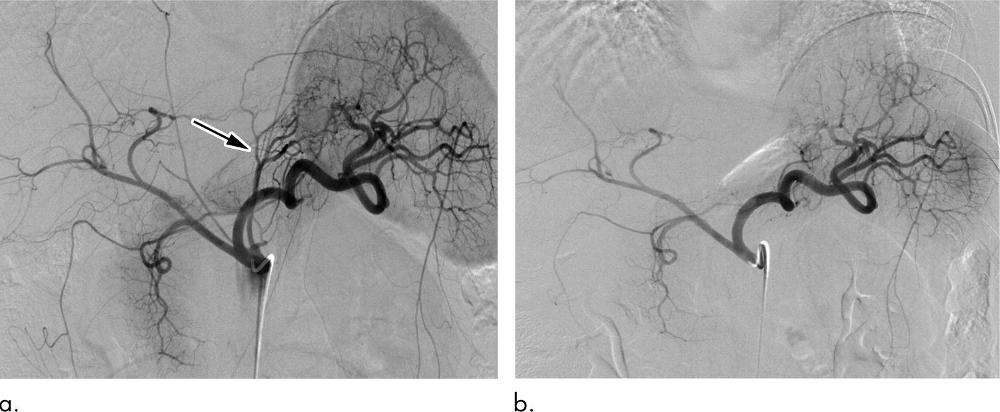
Figure 1. Figure 1: Bariatric embolization in a 41-year-old Caucasian woman with a baseline weight of 115 kg and a baseline body mass index (BMI) value of 48. At 12 months after embolization, she had weight loss of 16 kg (30 percent excess weight loss) and a BMI of 34. (a) Pre-embolization celiac angiogram showing classic left gastric artery (LGA) (arrow) anatomy, with the LGA arising from the proximal celiac artery and left gastroepiploic artery (GEA) branching from the gastroduodenal artery. (b) Postembolization angiogram showing successful embolization of the gastric fundus via the LGA and left GEA.
High-res (TIF) version
(Right-click and Save As)
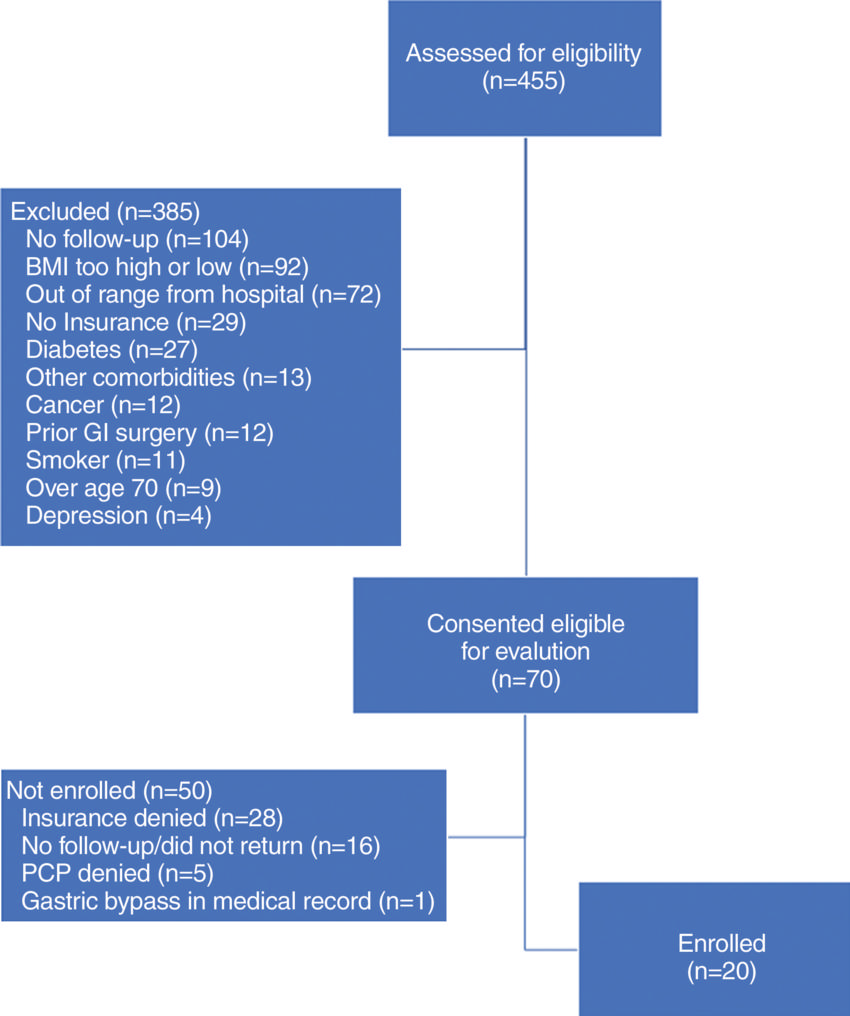
Figure 2. Participant selection flowchart. BMI = body mass index, GI = gastrointestinal, PCP = primary care provider.
High-res (TIF) version
(Right-click and Save As)
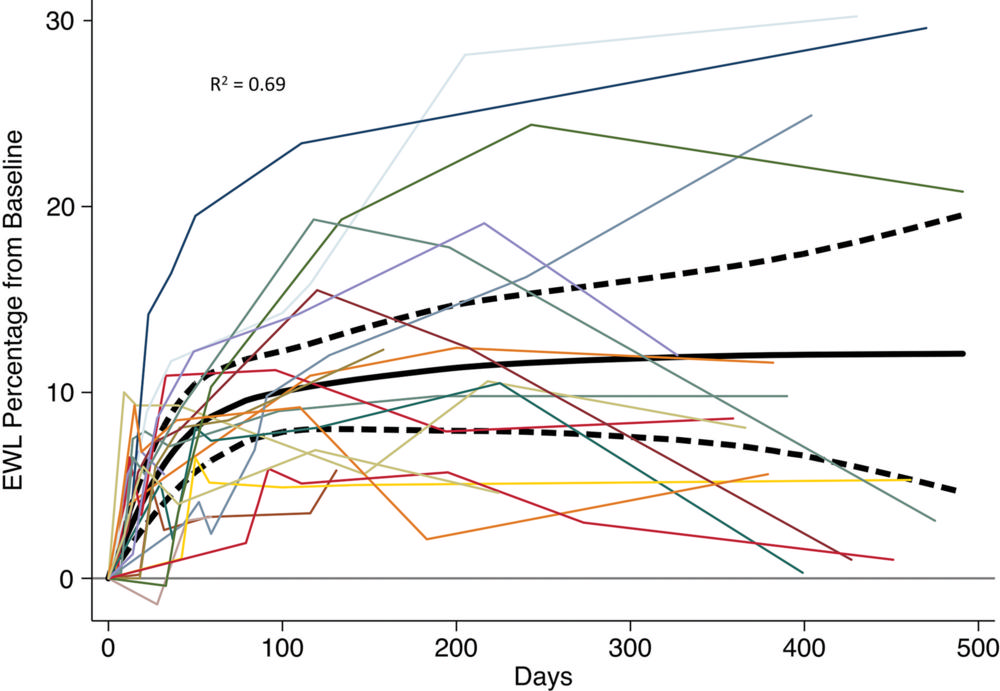
Figure 3. Excess weight loss (EWL) for the 20 participants who underwent bariatric embolization, plotted as percentage difference from baseline over time. Solid black line represents a fitted cubic spline model. Dotted lines represent 95 percent confidence interval.
High-res (TIF) version
(Right-click and Save As)
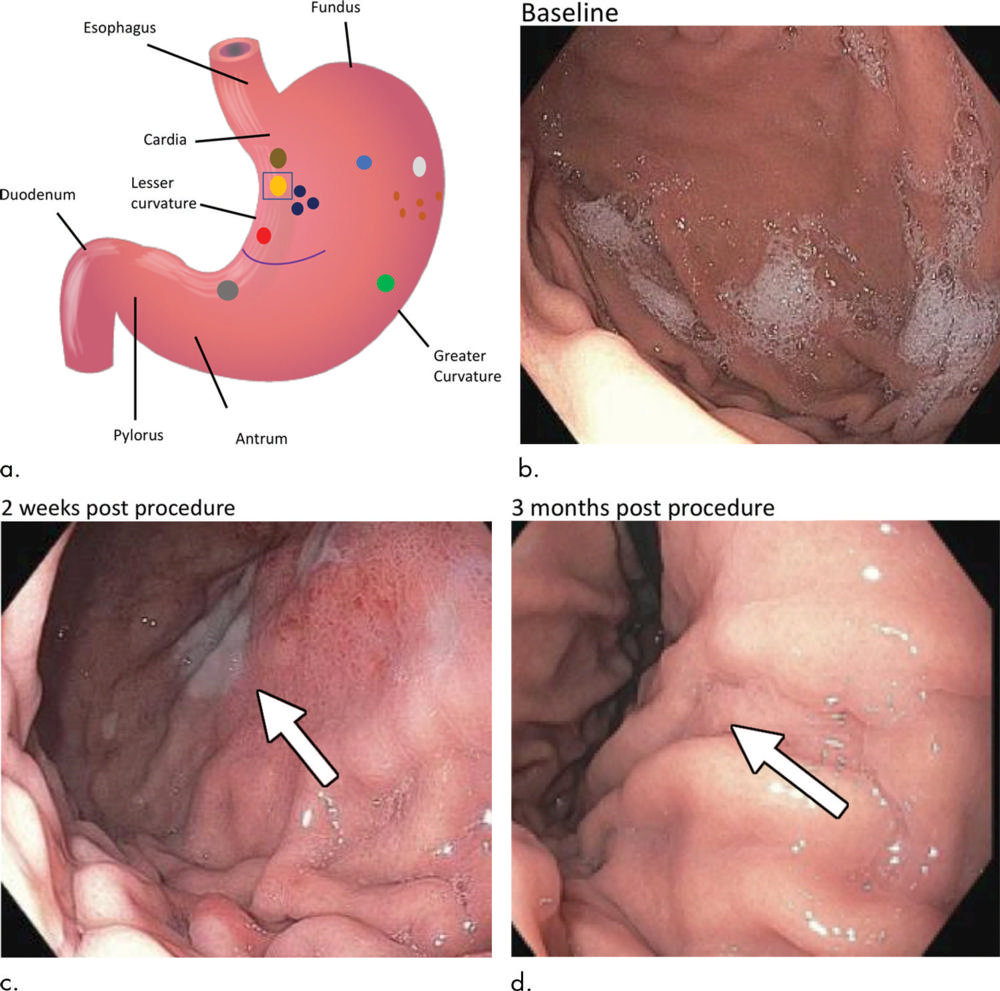
Figure 4. (a) Distribution of various gastric ulcerations observed during endoscopy 1 week after bariatric embolization. Relative sizes and shapes of ulcers are indicated by sizes and shapes of colored dots on diagram. Each color represents ulcers found on one participant (eg, the three black dots represent ulcers on one participant).The curved purple line represents a linear ulcer. The ulcer represented as a yellow oval and enclosed by a blue square corresponds to that shown in (b)-(d). (b)-(d) Endoscopic images of the same location in one participant (48-year-old African American woman with a baseline weight of 127 kg): (b) at baseline, (c) at 2 weeks after embolization (arrow indicates a small, superficial gastric ulcer, measuring 1 cm on the longest axis), and (d) at 3 months after embolization (arrow indicates prior location of the ulcer).
High-res (TIF) version
(Right-click and Save As)
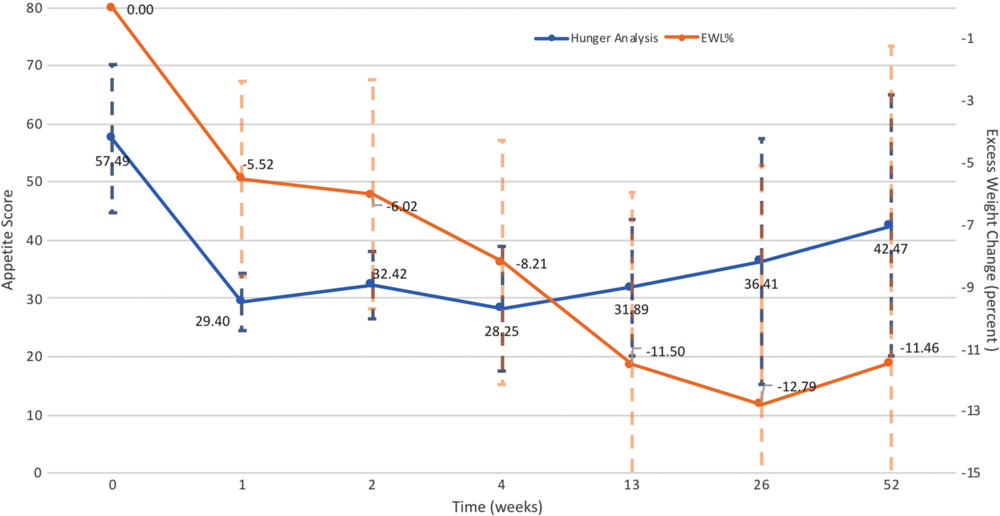
Figure 5. Hunger and excess weight loss (EWL) over time. Hunger scores were generated on the basis of subjective questions regarding appetite during the previous 3 days—before eating breakfast, before eating lunch, during midafternoon, and after dinner. Hunger scores are compared with EWL at each time point. In general, decreases in hunger scores were correlated with an increase in EWL and vice versa.
High-res (TIF) version
(Right-click and Save As)
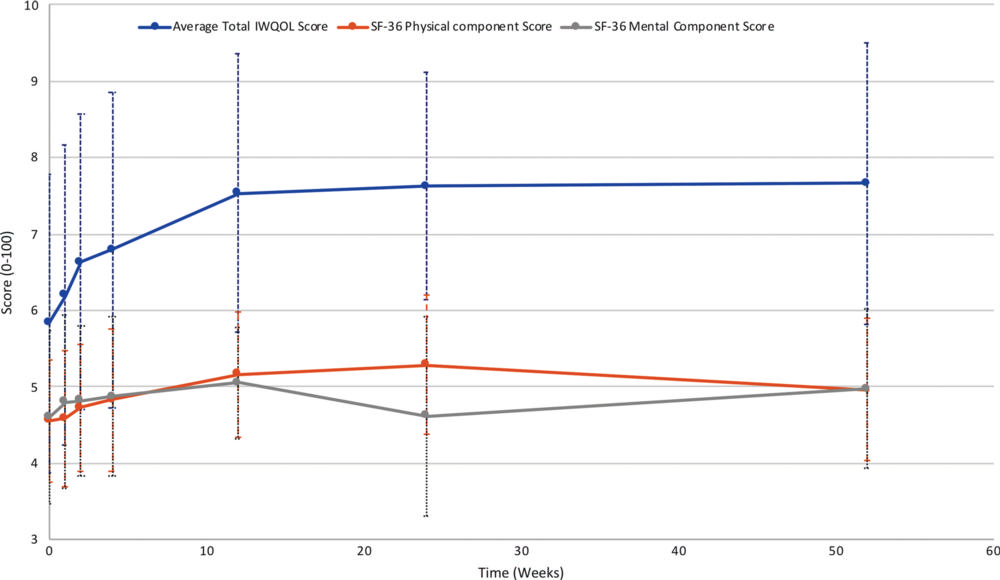
Figure 6. Quality-of-life (QOL) measures. The Short Form-36 (SF-36) health questionnaire is scored from 1 percent–100 percent, with a national average of 50 percent. Impact of Weight on Quality of Life (IWQOL) is reported as points out of 100.
High-res (TIF) version
(Right-click and Save As)
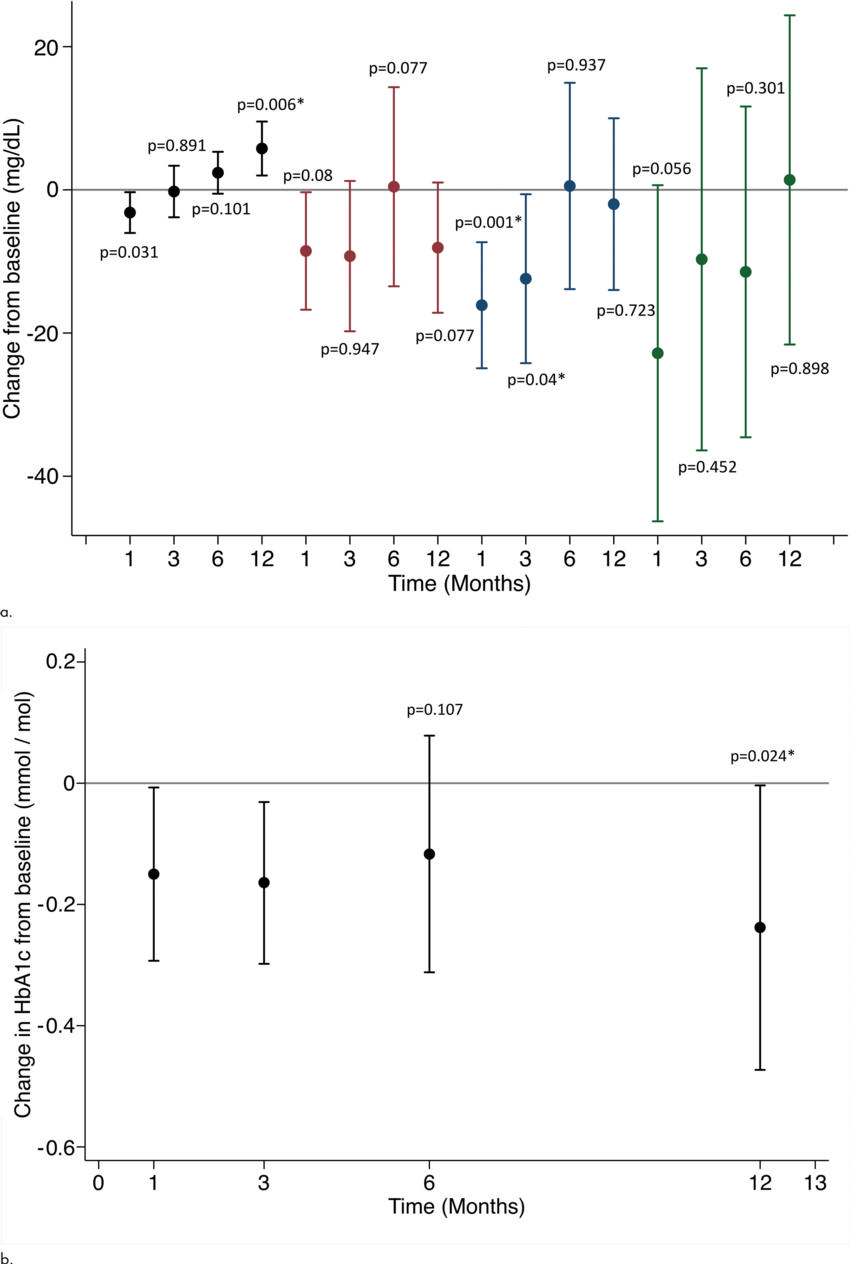
Figure 7. Changes in laboratory values over time. * indicates statistical significance. (a) Mean changes in lipids over time. High-density lipoprotein (black), low-density lipoprotein (red), total cholesterol (blue), triglycerides (green). (b) Changes in hemoglobin A1c (HbA1c) over time.
High-res (TIF) version
(Right-click and Save As)
