Noninvasive Imaging Helps Predict Heart Attacks
Released: March 14, 2017
At A Glance
- Noninvasive CT angiography and stress tests can help predict which patients are likely to suffer a heart attack or other adverse cardiovascular event.
- Invasive and noninvasive approaches were compared in 379 patients who were referred for invasive coronary angiography.
- Researchers found that both techniques are equally effective in identifying which patients will have a future major adverse cardiac event.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — Noninvasive CT angiography and stress tests can help predict which patients are likely to suffer a heart attack or other adverse cardiovascular event, according to a new study appearing online in the journal Radiology.
Cardiovascular disease is a leading cause of death worldwide. Bypass surgery or stent placement is often recommended in people with certain degrees of coronary arterial narrowing, or stenosis, but recent studies have shown that many of these patients do just as well with medical therapy. A key factor in treatment decisions is the hemodynamic significance of the lesion, meaning the degree to which the lesion is blocking blood from getting to areas of the heart.
“Previous studies show that a lesion is hemodynamically significant if there is a significant blood pressure drop corresponding to a big reduction in blood flow across the stenosis,” said study author João A.C. Lima, M.D., from Johns Hopkins Hospital and School of Medicine in Baltimore. “If plaque has those characteristics, the patient should be targeted for intervention, be it with a stent or downstream bypass surgery.”
A combination of invasive coronary angiography (ICA) and stress tests with single photon emission tomography (SPECT) myocardial imaging has been the gold standard for making these determinations, with ICA showing the blockages and SPECT the perfusion, or penetration of the blood into the tissue. However, ICA requires the use of a catheter that is threaded from a puncture point in the groin all the way up to the heart.
“Invasive angiography is generally safe, but it can cause vascular problems in a significant number of patients, most commonly at site of the puncture,” Dr. Lima said. “In rare cases, it can cause strokes or heart attacks. These risks are not trivial.”
The ICA/SPECT approach can also be expensive, as it often necessitates hospitalization for the patient.
“The traditional approach with invasive catheterization requires that patients go to the hospital, get a catheter inserted into their leg and go in for the nuclear SPECT study on a different day,” said study coauthor Marcus Chen, M.D., from the National Institutes of Health in Bethesda, Md. “Now with just one noninvasive test we can get two important but different pieces of information about the coronary arteries.”
The researchers set out to determine if combined CT angiography (CTA) and CT myocardial stress perfusion imaging (CTP) could demonstrate similar or superior ability to ICA/SPECT in predicting future adverse events.
They compared the invasive and noninvasive approaches in 379 patients who were referred for ICA from November 2009 to July 2011. The researchers looked at the ability of both techniques to predict whether or not a future major adverse cardiac event (MACE), such as a heart attack, revascularization, arrhythmia or hospitalization for chest pain or congestive heart failure would occur.
Fifty-one patients, or 13.5 percent, experienced one or more major adverse cardiac events, including 49 revascularizations, five myocardial infarctions, one cardiac death, nine hospitalizations for chest pain or congestive heart failure, and one arrhythmia.
Both techniques proved to have similarly high values for predicting MACE at two years after presentation and event-free survival. The two-year MACE-free rates for combined CT angiography and CT perfusion findings were 94 percent negative for coronary artery disease (CAD) versus 82 percent positive for CAD and were similar to combined ICA/SPECT findings (93 percent negative for CAD vs. 77 percent positive for CAD).
“The key finding of our study is that both techniques are equally effective in identifying which patients are going to have trouble down the road,” Dr. Lima said. “The noninvasive option should be a preferred or at least strongly considered option by cardiologists and radiologists managing these patients because it is safer and less expensive, and patients like it better.”
Obstacles remain before the noninvasive approach can achieve more widespread use, including the lack of a reimbursement code for stress CT perfusion. But the study indicates that the technique is relatively easy to incorporate into existing practices: 15 of the 16 centers in the trial had never done the procedure before, according to Dr. Chen, and all were all able to learn it effectively.
“Prognostic Value of Combined CT Angiography and Myocardial Perfusion Imaging versus Invasive Coronary Angiography and Nuclear Stress Perfusion Imaging in the Prediction of Major Adverse Cardiovascular Events: The CORE320 Multicenter Study.” Collaborating with Dr. Lima were Marcus Y. Chen, M.D., Carlos E. Rochitte, M.D., Ph.D., Armin Arbab-Zadeh, M.D., M.P.H., Ph.D., Marc Dewey, M.D., Ph.D., Richard T. George, M.D., Julie M. Miller, M.D., Hiroyuki Niinuma, M.D., Ph.D., Kunihiro Yoshioka, M.D., Ph.D., Kakuya Kitagawa, M.D., Hajime Sakuma, M.D., Ph.D., Roger Laham, M.D., Andrea L. Vavere, M.S., M.P.H., Rodrigo J. Cerci, M.D., Vishal C. Mehra, M.D., Ph.D., Cesar Nomura, M.D., Klaus F. Kofoed, M.D., Masahiro Jinzaki, M.D., Sachio Kuribayashi, M.D., Arthur J. Scholte, M.D., Michael Laule, M.D., Swee Yaw Tan, M.D., John Hoe, M.D., Narinder Paul, M.D., Frank J. Rybicki, M.D., Jeffrey A. Brinker, M.D., Andrew E. Arai, M.D., Matthew B. Matheson, M.S., Christopher Cox, Ph.D., Melvin E. Clouse, M.D., and Marcelo F. Di Carli, M.D., for the CORE320 Investigators.
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of over 54,600 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on cardiovascular imaging, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
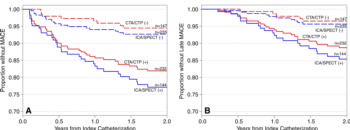
Figure 1. Kaplan-Meier survival curves used to predict major adverse cardiovascular event (MACE) (composite end point of late revascularization [˃30 days], myocardial infarction, cardiac death, arrhythmia, and hospitalization for chest pain or congestive heart failure) and late MACE (composite end point of late revascularization [˃182 days], myocardial infarction, cardiac death, arrhythmia, and hospitalization for chest pain or congestive heart failure) at 2 years after index cardiac catheterization. A, MACE survival curves for patients with and those without hemodynamically obstructive coronary artery disease (CAD) at combined CT angiography and CT perfusion (CTA /CTP) and combined invasive coronary angiography (ICA) and single photon emission CT (ICA /SPECT ). B, Late MACE survival curves in patients with and in those without hemodynamically obstructive CAD at CT angiography and CT perfusion and at ICA and single photon emission CT.
High-res (TIF) version
(Right-click and Save As)
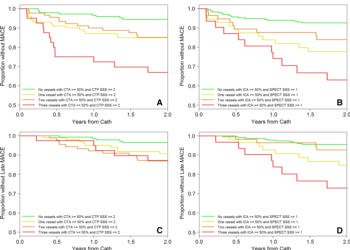
Figure 2. Kaplan-Meier survival curves used to predict major adverse cardiovascular event (MACE) (composite end point of late revascularization [˃30 days], myocardial infarction, cardiac death, arrhythmia, and hospitalization for chest pain or congestive heart failure) and late MACE (composite end point of late revascularization [˃182 days], myocardial infarction, cardiac death, arrhythmia, and hospitalization for chest pain or congestive heart failure) at 2 years after index cardiac catheterization. A, Survival curves for combined CT angiography and CT perfusion in patients without hemodynamically obstructive coronary artery disease (CAD) and in those with one, two, or three vessels with hemodynamically obstructive CAD. B, Survival curves for combined invasive coronary angiography (ICA) and single photon emission CT myocardial perfusion in patients without hemodynamically obstructive CAD and in those with one, two, or three vessels with hemodynamically obstructive CAD. C, Survival curves for combined CT angiography and myocardial perfusion in patients without hemodynamically obstructive CAD and in those with one, two, or three vessels with hemodynamically obstructive CAD. D, Survival curves for combined ICA and single photon emission CT myocardial perfusion in patients without hemodynamically obstructive CAD and in those with one, two, or three vessels with hemodynamically obstructive CAD.
High-res (TIF) version
(Right-click and Save As)
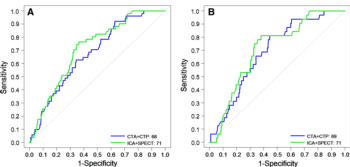
Figure 3. Receiver operating characteristic curves for combined CT angiography and myocardial perfusion imaging (CTA+CTP) and combined ICA and single photon emission computed tomography (ICA+SPECT ) used to predict, A, major adverse cardiovascular event (MACE) (composite end point of late revascularization [˃30 days], myocardial infarction, cardiac death, arrhythmia, or hospitalization for chest pain or congestive heart failure) at 2-year follow-up or, B, late MACE (composite end point of late revascularization [˃182 days], myocardial infarction, cardiac death, arrhythmia, or hospitalization for chest pain or congestive heart failure) at 2-year follow-up.
High-res (TIF) version
(Right-click and Save As)