RSNA Press Release
- Evaluation of the emergency radiology response to the Boston Marathon bombings highlights the crucial role medical imaging plays in emergency situations.
- Of the 40 wounded patients received at Brigham and Women’s Hospital, which is a Level 1 trauma center, 31 patients (78 percent) underwent imaging.
- After-action review identified opportunities to improve preparedness for potential future mass casualty events.
Researchers Assess Emergency Radiology Response after Boston Marathon Bombings
Released: July 15, 2014
| Media Contacts: | |
| RSNA Media Relations: | 1-630-590-7762 |
| Linda Brooks 1-630-590-7738 lbrooks@rsna.org |
Maureen Morley 1-630-590-7754 mmorley@rsna.org |
OAK BROOK, Ill. – An after-action review of the Brigham and Women's Hospital emergency radiology response to the Boston Marathon bombings highlights the crucial role medical imaging plays in emergency situations and ways in which radiology departments can improve their preparedness for mass casualty events. The new study is published online in the journal Radiology.
"It's important to analyze our response to events like the Boston Marathon bombing to identify opportunities for improvement in our institutional emergency operations plan," said senior author Aaron Sodickson M.D., Ph.D., emergency radiology director at Brigham and Women's Hospital.
Lead researcher John Brunner, M.D., was an emergency radiology fellow working in the Brigham and Women's Emergency Department on April 15, 2013, when two bombs detonated near the finish line of the Boston Marathon. As a Level 1 trauma center, the hospital received 40 of the wounded patients, most within hours of the bombing.
"Imaging is one of the best ways to decide who needs attention most quickly," Dr. Brunner said. "The use of shrapnel-laden explosive devices resulted in extensive shrapnel injuries that required evaluation with X-ray and computed tomography, or CT."
Of the 40 patients who arrived in the emergency department for care, 31 patients (78 percent) underwent imaging, including 57 X-rays performed on 30 patients and 16 CT scans of seven patients.
Additional staff were rapidly mobilized, including attending radiologists, radiology fellows and residents, and x-ray and CT technologists. In addition, the usual emergency radiology imaging equipment (two portable X-ray machines and two fixed digital X-ray units, an ultrasound machine and a CT scanner) were supplemented with additional imaging machines from elsewhere in the hospital, including two additional CT scanners and additional portable X-ray units.
The researchers studied the emergency radiology response by comparing turnaround times — or the amount of time taken to perform exams and to interpret the results — from routine emergency radiology operations with those during the mass casualty event. CT exam turnaround time averaged 37 minutes during the mass casualty event, significantly lower than the annual median of 72 minutes during routine operations. The researchers said the fast turnaround was likely the result of having access to three CT scanners and stationing a radiologist at each.
By contrast, the researchers found the X-ray turnaround time (median, 52 minutes) was longer than during routine operations (31 minutes), most likely due to a bottleneck created by the use of conventional radiography portable X-ray machines relying on a single x-ray plate readout device. To eliminate this technical bottleneck, these portable X-ray units have since been replaced by digital radiography equipment with wireless image transfer to enable faster exam completion and image availability.
"Imaging plays a vital role in all emergent situations, from everyday Emergency Department visits and trauma to mass casualty events," Dr. Sodickson said. "The surge in imaging utilization following the Boston Marathon bombing stressed emergency radiology operations but overall, things went smoothly in terms of patient care."
During the mass casualty event, the hospital's system for naming unidentified patients contributed to a large number of duplicative imaging orders and has since been overhauled. The new system, which includes a combination of a unique color, gender and numeral, (e.g. Crimson Male 12345) will reduce confusion that accompanied the influx of multiple patients following the Boston Marathon bombings.
"Hospitals need to have emergency operations plans in place, and emergency radiology is a crucial component of that preparedness," Dr. Sodickson said. "When an event occurs, it is important to direct a critical eye to the plan's operation in order to refine it for the future."
# # #
"The Boston Marathon Bombing: After-Action Review of the Brigham and Women's Hospital Emergency Radiology Response." Collaborating with Drs. Sodickson and Brunner were Tatiana Rocha, M.D., Avni A. Chudgar, M.D., Eric Goralnick M.D., Joaquim M. Havens, M.D., and Ali S. Raja, M.D., M.B.A., M.P.H. Study abstract
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (Radiology.RSNA.org/)
RSNA is an association of more than 53,000 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on X-ray and CT, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
 Figure 1. Images in a victim who sustained multiple shrapnel-related secondary blast injuries. (a) X-ray of the left lower extremity reveals the bone in many pieces in the left tibia and fibula with metallic objects (arrow) that were determined to be pressure cooker fragments. (b) Coronal and (c) axial images from the CT angio¬graphic examination show early vein opaqueness within the left peroneal and popliteal veins (arrow) during the arterial phase, which indicated traumatic arteriovenous fistula. A metallic foreign body and soft tissue gas bubbles are seen in the distal calf (b). High-res (TIF) version (Right-click and Save As) |
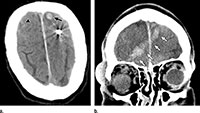 Figure 2. Images in a victim who sustained penetrating neurologic trauma from a ball bearing. (a) CT examination of the head reveals a spherical metallic object, determined to be a ball bearing, lodged in the left frontal lobe. Image also shows bleeding in the area between the brain and the thin tissues that cover the brain—subarachnoid hemorrhage (arrowhead)—and blood pooling in the brain, intrapa-renchymal hemorrhage (arrow). The ball bearing entered the right frontal cortex and crossed the midline. Image (b) shows intracranial hemorrhage along the ball bearing’s path from the right orbit through the right frontal lobe to the left frontal lobe (arrows). This patient did not undergo surgery. High-res (TIF) version (Right-click and Save As) |
 Figure 3. Tie plot of each imaging order and process steps within the first 10 hours of the bomb blasts, including (a) radiography and (b) CT orders. Two examinations ordered for a patient during hour 23 are excluded from the graph to permit improved visualization of the x-axis. High-res (TIF) version (Right-click and Save As) |
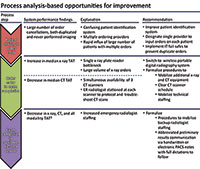 Figure 4. Key findings of process evaluation with summarized explanation and recommendations for improving future performance. Not statistically significant, but explainable variations in performance. PACS = picture archiving and communication system, TAT = turnaround time. High-res (TIF) version (Right-click and Save As) |

 PDF
PDF