RSNA Press Release
- Cerebral aneurysms of all sizes are twelve times more likely to rupture if they are growing in size.
- These findings dispute current guidelines stating that aneurysms less than seven millimeters in size have a low risk of rupture and do not need to be monitored.
- Each year in the U.S., approximately 30,000 people have a ruptured brain aneurysm.
Growth in Cerebral Aneurysms Increases Risk of Rupture
Released: July 2, 2013
| Media Contacts: | |
| RSNA Media Relations: | 1-630-590-7762 |
| Linda Brooks 1-630-590-7738 lbrooks@rsna.org |
Maureen Morley 1-630-590-7754 mmorley@rsna.org |
OAK BROOK, Ill. — Cerebral aneurysms of all sizes—even small ones below seven millimeters—are 12 times more likely to rupture if they are growing in size, according to a new study published online in the journal Radiology.
A cerebral aneurysm is a balloon-like bulge in a weakened blood vessel in the brain. If an aneurysm ruptures, blood is leaked into or around the brain, which can cause brain damage or death.
According to The Brain Aneurysm Foundation, an estimated 6 million people in the United States have an unruptured brain aneurysm, or 1 in 50 people. Ruptured brain aneurysms occur in approximately 30,000 Americans each year and are fatal in about 40 percent of cases. Of those who survive, about two-thirds suffer some permanent neurological deficit.
"Given what a devastating event a ruptured brain aneurysm is, we are very motivated to identify the real risk factors for rupture," said the study's lead author, J. Pablo Villablanca, M.D., chief of diagnostic neuroradiology at the David Geffen School of Medicine at the University of California, Los Angeles.
In Dr. Villablanca's study, 258 asymptomatic cerebral aneurysms identified either incidentally or during a baseline study of 165 patients (132 women, 33 men) were monitored over time (mean of 2.24 years) with computed tomography angiography (CTA), a noninvasive imaging study of the brain's blood vessels. Patients were scanned with CTA at intervals of six or 12 months.
Over the study period, the researchers observed growth in 46 or nearly 18 percent of all the intracranial aneurysms in a total of 38 patients. Three of the 39 growing saccular aneurysms ruptured, and of those, all were less than seven millimeters in size at study entry.
"Our study shows that the size of the aneurysm is not as important as was once thought," Dr. Villablanca said. "Any aneurysm is potentially capable of growth and thus requires follow-up imaging."
Current guidelines based on research conducted by the International Study of Unruptured Intracranial Aneurysms and other studies suggest that known aneurysms less than seven millimeters in size have a low risk of rupture and do not need to be monitored with imaging.
Compared to the aneurysms that stayed the same size, the 46 growing aneurysms in the study were associated with a 12-fold higher risk of rupture. The researchers calculated the risk of rupture for growing aneurysms at 2.4 percent per patient-year, versus 0.2 percent for aneurysms without growth.
"Our data support the need to perform longitudinal follow-up imaging to monitor for possible growth in all incidental unruptured aneurysms, including small lesions," Dr. Villablanca said.
The researchers also found that tobacco smoking and the initial size of the aneurysm were independent predictors of aneurysm growth. Together, these risk factors were associated with 78.4 percent of all aneurysm growth in the study.
"The positive association between aneurysm growth, aneurysm size, and cigarette smoking suggests that the combination of these factors are associated with an increased risk of rupture and may influence the need for therapeutic intervention," Dr. Villablanca said.
Observation was the treatment of choice for 194 of 212 (91 percent) stable aneurysms. When aneurysm growth was discovered by CTA imaging, 50 percent of the growing aneurysms were treated, while the remaining 50 percent continued to be observed.
# # #
"The Natural History of Asymptomatic Unruptured Cerebral Aneurysms Evaluated at CT Angiography: Growth and Rupture Incidence and Correlation with Epidemiologic Risk Factors." Collaborating with Dr. Villablanca were Gary R. Duckwiler, M.D., Reza Jahan, M.D., Satoshi Tateshima, M.D., Ph.D., Neil A. Martin, M.D., John Frazee, M.D., Nestor R. Gonzalez, M.D., James Sayre, Ph.D., and Fernando V. Vinuela, M.D.
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of more than 51,000 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on Computed Tomography Angiography (CTA), visit RadiologyInfo.org.
Images
 Figure 1 Frontal projection three-dimensional volume-rendered images with anteroposterior projection in a 48-year-old woman with small saccular basilar tip aneurysm that arose from small contour deformity located at basilar tip. (a) Image shows minor contour deformity at basilar tip. (b) Image shows interval development of wide-necked 3.2-mm maximal-diameter aneurysm projecting superiorly from basilar tip. Scan interval was 9 months and 3 weeks. High-res (TIF) version (Right-click and Save As) |
 Figure 2 Craniocaudad projection image shows 60 year-old woman with saccular anterior communicating aneurysm exhibiting unidimensional growth at dome. Anteroposterior 3 transverse 3 craniocaudad aneurysm size (4.4 mm X 2.9 mm X 3.2 mm) was stable (within measurement error) from (a) November 15, 2001; through (b) February 21, 2002, and August 16, 2002 (not shown). During third year of observation, lesion underwent measurable and visible growth at dome region (7 mm X 2.8 mm X 3.2 mm) shown on (c) image from Sep¬tember 4, 2003. Patient underwent successful coil embolization on November 5, 2003. High-res (TIF) version (Right-click and Save As) |
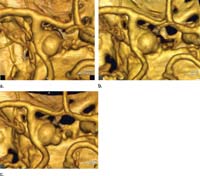 Figure 3 Targeted volume-rendered three-dimensional images from above left cavernous carotid bifurcation region in 72-year-old woman with saccular aneurysm of left supraclinoid internal carotid artery show bleb development with comparatively stable sac size. (a) October 17, 2000: Image shows saccular aneurysm (anteroposterior X transverse X craniocaudad, 5.9 mm X 7.1 mm X 7.9 mm) with barely perceptible medial deformity of sac wall. (b) November 29, 2001: Image shows clearly visible small aneurysm bleb. (c) October 29, 2002: Image shows prominent growth of medial bleb and com-paratively stable sac size (8.3 mm X 7.2 mm X 8.5 mm). Patient underwent successful neurosurgical clip placement before rupture on December 30, 2002. High-res (TIF) version (Right-click and Save As) |
 Figure 4 Volume-rendered three-dimensional CT angiographic image with superior to inferior projection and posterolateral perspective in a 77-year-old woman with asymptomatic 5.8-mm saccular basilar tip aneurysm shows rapid and eccentric growth at dome before rupture. (a) Patient was scheduled for 6-month follow-up scan, but pre¬sented at 4 months with subarachnoid hemorrhage due to rupture of lesion. (b) At time of rupture, lesion had grown to maximal diameter of 6.6 mm with substantial posteriorly directed eccentric growth at dome region and 50% increase in sac volume. High-res (TIF) version (Right-click and Save As) |

 PDF
PDF