New Study Shows Increase in Domestic Violence Injuries during COVID-19
Released: August 13, 2020
At A Glance
- The incidence and severity of physical intimate partner violence (IPV) increased during the COVID-19 pandemic.
- The number of injuries to deep internal organs during the pandemic period of observation was 28 compared to a total of 16 during the prior 3 years.
- The role of radiologists in identifying victims of IPV through imaging exams has become crucial due to social distancing.
- RSNA Media Relations
1-630-590-7762
media@rsna.org
OAK BROOK, Ill. — There was a higher incidence and severity of physical intimate partner violence (IPV) among patients seen at a large, academic medical center in the U.S. during the COVID-19 pandemic compared with the prior three years, according to a new study published in Radiology.
“Our study showed a higher incidence of physical IPV, both in absolute numbers and proportion, with more severe injuries despite fewer patients reporting IPV,” said Bharti Khurana, M.D., principal investigator and director of the Trauma Imaging Research and Innovation Center at Brigham and Women’s Hospital in Boston, Massachusetts. “This indicates that victims are reporting to health care facilities in the late stages of the abuse cycle. Fear of contracting infection and closure of ambulatory sites might be preventing victims of mild physical or emotional abuse from seeking help compared to the pre-pandemic era.”
Social distancing has proven to be effective for controlling the spread of coronavirus but with negative socioeconomic and psychological impacts. Service-oriented economies have seen increased unemployment and a higher incidence of substance and alcohol abuse and mental health disorders.
Since the outbreak of COVID-19, reports of IPV have increased worldwide during mandatory “lockdowns” to curb the spread of the virus.
Dr. Khurana and colleagues set out to assess the incidence, pattern and severity of injuries related to IPV at Brigham and Women’s Hospital during COVID-19 pandemic. The demographics, clinical presentation, injuries and radiological findings of patients reporting physical abuse arising from IPV between March 11 and May 3, 2020, were compared with the same period over the past three years.
Data from 26 physical IPV victims from 2020 (37+/-13 years, 25 women) were evaluated and compared with 42 physical IPV victims (41+/-15 years, 40 women) from 2017 to 2019. While the overall number of patients reporting IPV was lower, the incidence of physical IPV was 1.8 times greater during the pandemic. Five victims of severe abuse were identified in 2020 (5/26=19%) compared to one each of the previous years.
The total number of deep injuries (injuries to deep internal organs) was 28 during 2020 versus 16 from 2017 to 2019. The number of deep injuries per victim was 1.1 during 2020 compared with 0.4 from 2017 to 2019. The incidence of high-risk abuse defined by mechanism (injuries due to strangulation, stab injuries, burns or use of weapons such as knives, guns and other objects that could inflict deep injuries) was 2 times greater. Patients with IPV during the COVID-19 pandemic were more likely to be ethnically white. Seventeen (65%) victims in 2020 were white, compared to 11 (26%) in the prior years.
“During the pandemic, victims experienced more injuries to the chest and abdomen compared to prior years,” said coauthor Babina Gosangi, M.D., assistant professor of radiology at Yale New Haven Health in New Haven, Connecticut, and former emergency radiology fellow at Brigham and Women’s Hospital. “For instance, one victim sustained multiple bilateral rib fractures with right pneumothorax and bilateral lung contusions—requiring hospital admission for more than 10 days—after she was repeatedly punched in the chest. Another victim was stabbed in the abdomen and had lacerations to the liver and kidney.”
It is challenging to help IPV victims in the time of the pandemic when health care providers are overwhelmed by COVID-19 patients. In addition, alternative options for IPV victims to seek help have decreased. Many ambulatory clinics are no longer seeing as many patients in person due to the virus and are instead pivoting their services to virtual consultation. Telehealth visits limit the opportunity to visualize bruises or other signs of physical trauma and hamper the ability of the health care provider to gather nonverbal cues.
It may also be difficult for victims who are at home to report IPV, and health care providers may be omitting IPV screening questions altogether on these calls due to patient’s limited privacy. Therefore, the role of radiologists in identifying victims of IPV through imaging exams has become crucial.
By recognizing high imaging utilization, location and imaging patterns specific to IPV, old injuries of different body parts, and injuries inconsistent to provided history, radiologists can identify victims of IPV even when the victims are not forthcoming.
Dr. Khurana, who is also assistant professor of radiology at Harvard Medical School in Boston, sees this as an opportunity for radiologists to use their expertise in providing patient-centered care and play a critical role in facilitating early intervention, preventing life-threatening injuries and saving lives by early identification of IPV victims.
“As health care providers, we are missing opportunities to identify victims early in the cycle during the pandemic,” she said. “There is under-reporting by the victims, accentuated due to fear of seeking care due to COVID-19. At the same time, IPV-related injuries may be getting overlooked or misinterpreted, as our frontline physicians are overwhelmed by a vast number of COVID-19 patients in the Emergency Department.”
The researchers emphasize that radiologists and other health care providers should proactively participate in identifying IPV victims and reaching out to vulnerable communities as an essential service during the pandemic and other crisis situations.
“Exacerbation of Physical Intimate Partner Violence during COVID-19 Lockdown” Collaborating with Drs. Khurana and Gosangi on this paper were Hyesun Park, M.D., Richard Thomas, M.D., Rahul Gujrathi, M.D., Camden P. Bay, Ph.D., Ali S. Raja, M.D., Steven E. Seltzer, M.D., Marta Chadwick Balcom, J.D., Meghan L. McDonald, R.N., Dennis P. Orgill, M.D., Ph.D., Mitchel B. Harris, M.D., Giles W. Boland, M.D., and Kathryn Rexrode, M.D. The study was partially funded by a Stepping Strong Injury Prevention Innovation award.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, and owned and published by the Radiological Society of North America, Inc. (https://pubs.rsna.org/journal/radiology)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
For patient-friendly information on medical imaging, visit RadiologyInfo.org.
Press Resources:
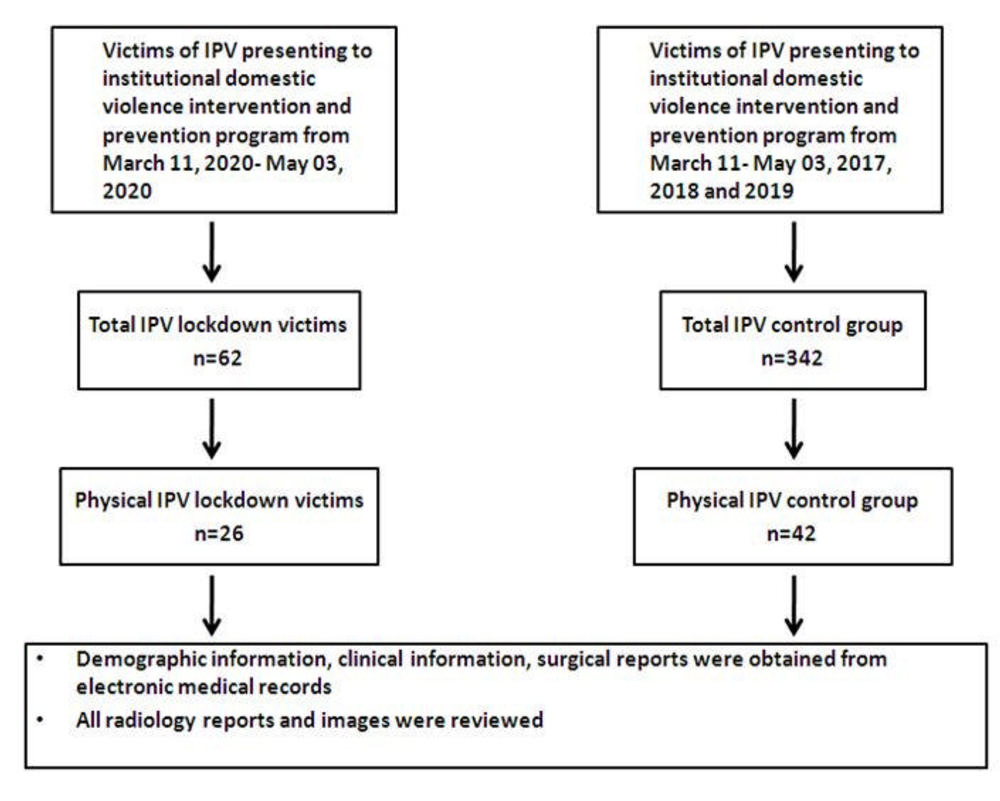
Figure 1. Flowchart of the COVID-19 pandemic victims and control groups.
High-res (TIF) version
(Right-click and Save As)
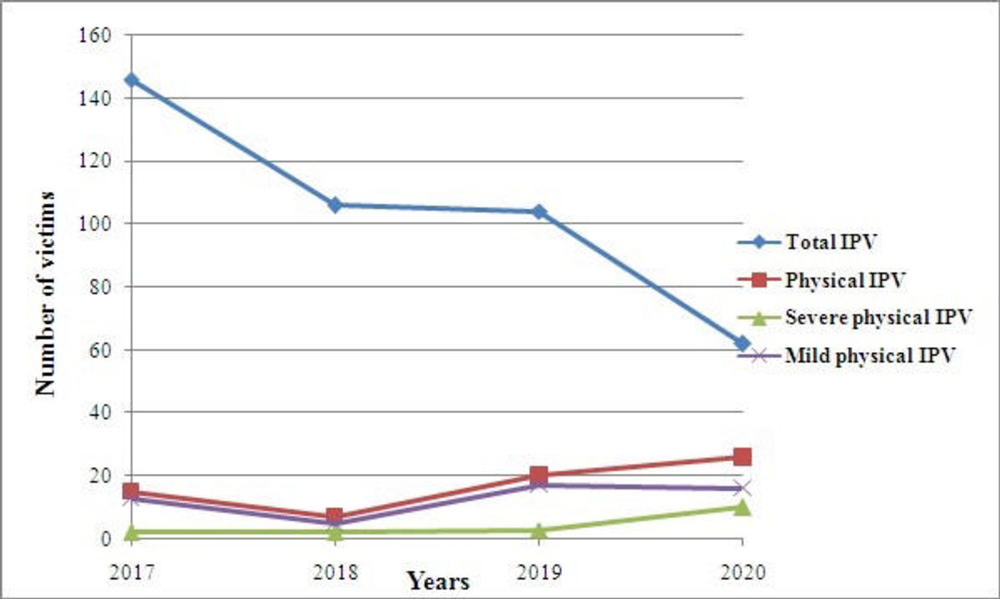
Figure 2. Graph illustrates year-wise comparison of total intimate partner violence (IPV), physical intimate partner violence (IPV), severe and mild grades of physical intimate partner violence (IPV).
High-res (TIF) version
(Right-click and Save As)
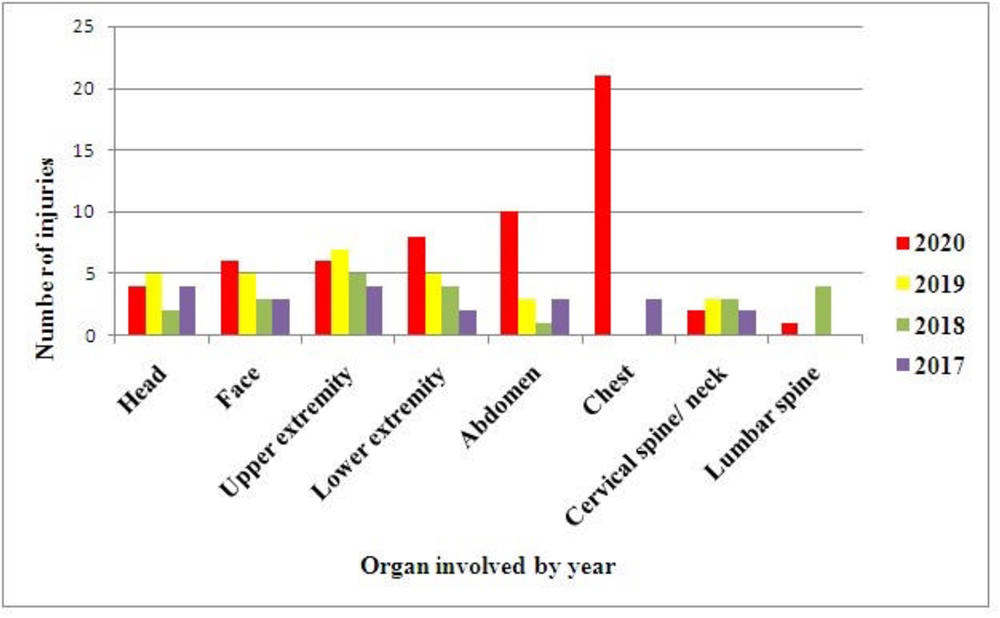
Figure 3. Graph illustrates organ wise injuries for victims of intimate partner violence (IPV) based on the year.
High-res (TIF) version
(Right-click and Save As)
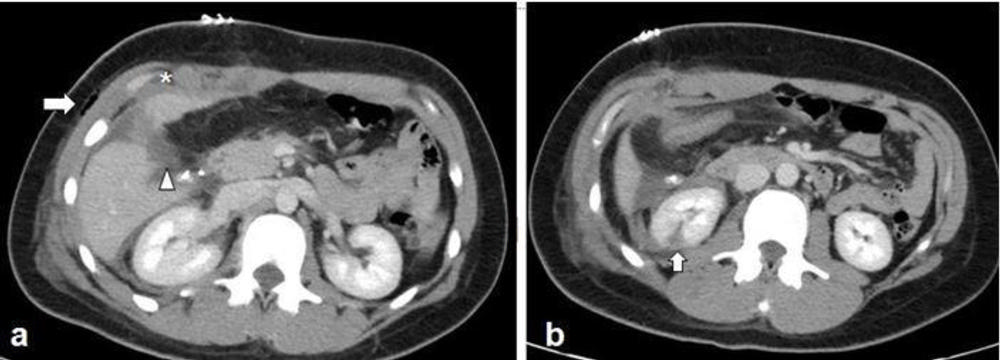
Figure 4. Images in a 27-year-old female victim who was stabbed in the right mid abdomen by her boyfriend. (a) Axial abdomen CT scan demonstrates an AAST (American Association for the Surgery of Trauma) grade 2 liver laceration (arrowhead) with a small perihepatic hematoma (asterisk), and subcutaneous emphysema (arrow) at the site of stab injury. (b) Additional axial CT abdomen image demonstrated irregular hypoattenuation in the inferior aspect of left kidney, representing an AAST grade 2 laceration. The patient underwent surgical repair of liver laceration and cholecystectomy. The renal injury was managed conservatively.
High-res (TIF) version
(Right-click and Save As)
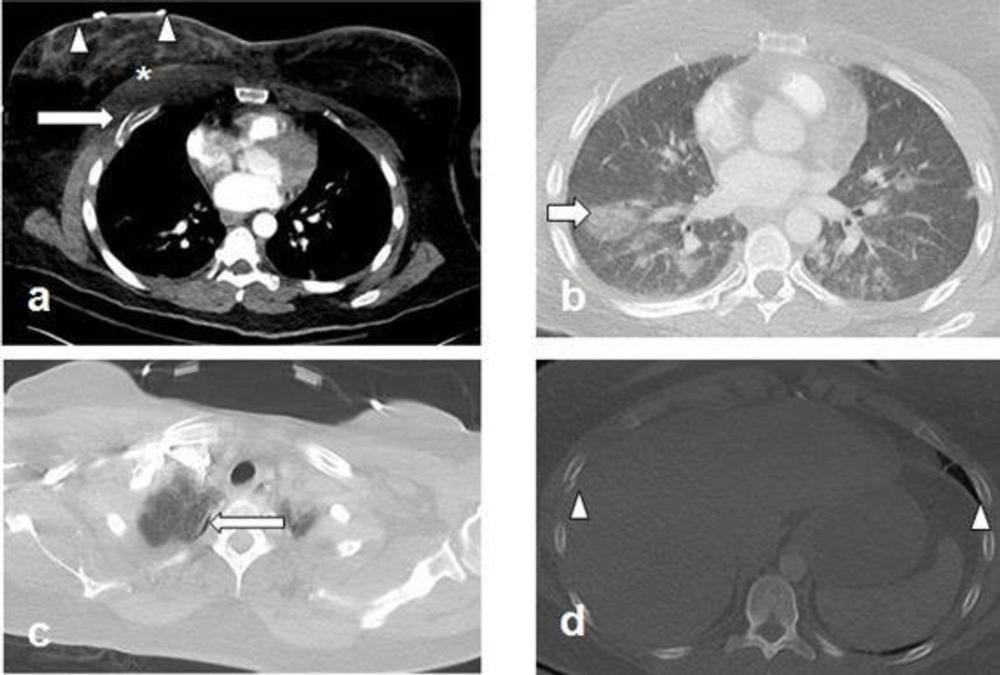
Figure 5. Images in a 38- year-old female victim struck in the face and chest by her boyfriend. The patient sustained multiple right sided rib fractures. (a) Axial post contrast chest CT demonstrates a comminuted right fourth rib fracture (arrow), extensive swelling of right breast (arrowheads) and anterior chest wall muscle (asterisk), suggesting contusion and intramuscular hematoma. (b) Ground-glass opacity in the right lung peripherally suggestive of lung contusion (arrow). (c) Additional chest CT image through apices on lung window demonstrates trace right apical pneumothorax (arrow). (d) Bilateral rib fractures (arrowheads).
High-res (TIF) version
(Right-click and Save As)
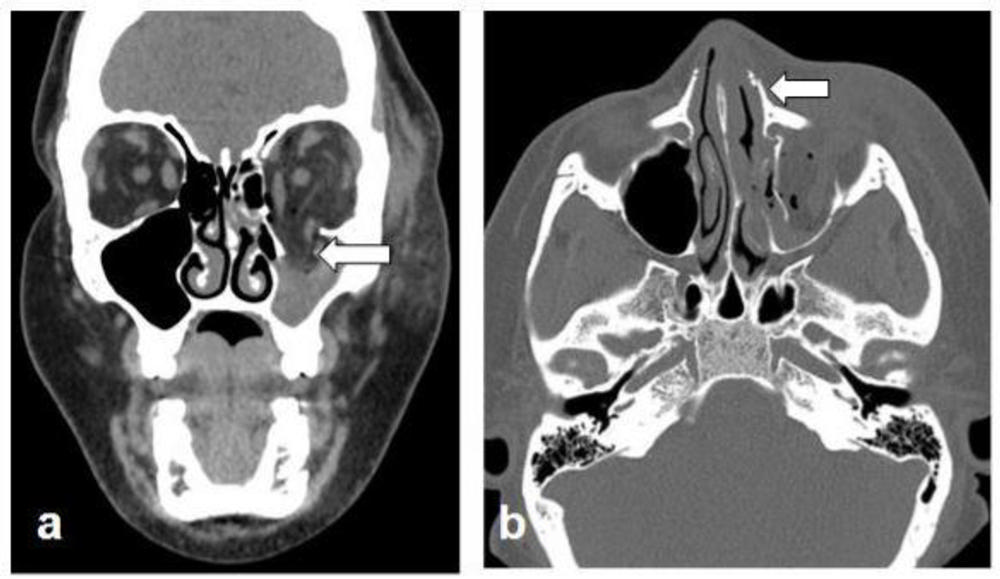
Figure 6. Images in a 35-year-old female victim who was strangulated and hit in the face multiple times by her boyfriend. (a) Coronal reconstructed non-contrast face CT demonstrates acute comminuted inferiorly displaced fracture of the left inferomedial orbital wall (arrow), with herniation of fat and inferior rectus muscle into the left maxillary sinus. Asymmetric subcutaneous swelling is noted on the left. (b) Axial face CT image demonstrates a minimally displaced left nasal bone fracture (arrow). The patient underwent surgical repair of the left orbital wall.
High-res (TIF) version
(Right-click and Save As)

