Multi-Institutional Study Looks at Brain MRI Findings in COVID-19
Released: June 16, 2020
At A Glance
- Brain findings in COVID-19 patients from 16 hospitals showed three distinct patterns.
- A majority of patients had intracerebral hemorrhagic lesions, which were associated with worse clinical status.
- SARS-CoV-2 RNA was detected in the cerebrospinal fluid in only one of 37 patients.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org - Dionna Arnold
1-630-590-7791
darnold@rsna.org
OAK BROOK, Ill. (June 16, 2020) — A new multi-institutional study published in the journal Radiology identifies patterns in abnormal brain MRI findings in patients with COVID-19.
Current data on central nervous system (CNS) involvement in COVID-19 is uncommon but growing, demonstrating a high frequency of neurological symptoms. However, the delineation of a large cohort of confirmed brain MRI abnormalities (excluding ischemic infarcts) related to COVID-19 has never been performed, and the underlying pathophysiological mechanisms remain unknown.
The purpose of this current study was to describe the neuroimaging findings other than stroke in patients with severe COVID-19 and report the clinical and biological profile of these patients.
The retrospective observational national multicenter study was initiated by the French Society of Neuroradiology (SFNR) in collaboration with neurologists, intensivists and infectious disease specialists. Consecutive patients with COVID-19 infection and neurologic manifestations who underwent brain MRI from March 23 to April 27, 2020, in 16 French centers, including 11 university hospitals and five general hospitals were included in the study.
Thirty men (81%) and 7 women (19%) met inclusion criteria, with a mean age of 61 years. The most common neurologic manifestations were alteration of consciousness (27/37, 73%), pathological wakefulness when the sedation was stopped (15/37, 41%), confusion (12/37, 32%) and agitation (7/37, 19%).
Among the 37 patients included, 28/37 (76%) were associated with one neuroimaging pattern, 7/37 (19%) with two patterns, and 2/37 (5%) showed three patterns. The most frequent MRI findings were: signal abnormalities located in the medial temporal lobe in 16/37 (43%) patients, non-confluent multifocal white matter hyperintense lesions on FLAIR and diffusion sequences, with variable enhancement, with associated hemorrhagic lesions in 11/37 patients (30%), and extensive and isolated white matter microhemorrhages in 9/37 patients (24%).
A majority of patients (20/37, 54%) had intracerebral hemorrhagic lesions and a more severe clinical presentation.
“Three main neuroradiological patterns could be distinguished, and the presence of hemorrhage was associated with worse clinical status. SARS-CoV-2 RNA was detected in the cerebrospinal fluid in only one patient, and the underlying mechanisms of brain involvement remain unclear,” the authors wrote. “Imaging and neurological follow up has to be undertaken in order to evaluate the prognosis of these patients.”
RSNA is committed to connecting radiologists and the radiology community to the most timely and useful COVID-19 information and resources. RSNA’s COVID-19 Resources page houses the latest guidance, original research, image collection and more. The page will be updated on an ongoing basis.
“Brain MRI Findings in Severe COVID-19: A Retrospective Observational Study.” Stéphane Kremer, M.D., François Lersy, M.D., Jérome de Sèze, M.D., Jean-Christophe Ferré, M.D., Adel Maamar, M.D., Béatrice Carsin-Nicol, M.D., Olivier Collange, M.D., Fabrice Bonneville, M.D., Gilles Adam, M.D., Guillaume Martin-Blondel, M.D., Marie Rafiq, M.D., Thomas Geeraerts, M.D., Louis Delamarre, M.D., Sylvie Grand, M.D., Alexandre Krainik, M.D., Sophie Caillard, M.D., Jean Marc Constans, M.D., Serge Metanbou, M.D., Adrien Heintz, Ph.D., Julie Helms, M.D., Maleka Schenck, M.D., Nicolas Lefèbvre, M.D., Claire Boutet, M.D., Xavier Fabre, M.D., Géraud Forestier, M.D., Isaure de Beaurepaire, M.D., Grégoire Bornet, M.D., Audrey Lacalm, M.D., Hélène Oesterlé, M.D., Federico Bolognini, M.D., Julien Messie, M.D., Ghazi Hmeydia, M.D., Joseph Benzakoun, M.D., Catherine Oppenheim, M.D., Blanche Bapst, M.D., Imen Megdiche, M.D., Marie-Cécile Henri-Feugeas, M.D., Antoine Khalil, M.D., Augustin Gaudemer, M.D., Lavinia Jager, M.D., Patrick Nesser, M.D., Yannick Talla Mba, M.D., Céline Hemmert, M.D., Philippe Feuerstein, M.D., Nathan Sebag, M.D., Sophie Carré, M.D., Manel Alleg, M.D., Claire Lecocq, M.D., Emmanuelle Schmitt, M.D., René Anxionnat, M.D., François Zhu, M.D., Pierre-Olivier Comby, M.D., Frédéric Ricolfi, M.D., Pierre Thouant, M.D., Hubert Desal, M.D., Grégoire Boulouis, M.D., Jérome Berge, M.D., Apolline Kazémi, M.D., Nadya Pyatigorskaya, M.D., Augustin Lecler, M.D., Suzana Saleme, M.D., Myriam Edjlali-Goujon, M.D., Basile Kerleroux, M.D., Pierre-Emmanuel Zorn, Ph.D., Muriel Mathieu, Seyyid Baloglu, M.D., François-Daniel Ardellier, M.D., Thibault Willaume, M.D., Jean Christophe Brisset, Ph.D., Clotilde Boulay, M.D., Véronique Mutschler, M.D., Yves Hansmann, M.D., Paul-Michel Mertes, M.D., Francis Schneider, M.D., Samira Fafi-Kremer, Pharm.D., Mickael Ohana, M.D., Ferhat Meziani, M.D., Jean-Stéphane David, M.D., Nicolas Meyer, M.D., Mathieu Anheim, M.D., François Cotton, M.D.
Radiology is edited by David A. Bluemke, M.D., Ph.D., University of Wisconsin School of Medicine and Public Health, Madison, Wis., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on brain MRI, visit RadiologyInfo.org.
Press Resources:
Images (JPG, TIF):

Figure 1. Flowchart of patient inclusion and exclusion.
High-res (TIF) version
(Right-click and Save As)
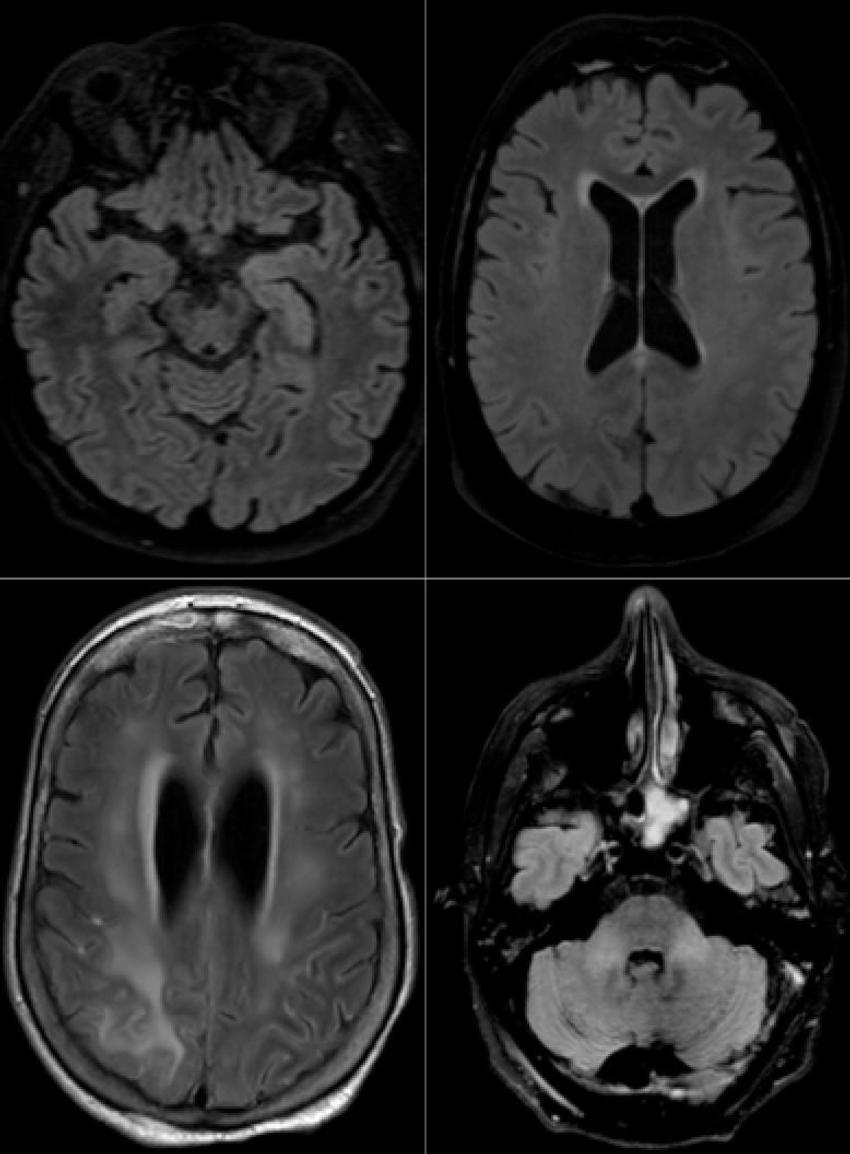
Figure 2. Axial FLAIR in four different COVID-19 patients. A) 58-year old man with impaired consciousness: FLAIR hyperintensities located in the left medial temporal lobe. B) 66-year old man with impaired consciousness: FLAIR ovoid hyperintense lesion located in the central part of the splenium of the corpus callosum. C) 71-year old woman with pathological wakefulness after sedation: extensive and confluent supratentorial white matter FLAIR hyperintensities. Association with leptomeningeal enhancement. D) 61-year old man with confusion: hyperintense lesions involving both middle cerebellar peduncles. FLAIR = Fluid-attenuated inversion recovery
High-res (TIF) version
(Right-click and Save As)
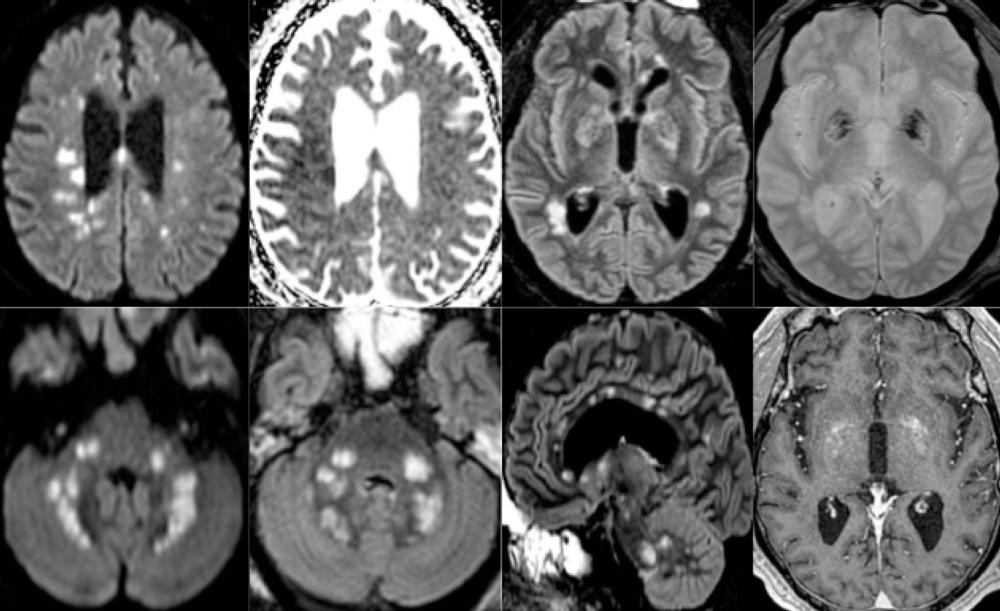
Figure 3. 65-year old man with pathological wakefulness after sedation. Non-confluent multifocal white matter hyperintense lesions on FLAIR and diffusion, with variable enhancement, and hemorrhagic lesions. Axial Diffusion (A, B), Apparent Diffusion Coefficient (ADC) map (C), axial FLAIR (D, E), sagittal FLAIR (F), axial Susceptibility weighted imaging (SWI) (G), and postcontrast T1 weighted MR images (H). Multiple nodular hyperintense Diffusion and FLAIR lesions localized in the white matter including the corpus callosum (F). Some of them are associated with reduced ADC corresponding to cytotoxic edema (C). Other lesions are located next to the lenticular nucleus (E, G, H), with hemorrhagic changes (G), and enhancement after contrast administration. FLAIR = Fluid-attenuated inversion recovery
High-res (TIF) version
(Right-click and Save As)
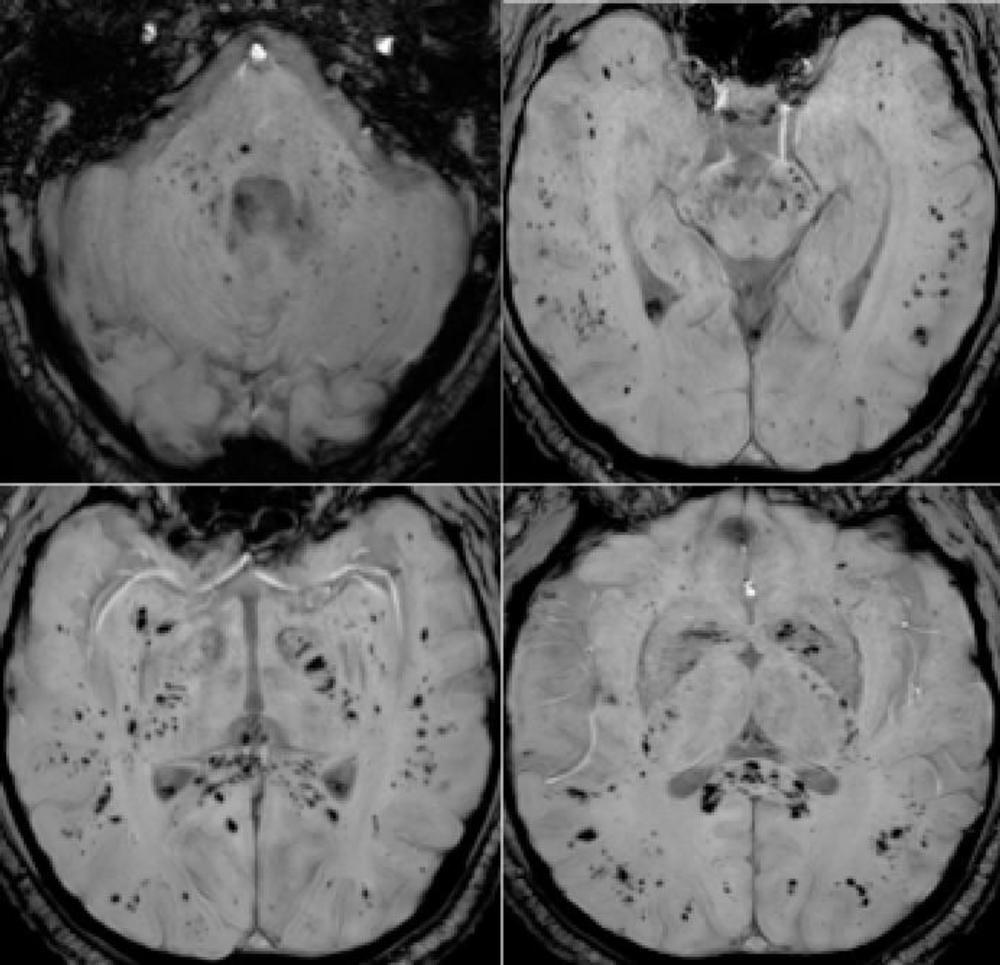
Figure 4. 57-year old man with pathological wakefulness after sedation. Extensive and isolated white matter microhemorrhages. Axial Susceptibility weighted imaging (SWI) (A, B, C, D): multiple microhemorrhages mainly affecting the subcortical white matter, corpus callosum, internal capsule, and cerebellar peduncles.
High-res (TIF) version
(Right-click and Save As)
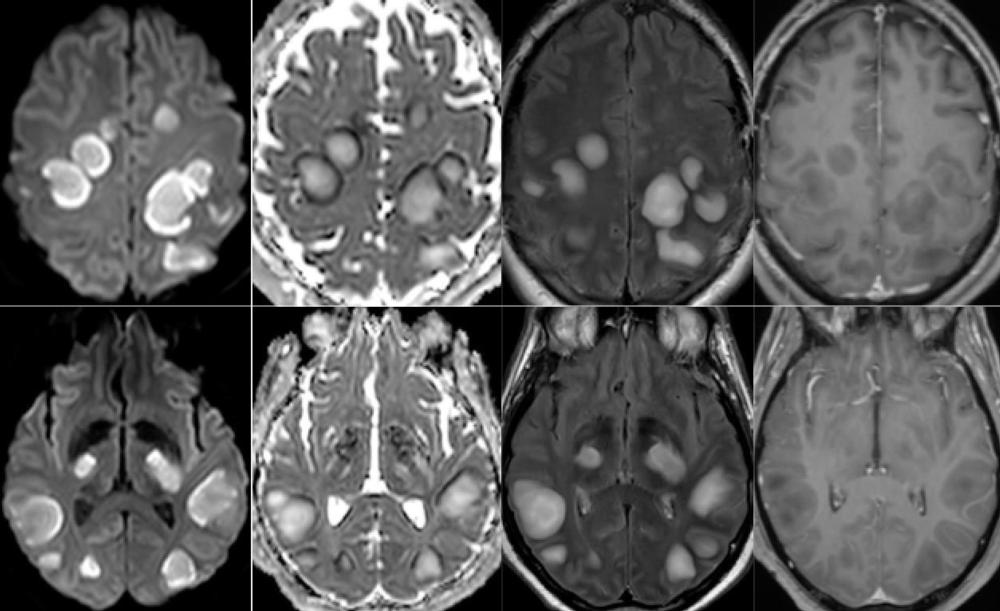
Figure 5. 54-year old man with pathological wakefulness after sedation. Non-confluent multifocal white matter hyperintense lesions on FLAIR and diffusion, with variable enhancement. Axial Diffusion (A, B), Apparent Diffusion Coefficient (ADC) map (C, D), axial postcontrast FLAIR (E, F), and postcontrast T1 weighted MR images (G, H). Multiple nodular hyperintense Diffusion and FLAIR subcortical and corticospinal tracts lesions, with very mild mass effect on adjacent structures. The lesions present a center with an elevation of ADC corresponding to vasogenic edema and a peripheral ring of reduced ADC corresponding to cytotoxic edema (C, D). After contrast administration, small areas of very mild enhancement are detected (G, H). FLAIR = Fluid-attenuated inversion recovery
High-res (TIF) version
(Right-click and Save As)
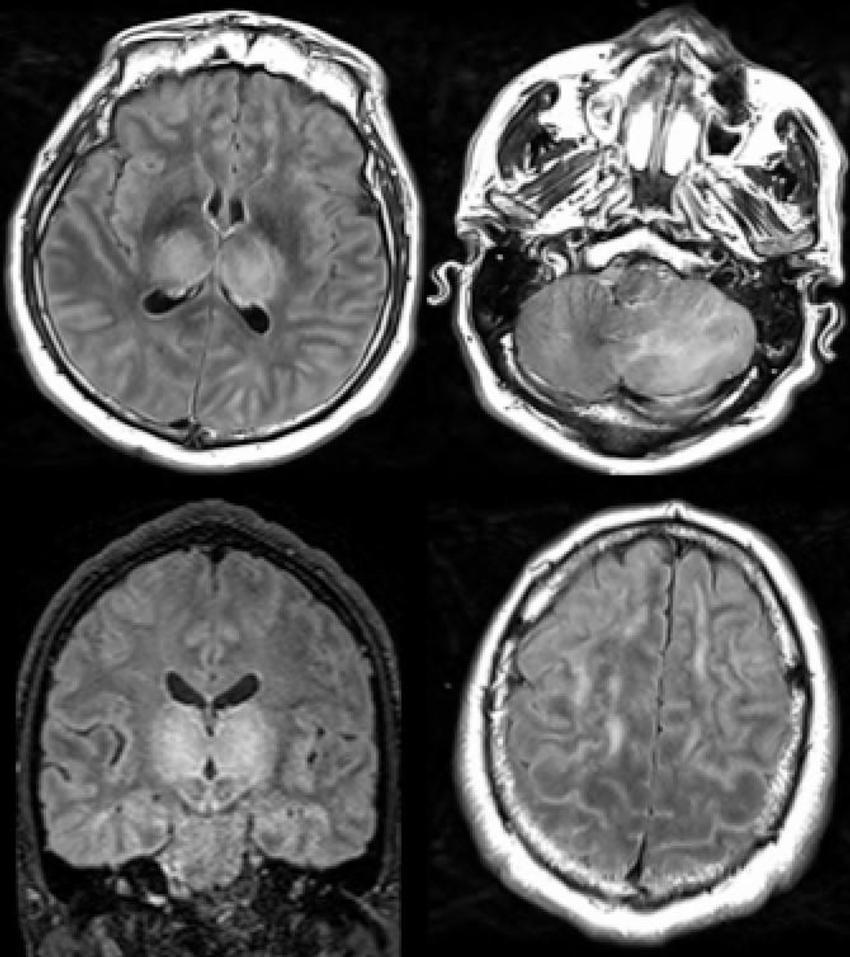
Figure 6. 51-year old man with impaired consciousness. Acute necrotizing encephalopathy. Axial FLAIR (A, C, D), and coronal FLAIR (B): bilateral FLAIR hyperintensity in both thalami (A, B), associated with involvement of the cerebellar (C), and cerebral (D) white matter. FLAIR = Fluid-attenuated inversion recovery
High-res (TIF) version
(Right-click and Save As)