Weight Loss Can Slow Down Knee Joint Degeneration
Released: May 02, 2017
At A Glance
- Overweight and obese patients who lose weight can slow down the progression of cartilage degeneration in the knee.
- Researchers investigated the association between weight loss and the progression of knee cartilage changes in 640 overweight and obese patients.
- Patients who had a decrease in BMI of more than 5 percent over 48 months had slower degeneration of their knee cartilage.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
OAK BROOK, Ill. — Overweight and obese people who lost a substantial amount of weight over a 48-month period showed significantly lower degeneration of their knee cartilage, according to a new study published online in the journal Radiology.
According to the National Institutes of Health, obesity is a risk factor for osteoarthritis. Being overweight or obese can place extra pressure on joints and cartilage, causing them to wear away. In addition, people with more body fat may have higher blood levels of substances that cause inflammation in the joints, raising the risk for osteoarthritis.
“For this research, we analyzed the differences between groups with and without weight loss,” said the study’s lead author, Alexandra Gersing, M.D., from the Department of Radiology and Biomedical Imaging at the University of California, San Francisco. “We looked at the degeneration of all knee joint structures, such as menisci, articular cartilage and bone marrow.”
The research team investigated the association between weight loss and the progression of cartilage changes on MRI over a 48-month period in 640 overweight and obese patients (minimum body mass index [BMI] 25 kg/m2) who had risk factors for osteoarthritis or MRI evidence of mild to moderate osteoarthritis. Data was collected from the Osteoarthritis Initiative, a nationwide research study focused on the prevention and treatment of knee osteoarthritis. Patients were categorized into three groups: those who lost more than 10 percent of their body weight, those who lost five to 10 percent of their body weight, and a control group whose weight remained stable.
The results showed that patients with 5 percent weight loss had lower rates of cartilage degeneration when compared with stable weight participants. In those with 10 percent weight loss, cartilage degeneration slowed even more.
Not only did the researchers find that weight loss slowed articular cartilage degeneration, they also saw changes in the menisci. Menisci are crescent-shaped fibrocartilage pads that protect and cushion the joint.
“The most exciting finding of our research was that not only did we see slower degeneration in the articular cartilage, we saw that the menisci degenerated a lot slower in overweight and obese individuals who lost more than 5 percent of their body weight, and that the effects were strongest in overweight individuals and in individuals with substantial weight loss,” Dr. Gersing said.
Light to moderate exercise is also recommended to protect against cartilage degeneration in the knee.
“Our study emphasizes the importance of individualized therapy strategies and lifestyle interventions in order to prevent structural knee joint degeneration as early as possible in obese and overweight patients at risk for osteoarthritis or with symptomatic osteoarthritis,” Dr. Gersing said.
“Is Weight Loss Associated with Less Progression of Changes in Knee Articular Cartilage among Obese and Overweight Patients as Assessed with MR Imaging over 48 Months? Data from the Osteoarthritis Initiative.” Collaborating with Dr. Gersing were Benedikt J. Schwaiger, M.D., Michael C. Nevitt, M.D., Gabby B. Joseph, Ph.D., Nattagan Chanchek, M.D., Julio B. Guimaraes, M.D., John Mbapte Wamba, M.D., Luca Facchetti, M.D., Charles E. McCulloch, Ph.D., and Thomas M. Link, M.D. Ph.D.
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of over 54,600 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on musculoskeletal MRI, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
and Video clips (.mp4 format)
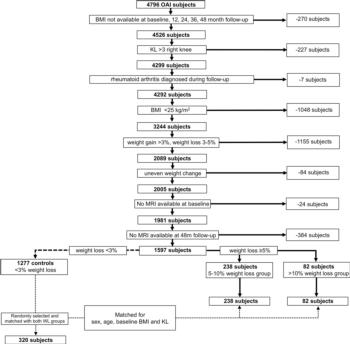
Figure 1. Flowchart shows participant selection from Osteoarthritis Initiative database. KL = Kellgren-Lawrence score.
High-res (TIF) version
(Right-click and Save As)
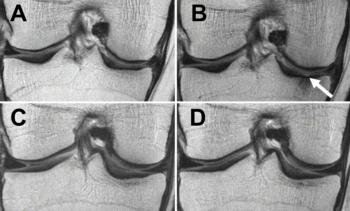
Figure 2. MRIs of the right knee obtained with the coronal proton density–weighted fast spin-echo fat-suppression sequence at, A, C, baseline and, B, D, after 48 months. Patients were an obese 65-year-old woman with stable weight and mild knee pain (Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain subscale score of 3 at baseline; baseline BMI, 33.1 kg/m2) (A and B) and an obese 64-year-old woman with weight loss over 48 months and mild knee pain (approximately 10.9 percent decrease in BMI; WOMAC pain subscale score of 5 at baseline; baseline BMI, 33.7 kg/m2) (C and D). The woman with stable weight developed a full-thickness focal cartilage defect at the medial tibia (arrow) (baseline cartilage Whole-Organ Magnetic Resonance Imaging Score (WORMS) grade 0 in A and 2.5 in B). In contrast, no cartilage defects were detected at baseline or 48-month follow-up in the woman with weight loss (cartilage WORMS grade 0 in C and D).
High-res (TIF) version
(Right-click and Save As)
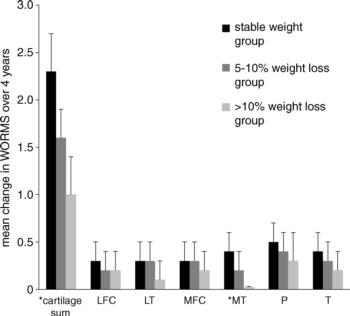
Figure 3. Mean change in Whole-Organ Magnetic Resonance Imaging Score (± standard error of the mean) over 4 years in the groups with stable weight, 5 percent–10 percent weight loss, and more than 10 percent weight loss in the subgroups. Cartilage sum = sum of all compartments; LFC = lateral femoral condyle; LT = lateral tibia; MFC = medial femoral condyle; MT = medial tibia; P = patella; T = trochlea. * indicates significant differences between the groups after logistic regression analysis (P < .017).
High-res (TIF) version
(Right-click and Save As)
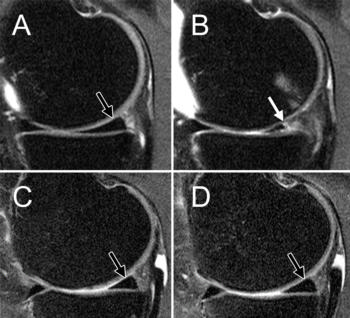
Figure 4. MRIs of the right knee obtained with sagittal intermediate-weighted fast spin-echo fat-suppression sequence at, A, C, baseline and, B, C, after 48 months. Patients were an obese 57-year-old woman with stable weight and mild knee pain (Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain subscale score of 5 at baseline; baseline BMI, 31.4 kg/m2) (A, B) and an obese 59-year-old woman with weight loss (approximately 8.5 percent decrease in BMI) over 48 months and mild knee pain (WOMAC pain subscale score of 6 at baseline; baseline BMI, 32.1 kg/ m2) (C, D). The woman with stable weight developed a maceration of the medial meniscus (arrow) (medial meniscus Whole-Organ Magnetic Resonance Imaging Score (WORMS) of grade 0 in A and grade 4 in B) and thinning of the cartilage of the medial femoral condyle. In contrast, no meniscal defects (arrows) were seen on C or D (medial meniscus WORMS grade 0) in the participant with weight loss.
High-res (TIF) version
(Right-click and Save As)
