Researchers Generate 3-D Virtual Reality Models of Unborn Babies
Released: November 21, 2016
At A Glance
- New technology transforms MRI and ultrasound data into a 3-D virtual reality model of a fetus.
- The fetal models are remarkably similar to the postnatal appearance of the newborn baby, and recreate the whole internal structure of the fetus.
- Wearing a virtual reality headset, users can hear the baby’s heartbeat and, by moving their head, study the baby’s anatomy.
- RSNA Media Relations
1-630-590-7762
media@rsna.org - Maureen Morley
1-630-590-7754
mmorley@rsna.org - Linda Brooks
1-630-590-7738
lbrooks@rsna.org
CHICAGO — Parents may soon be able to watch their unborn babies grow in realistic 3-D immersive visualizations, thanks to new technology that transforms MRI and ultrasound data into a 3-D virtual reality model of a fetus, according to research being presented next week at the annual meeting of the Radiological Society of North America (RSNA).
MRI provides high-resolution fetal and placental imaging with excellent contrast. It is generally used in fetal evaluation when ultrasound cannot provide sufficiently high-quality images.
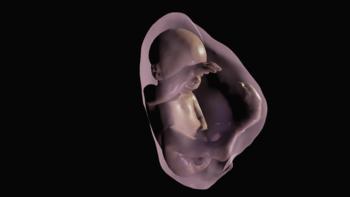
Researchers in Brazil created virtual reality 3-D models based on fetal MRI results. Sequentially-mounted MRI slices are used to begin construction of the model. A segmentation process follows in which the physician selects the body parts to be reconstructed in 3-D. Once an accurate 3-D model is created—including the womb, umbilical cord, placenta and fetus—the virtual reality device can be programmed to incorporate the model.
"The 3-D fetal models combined with virtual reality immersive technologies may improve our understanding of fetal anatomical characteristics and can be used for educational purposes and as a method for parents to visualize their unborn baby," said study co-author Heron Werner Jr., M.D., Ph.D., from the Clínica de Diagnóstico por Imagem, in Rio de Janeiro, Brazil.
The virtual reality fetal 3-D models are remarkably similar to the postnatal appearance of the newborn baby. They recreate the entire internal structure of the fetus, including a detailed view of the respiratory tract, which can aid doctors in assessing abnormalities.
For the virtual reality device, Dr. Werner and colleagues used the latest-generation Oculus Rift 2 headset. Oculus Rift 2 places the user in an immersive environment, complete with heartbeat sounds derived from the ultrasound of the fetus. Users can study the 3-D fetal anatomy simply by moving their head.
"The experience with the Oculus Rift has been wonderful," Dr. Werner said. "It provides fetal images that are sharper and clearer than ultrasound and MR images viewed on a traditional display."
The technology has numerous potential applications, including assessment of fetal airway patency. Airway patency, or the state of airways being open and unblocked, is an important issue for a developing fetus. For example, if ultrasound showed an abnormal mass near the fetal airway, physicians could use the 3-D images and the headset to assess the entire length of the airway and make better informed decisions about delivery.
The technology also can help coordinate care with multidisciplinary teams and provide better visual information to parents to help them understand malformations and treatment decisions.
"The physicians can have access to an immersive experience on the clinical case that they are working on, having the whole internal structure of the fetus in 3-D in order to better visualize and share the morphological information," Dr. Werner said. "We believe that these images will help facilitate a multidisciplinary discussion about some pathologies in addition to bringing a new experience for parents when following the development of their unborn child."
The researchers have used the technique on patients at a clinic in Rio de Janeiro, including cases where the fetus had evidence of an abnormality that required postnatal surgery. They hope to use the technology more broadly over the next year.
Co-authors on the study are Bianca Guedes Ribeiro, M.D., Jorge Lopes, Ph.D., Gerson Ribeiro, Pedro Daltro, M.D., Tatiana M. Fazecas, M.D., Renata A. Nogueira, M.D., and Leise Rodrigues, M.D.
Note: Copies of RSNA 2016 news releases and electronic images will be available online at RSNA.org/press16 beginning Monday, Nov. 28.
RSNA is an association of more than 54,000 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Ill. (RSNA.org)
Editor's note: The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA Newsroom at 1-312-791-6610.
For patient-friendly information on obstetric ultrasound and MRI, visit RadiologyInfo.org.
Images (.JPG and .TIF format)
and Video clips (.mp4 format)
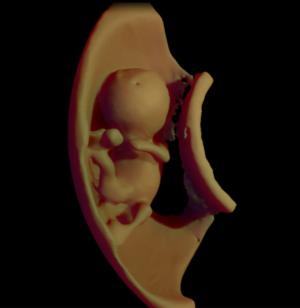
Figure 1. 3D virtual model ultrasound view of fetus at 12 weeks
High-res (TIF) version
(Right-click and Save As)
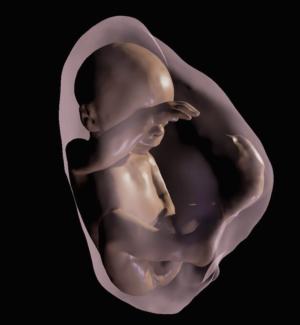
Figure 2. 3D virtual model MRI view of fetus at 26 weeks
High-res (TIF) version
(Right-click and Save As)

Figure 4. Still from fly-through of internal structures at 26 weeks
High-res (TIF) version
(Right-click and Save As)
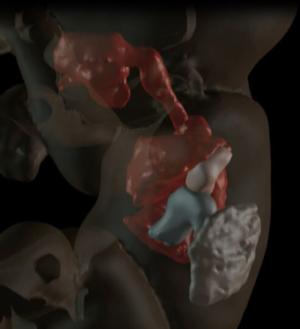
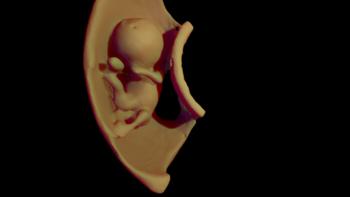
Figure 5. Visualization of internal structures at 27 weeks
High-res (TIF) version
(Right-click and Save As)
Video 1. 3D model of the fetus (12 weeks) generated from ultrasound files segmented in order to build the 3D virtual reality.
Download.mp4
(Right-click and Save As)
Video 2. 3D model of the fetus (26 weeks) generated from magnetic resonance imaging files segmented in order to build the 3D virtual reality.
Download.mp4
(Right-click and Save As)

Video 3. 3D model navigation in a fetus (27 weeks) with left congenital diaphragmatic hernia submitted to Fetoscopic Endotracheal Balloon (FETO). Note the yellow-colored balloon.
Download.mp4
(Right-click and Save As)

Video 4. Heron Werner Jr., M.D., Ph.D., describes the findings of his study.
Download.mp4
(Right-click and Save As)

Video 5. Heron Werner Jr., M.D., Ph.D., describes how this technology affects parental bonding.
Download.mp4
(Right-click and Save As)

